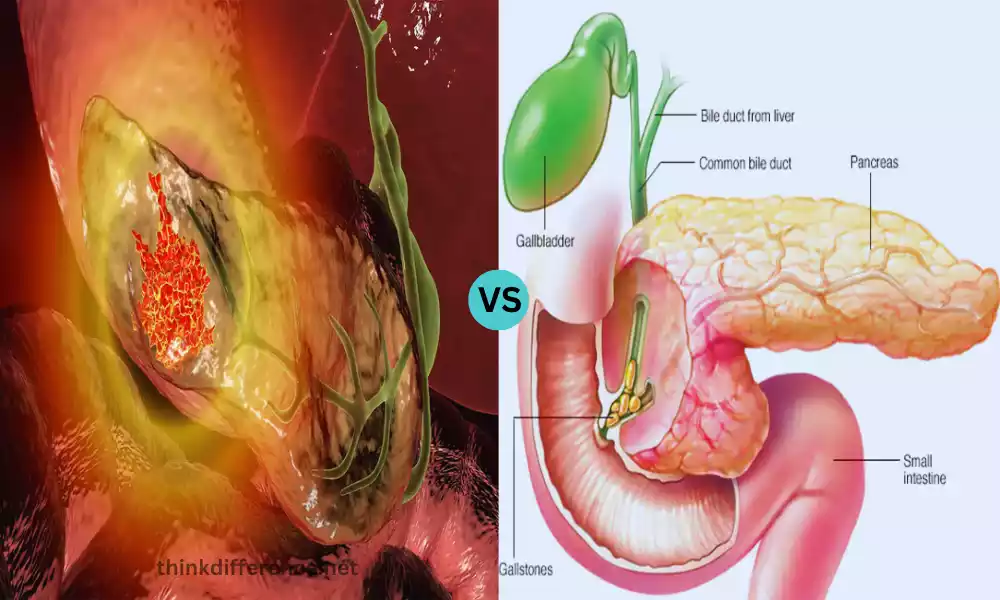
Pancreatic Cancer and Pancreatitis are two distinct but significant medical conditions that affect the pancreas, an essential organ in the human body. Pancreatic cancer involves the abnormal growth of malignant cells within the pancreas, while pancreatitis is characterized by inflammation of the pancreas often triggered by factors like alcohol consumption or gallstones. Both conditions can have serious implications for health, making understanding their differences crucial for timely diagnosis and appropriate management.
Pancreatic Cancer
Definition of Pancreatic Cancer
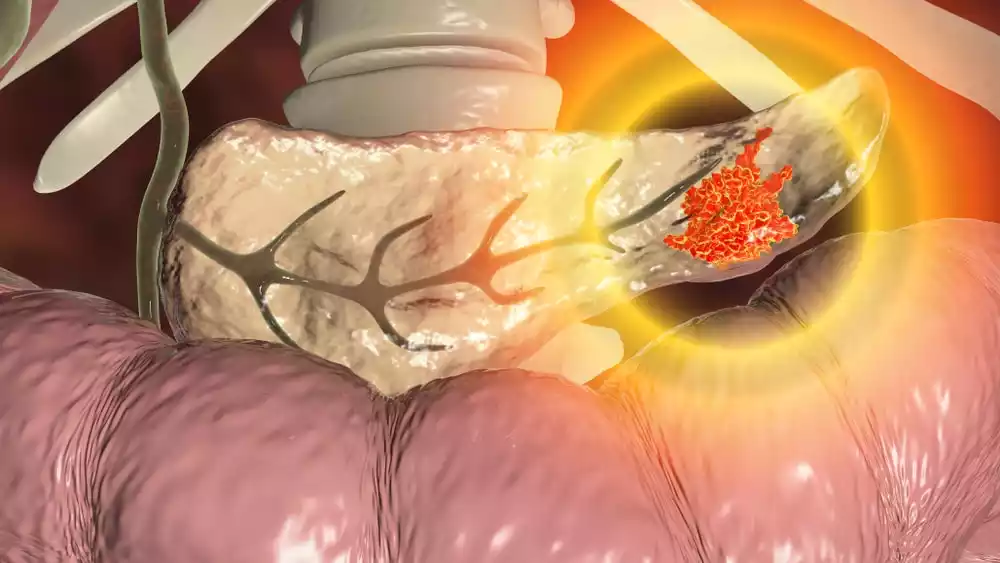
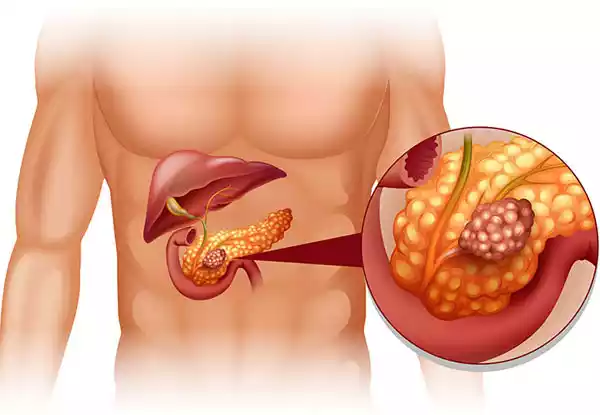
Pancreatic cancer is a malignant neoplasm that originates in the cells of the pancreas, a vital organ located behind the stomach. This aggressive form of cancer occurs when cells in the pancreas begin to grow uncontrollably, forming tumors that can interfere with the normal functioning of the pancreas and potentially spread to other parts of the body.
Pancreatic cancer is known for its high mortality rate, often due to its late-stage diagnosis and the aggressive nature of the disease. It can manifest in different types, such as exocrine pancreatic cancer (which affects the cells responsible for producing digestive enzymes) and less common endocrine pancreatic cancer (which affects the hormone-producing cells of the pancreas).
Types of Pancreatic Cancer
Here’s a concise overview of the main types of pancreatic cancer:
- Exocrine Pancreatic Cancer:
- Pancreatic Ductal Adenocarcinoma (PDAC): The most common type, originating in ductal cells. Aggressive and tends to spread early.
- Adenosquamous Carcinoma: Contains both glandular and squamous components. Rare but aggressive.
- Undifferentiated Carcinoma: Poorly differentiated cells with a poorer prognosis.
