Aphthous Ulcers and Herpetic Ulcers are two distinct types of oral lesions that can cause discomfort and pain. While both may appear similar at first glance, they are fundamentally different in terms of their causes, contagiousness, appearance, and treatment. Understanding these distinctions is vital in providing accurate diagnosis and efficient management. We will delve into the characteristics of aphthous ulcers and herpetic ulcers, shedding light on what sets them apart.
Aphthous Ulcers
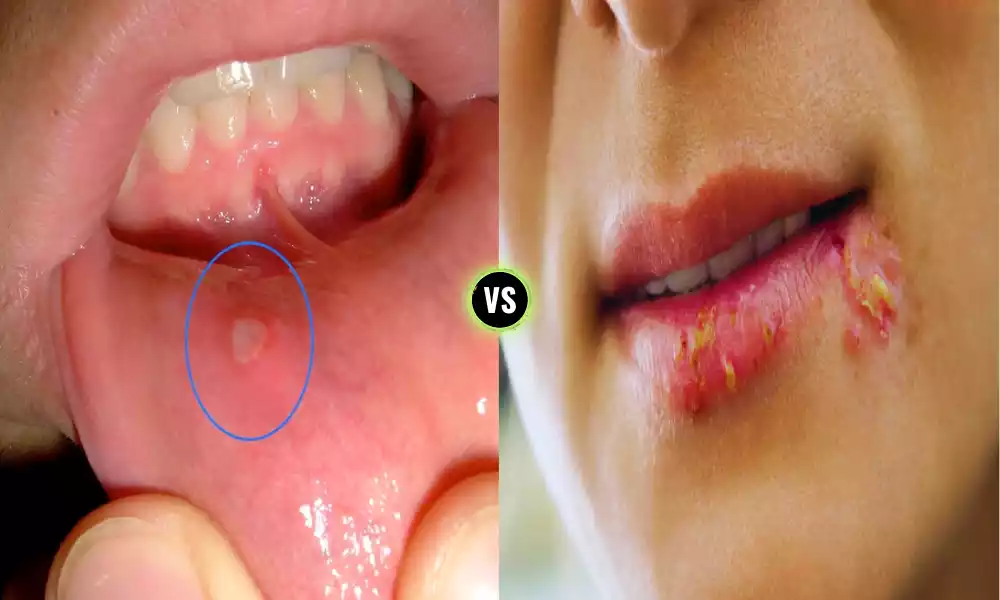
Aphthous ulcers, commonly known as canker sores, are painful and non-contagious lesions that develop on the mucous membranes inside the mouth. These ulcers are typically small, round, or oval-shaped, and have a white or yellow center surrounded by a red border. They can occur on the tongue, inner cheeks, gums, soft palate, or the back of the throat.

Aphthous ulcers are characterized by their recurrent nature, causing discomfort and making activities like eating, drinking, and speaking painful. While their exact cause is not fully understood, they are believed to be related to immune system dysfunction and various triggering factors. These ulcers usually heal on their own within 1-2 weeks, but various treatments can be employed to alleviate pain and promote faster healing.
Causes of Aphthous Ulcers
The exact cause of aphthous ulcers, also known as canker sores, is not fully understood, and they can occur spontaneously in many individuals. Several factors and triggers are believed to contribute to their development.
Common causes and contributing factors include:
-
- Immune System Dysfunction: There is evidence to suggest that aphthous ulcers may be related to an abnormal immune response. The immune system may mistakenly target and damage the mucous membranes inside the mouth, leading to the formation of ulcers.
- Genetics: There may be a genetic predisposition to developing aphthous ulcers. Individuals with a family history of canker sores are more likely to experience them.
- Trauma: Minor oral trauma or injury, such as accidental biting of the cheek or tongue, aggressive tooth brushing, or dental work, can trigger the development of aphthous ulcers.
- Stress: High levels of stress or emotional tension can weaken the immune system and increase the likelihood of aphthous ulcers.
- Dietary Factors: Certain foods and dietary habits may trigger or exacerbate aphthous ulcers in some people. These can include acidic or spicy foods, citrus fruits, and food allergies.