- Endocrine Pancreatic Cancer (Pancreatic Neuroendocrine Tumors or PNETs):
- Insulinoma: Produces insulin, causing low blood sugar.
- Glucagonoma: Produces glucagon, raising blood sugar.
- Gastrinoma: Produces gastrin, leading to excess stomach acid.
- Somatostatinoma: Produces somatostatin, regulating other hormones.
- VIPoma: Produces VIP, causing severe diarrhea and imbalances.
- Non-Functioning PNETs: Doesn’t produce significant hormones; may cause symptoms as they grow.
These types have distinct characteristics and behaviors, impacting diagnosis and treatment approaches.
Risk Factors of Pancreatic Cancer
Here are the key risk factors associated with pancreatic cancer:
- Age: As one ages, their risk for pancreatic cancer increases exponentially – most cases occurring among those over 65.
- Smoking: Smoking tobacco is a significant risk factor, as it can double or even triple the risk of developing pancreatic cancer.
- Family History: Having a close family member (parent, sibling, or child) who has had pancreatic cancer increases your risk, suggesting a potential genetic component.
- Inherited Gene Mutations: Certain inherited gene mutations, such as mutations in the BRCA1, BRCA2, PALB2, or p16 genes, can elevate the risk of pancreatic cancer.
- Chronic Pancreatitis: Long-term inflammation of the pancreas, often due to excessive alcohol consumption or other causes, can increase the risk of developing pancreatic cancer.
- Diabetes: Individuals with long-standing diabetes have a slightly higher risk of developing pancreatic cancer. The connection between pancreatic cancer and diabetes remains complex and unfathomable for most.
- Obesity: Being overweight or obese increases the risk of pancreatic cancer, possibly due to the associated metabolic changes.
- Diet: A diet high in red meat, processed meat, and saturated fats and low in fruits and vegetables may contribute to an increased risk.
- Heavy Alcohol Consumption: While the relationship is not fully established, heavy and prolonged alcohol consumption may elevate the risk of pancreatic cancer.
- Workplace Exposure: Certain chemicals, such as those used in dry cleaning and metalworking, might be linked to an increased risk.
- Gender: Men are less likely to develop pancreatic cancer than females.
- Race and Ethnicity: African Americans are at a slightly higher risk compared to Asians, Hispanics, and whites.
It’s important to note that having one or more of these risk factors doesn’t necessarily mean someone will develop pancreatic cancer. Conversely, some individuals without obvious risk factors may still be diagnosed with the disease. If you have concerns about your risk, it’s a good idea to discuss them with a healthcare professional.
How is pancreatic cancer diagnosis?
Diagnosing pancreatic cancer involves:
- Medical History and Physical Exam: Discussing symptoms, risk factors, and medical history.
- Imaging Tests:
- CT Scan: Detailed cross-sectional images of the pancreas and surrounding areas.
- MRI: Detailed images using magnets and radio waves.
- Endoscopic Ultrasound (EUS): Inserting an ultrasound probe through the digestive tract to visualize the pancreas.
- PET-CT: Highlighting abnormal cell activity and spread.
- Biopsy: Collecting tissue samples for examination using methods like FNA or biopsy during endoscopy.
- Blood Tests:
- Tumor Markers: Measuring substances like CA19-9 produced by tumors.
- Liver Function Tests: Assessing liver health affected by cancer.
A multidisciplinary team reviews results to confirm diagnosis and plan treatment. Early detection is crucial for effective management.
Pancreatitis
Definition of Pancreatitis
Pancreatitis refers to the inflammation of the pancreas, an organ located behind the stomach that plays a crucial role in digestion and regulating blood sugar levels. This inflammation can occur suddenly (acute pancreatitis) or develop over a longer period (chronic pancreatitis).
Acute pancreatitis is often characterized by a sudden and severe onset of symptoms, which can include intense abdominal pain, nausea, vomiting, and fever. It can be caused by various factors such as gallstones, heavy alcohol consumption, certain medications, infections, and high levels of triglycerides in the blood.
Chronic pancreatitis, on the other hand, involves ongoing inflammation that can lead to permanent damage to the pancreas over time. This can result in persistent abdominal pain, digestive problems, and potential complications like diabetes due to the disruption of insulin production.
Both forms of pancreatitis can range in severity from mild to severe and can require medical intervention, including pain management, dietary changes, and, in more severe cases, hospitalization.
Causes of Pancreatitis
Pancreatitis can be caused by various factors, with some common triggers and underlying causes. Here are the main causes of pancreatitis:
- Gallstones: One of the leading causes of acute pancreatitis is gallstones that block the pancreatic duct, preventing enzymes from flowing properly and leading to inflammation.
- Heavy Alcohol Consumption: Chronic alcohol abuse can trigger chronic pancreatitis. It’s believed that alcohol causes direct damage to the pancreas and affects enzyme secretion.
- Trauma or Injury: Physical trauma, such as a blow to the abdomen, can lead to pancreatitis.
- Certain Medications: Some medications, especially those that affect triglyceride levels or have a toxic effect on the pancreas, can contribute to pancreatitis.
- High Triglyceride Levels: Elevated levels of triglycerides (a type of fat) in the blood can increase the risk of pancreatitis.
- Infections: Infections like mumps or viral hepatitis can cause pancreatitis, although this is relatively rare.
- ERCP (Endoscopic Retrograde Cholangiopancreatography): This medical procedure, used to treat gallstones, can sometimes lead to pancreatitis as a complication.
- Autoimmune Pancreatitis: In some cases, the body’s immune system mistakenly attacks the pancreas, leading to inflammation.
- Genetic Factors: Certain genetic conditions, such as hereditary pancreatitis, can increase the risk of developing the disease.
- Cystic Fibrosis: This genetic disorder can affect the function of various organs, including the pancreas.
- Hypercalcemia: Elevated levels of calcium in the blood can trigger inflammation of the pancreas.
- Hyperlipidemia: High levels of fats in the blood can contribute to pancreatitis.
- Pancreatic Cancer: Rarely, pancreatic cancer can cause inflammation of the pancreas.
It’s important to note that acute pancreatitis and chronic pancreatitis have different causes and risk factors. Acute pancreatitis is often linked to sudden triggers like gallstones and alcohol, while chronic pancreatitis is more often associated with long-term alcohol abuse or underlying conditions. If you experience symptoms of pancreatitis, seek medical attention promptly for proper diagnosis and treatment.
Symptoms of Pancreatitis
The symptoms of pancreatitis can vary in severity and presentation, depending on whether it’s acute or chronic pancreatitis. Here are the common symptoms associated with both forms:
Acute Pancreatitis:
- Sudden and Severe Abdominal Pain: The hallmark symptom. The pain is often located in the upper abdomen and can radiate to the back. It can be intense and persistent.
- Nausea and Vomiting: Nausea is common, and vomiting might provide temporary relief from the pain.
- Fever: A mild to high fever can accompany acute pancreatitis.
- Tenderness: The abdomen might be tender to touch.
- Increased Heart Rate: Heart rate may be elevated due to inflammation.
- Jaundice: In severe cases, yellowing of the skin and eyes can occur if the bile duct becomes blocked.
Chronic Pancreatitis:
- Abdominal Pain: The pain tends to be persistent and can be dull, steady, or intermittent. It might worsen after eating or drinking alcohol.
- Weight Loss: Chronic pancreatitis can lead to malabsorption of nutrients, resulting in weight loss.
- Digestive Issues: Frequent oily, foul-smelling stools (steatorrhea) and difficulty digesting fatty foods due to decreased enzyme production.
- Nausea and Vomiting: These symptoms might be more prominent in chronic cases.
- Diabetes: Over time, chronic pancreatitis can affect insulin production, leading to diabetes.
It’s important to note that the severity of symptoms can vary widely, and some individuals might experience only a subset of these symptoms. If you suspect pancreatitis, especially if you experience severe abdominal pain, seek medical attention promptly. Pancreatitis requires proper diagnosis and management to prevent complications and promote recovery.
How is Pancreatitis diagnosis?
Diagnosing pancreatitis involves:
- Medical History and Physical Exam: Discussing symptoms, risk factors, and physical evaluation.
- Blood Tests: Measuring amylase and lipase levels, and liver function tests.
- Imaging: Using ultrasound, CT scan, or MRI to visualize the pancreas and surrounding areas.
- Stool Tests: Assessing fat malabsorption in chronic cases.
- Biopsy: Collecting tissue samples using FNA or ERCP biopsy if needed.
- Additional Tests: Depending on the situation, genetic testing or special scans might be used.
A doctor will analyze results to confirm the diagnosis and determine appropriate treatment.
Comparison Table of Pancreatitis and Pancreatic Cancer
Here’s a concise comparison table between pancreatitis and pancreatic cancer:
| Aspect | Pancreatitis | Pancreatic Cancer |
|---|---|---|
| Definition | Inflammation of the pancreas | Malignant growth in the pancreas |
| Causes | Gallstones, alcohol, infections, medications | Genetic mutations, smoking, family history |
| Onset | Sudden (acute) or long-term (chronic) | Gradual development over time |
| Symptoms | Acute pain, nausea, vomiting, fever, tenderness | Abdominal pain, weight loss, jaundice, digestive issues |
| Duration of Symptoms | Can improve with treatment (acute) | Persist and worsen (chronic) |
| Diagnostic Tests | Blood tests (enzyme levels), imaging (ultrasound, CT), possibly biopsy | Blood tests (tumor markers), imaging (CT, MRI), biopsy |
| Management | Treatment and lifestyle changes for acute, potential long-term management for chronic | Depends on cancer stage, treatment options vary |
| Prognosis | Favorable for acute cases with timely intervention | Generally more serious due to late-stage diagnosis |
| Risk Factors | Gallstones, alcohol, infections, medications | Genetic mutations, smoking, family history, age |
| Prevalence | Relatively common | Less common but often diagnosed at advanced stages |
Remember that this table provides a simplified comparison. For accurate diagnosis, treatment, and management, consulting a healthcare professional is essential.
Treatment Approaches for Pancreatic Cancer and pancreatitis
Pancreatic Cancer
Here’s an overview of the treatment approaches for pancreatic cancer:
- Surgery:
- Whipple Procedure (Pancreaticoduodenectomy): This complex surgery involves removing the head of the pancreas, part of the small intestine, gallbladder, and bile duct. It’s used for tumors in the head of the pancreas.
- Distal Pancreatectomy: Removes the tail and sometimes part of the body of the pancreas. Used for tumors in the body or tail of the pancreas.
- Total Pancreatectomy: Removes the entire pancreas. Rarely performed and usually reserved for extensive cases.
- Chemotherapy:
- Neoadjuvant Chemotherapy: Administered before surgery to shrink tumors and improve the chances of successful surgery.
- Adjuvant Chemotherapy: Given after surgery to eliminate any remaining cancer cells and reduce the risk of recurrence.
- Palliative Chemotherapy: Used for advanced cases to alleviate symptoms and slow the cancer’s progression.
- Radiation Therapy:
- Adjuvant Radiation Therapy: Given after surgery to destroy any remaining cancer cells.
- Palliative Radiation Therapy: Used to relieve pain and other symptoms in advanced cases.
- Targeted Therapy:
- Targeted Drugs: Target specific molecules involved in the growth and spread of cancer cells.
- PARP Inhibitors: Used for certain inherited genetic mutations.
- Immunotherapy:
- Immune Checkpoint Inhibitors: Increase the body’s immune system against cancerous cells.
- CAR T-cell Therapy: Experimental approach involving modified immune cells.
- Clinical Trials:
- Participation in research studies testing new treatments or combinations.
- Palliative Care:
- Focuses on symptom management, pain relief, and improving quality of life for advanced-stage patients.
Treatment plans are tailored to the patient’s individual case, including the stage of cancer, overall health, and specific characteristics of the tumor. A multidisciplinary team of oncologists, surgeons, radiologists, and other specialists collaborates to determine the most effective treatment approach.
Pancreatitis
Here’s an overview of the treatment approaches for pancreatitis:
- Acute Pancreatitis:
- Hospitalization: Severe cases may require hospitalization for close monitoring, intravenous fluids, and pain management.
- Pain Management: Medications such as analgesics or anti-inflammatory drugs are used to alleviate abdominal pain.
- NPO (Nothing by Mouth): Initially, patients may need to abstain from eating to allow the pancreas to rest and heal.
- IV Nutrition: In severe cases, where eating is not possible, intravenous nutrition might be provided.
- Addressing Underlying Causes: Treating gallstones, infections, or other triggers that led to pancreatitis.
- Surgery: In rare cases, surgery might be needed to remove damaged tissue or treat complications.
- Chronic Pancreatitis:
- Pain Management: Pain relievers, anti-inflammatory drugs, or enzyme supplements can help manage pain.
- Dietary Modifications: Adjusting the diet to ease digestion and reduce strain on the pancreas, including low-fat meals and smaller portions.
- Enzyme Replacement Therapy: Providing enzyme supplements to aid digestion and prevent malabsorption.
- Lifestyle Changes: Limiting alcohol consumption and managing weight to reduce stress on the pancreas.
- Treating Complications: Addressing complications like pseudocysts or bile duct obstructions if they arise.
- Severe Cases and Complications:
- ERCP (Endoscopic Retrograde Cholangiopancreatography): Used to remove gallstones causing blockages or place stents in the bile ducts.
- Surgery: In cases of severe pain or complications, surgical interventions might be considered, such as drainage of pseudocysts or surgical removal of damaged tissue.
- Prevention:
- Lifestyle Changes: Avoiding heavy alcohol consumption and maintaining a healthy weight.
- Treating Underlying Conditions: Managing conditions like high triglycerides or autoimmune disorders that could trigger pancreatitis.
- Regular Follow-up: Monitoring and managing the condition to prevent flare-ups and complications.
Treatment plans are individualized based on the type of pancreatitis, its severity, and the patient’s overall health. Consultation with a healthcare provider is essential to determine the most suitable treatment approach.
The Role of Diet in Pancreatic Health
Diet plays a crucial role in maintaining pancreatic health:
- Pancreatitis Prevention: Opt for a low-fat diet, balanced nutrition, and smaller, frequent meals. Limit alcohol and stay hydrated.
- Pancreatic Cancer Risk: Choose fruits, vegetables, lean proteins, and whole grains to reduce cancer risk.
- Blood Sugar Control: Opt for low glycemic index foods to regulate blood sugar levels.
- Avoid Risk Factors: Limit processed foods, moderate sugar intake, and maintain a healthy weight.
- Hydration: Stay well-hydrated to support digestion and prevent gallstones.
- Consult Professionals: Follow medical advice and consult dietitians for personalized guidance.
Support and Care for Patients
Support and care for patients with pancreatic health conditions involve:
- Comprehensive Team: Multidisciplinary medical team coordination.
- Education: Clear information about conditions and treatments.
- Emotional Support: Counseling and support groups.
- Nutritional Guidance: Tailored dietary plans for symptom management.
- Pain Management: Effective strategies for pain relief.
- Palliative Care: Focus on symptom relief and quality of life.
- Clinical Trials: Access to cutting-edge treatments.
- Caregiver Support: Resources for caregivers’ challenges.
- Communication: Open dialogue and shared decision-making.
- Financial Assistance: Information on financial support.
- Survivorship Care: Monitoring health after treatment.
- End-of-Life Care: Resources for end-of-life planning.
Personalized care addressing physical, emotional, and practical needs is vital for patient well-being.
Recent Advances in Research and Treatment
As of my last update in September 2021, here are some recent advances in research and treatment for pancreatic health, including pancreatitis and pancreatic cancer. Please developments beyond this date are not covered:
Pancreatitis:
- Genetic Insights: Advances in genetic research have provided insights into the genetic factors contributing to pancreatitis. This understanding may lead to personalized treatments targeting specific genetic mutations.
- Biologic Therapies: Emerging research explores the potential of biologic therapies that target specific inflammatory pathways to manage and treat pancreatitis.
- Minimally Invasive Techniques: Advancements in endoscopic procedures allow for the removal of gallstones or the placement of stents to manage complications without the need for traditional surgery.
- Nutritional Interventions: Research is focusing on tailoring dietary interventions to manage symptoms and promote healing in acute and chronic pancreatitis.
Pancreatic Cancer:
- Immunotherapy: Immunotherapies like immune checkpoint inhibitors are being explored to stimulate the body’s immune system to recognize and attack pancreatic cancer cells.
- Targeted Therapies: Research is identifying specific genetic mutations that drive pancreatic cancer, leading to the development of targeted therapies aimed at inhibiting these mutations.
- Early Detection: Advances in liquid biopsies and biomarker research aim to improve early detection of pancreatic cancer when treatment options are more effective.
- Combination Therapies: Clinical trials are investigating combinations of chemotherapy, radiation, targeted therapies, and immunotherapies to enhance treatment efficacy.
- Precision Medicine: Personalized treatment approaches are being developed based on the unique genetic and molecular characteristics of individual patients’ tumors.
- Surgical Techniques: Innovations in surgical techniques, such as robotic-assisted surgery, are improving the precision and outcomes of surgeries for pancreatic cancer.
- Palliative Care: Enhanced palliative care approaches are being integrated to improve the quality of life and symptom management for advanced pancreatic cancer patients.
Remember that these are just a few examples of recent advances, and the field of medical research is constantly evolving. To get the most current information, I recommend consulting medical literature, research institutions, and healthcare professionals.
Summary
Pancreatitis and Pancreatic cancer are significant health concerns that require awareness and proactive healthcare measures. By understanding the signs, symptoms, risk factors, and treatments options for an illness, patients can better prepare themselves.