- Hormonal Changes: Hormonal fluctuations, such as those occurring during menstruation, pregnancy, or menopause, can sometimes lead to the development of canker sores.
- Underlying Medical Conditions: Certain underlying medical conditions, such as celiac disease, Crohn’s disease, or Behçet’s syndrome, may be associated with an increased risk of aphthous ulcers.
- Medications: Some medications, particularly those that affect the immune system, may contribute to the development of canker sores as a side effect.
While these factors are associated with aphthous ulcers, the exact cause can vary from person to person. Additionally, some individuals may experience recurrent aphthous ulcers without a clear identifiable cause. If you frequently experience aphthous ulcers or have severe and persistent ulcers, it’s advisable to consult a healthcare provider or dentist for a thorough evaluation and appropriate management.
Symptoms of Aphthous Ulcers
Aphthous ulcers, also known as canker sores, can be quite uncomfortable due to their painful nature. They typically share several common symptoms, although the severity and exact presentation can vary from person to person.
The main symptoms of aphthous ulcers include:
-
- Pain: Aphthous ulcers are known for causing significant pain or discomfort. The level of pain can range from mild to severe, making it difficult for individuals to eat, drink, or speak comfortably.
- Lesion Appearance: Aphthous ulcers typically appear as small, round or oval-shaped sores with a white or yellow center and a red border. The size of the ulcers can vary, but they are generally less than one centimeter in diameter.
- Location: These ulcers most commonly develop on the soft tissues inside the mouth. Common sites include the tongue, inner cheeks, gums, and the soft palate at the back of the mouth. They can also occasionally appear on the lips or the throat.
- Sensitivity: The area surrounding the aphthous ulcer can become sensitive and inflamed. This sensitivity can make it painful to touch or irritate the ulcer.
- Difficulty Eating and Drinking: Due to the pain, individuals with aphthous ulcers may experience difficulty eating and drinking, especially when consuming acidic or spicy foods.
- Swelling: In some cases, the area around the ulcer may become slightly swollen.
- Discomfort While Speaking: Aphthous ulcers can cause discomfort or pain while speaking, especially if they are located on the tongue or inner cheek.
- Recurrent Episodes: Many individuals with aphthous ulcers experience recurrent episodes, with new ulcers appearing periodically. The frequency and severity of these episodes can vary widely.
Aphthous ulcers are not contagious, and they typically heal on their own within 1-2 weeks. Over-the-counter and prescription topical medications can be used to manage pain and promote healing. If the ulcers are persistent, unusually large, or accompanied by other concerning symptoms, it is advisable to seek medical advice from a healthcare provider or dentist for a thorough evaluation and appropriate treatment.
Herpetic Ulcers
Herpetic ulcers are oral or genital lesions characterized by clusters of small, fluid-filled blisters that rupture and form painful ulcers. These ulcers are caused by the herpes simplex virus (HSV), with HSV-1 commonly causing oral herpes (herpetic ulcers around the mouth) and HSV-2 often responsible for genital herpes (herpetic ulcers in the genital area).

Herpetic ulcers can be highly contagious, especially during the blistering stage when the virus sheds from the open sores. They are often preceded by a tingling or burning sensation at the site where the ulcers will appear. These ulcers can be painful, itchy, and uncomfortable, making daily activities like eating, drinking, and urinating difficult.
The duration of herpetic ulcers can range from 2-3 weeks, including the blistering stage. Antiviral medications are commonly prescribed to reduce symptoms, speed up healing, and decrease the likelihood of transmission to others. Good hygiene practices and the use of barrier methods during sexual activity are also recommended to prevent the spread of genital herpes.
Causes of Herpetic Ulcers
Herpetic ulcers, caused by the herpes simplex virus (HSV), particularly HSV-1 (oral herpes) and HSV-2 (genital herpes), are primarily transmitted through direct contact with the virus. The virus enters the body through mucous membranes or breaks in the skin.
Here are the main causes and modes of transmission for herpetic ulcers:
-
- Viral Infection: The primary cause of herpetic ulcers is infection with the herpes simplex virus (HSV). HSV-1 typically causes oral herpes and herpetic ulcers around the mouth, while HSV-2 is responsible for genital herpes and ulcers in the genital area. Infections occur when the virus comes into contact with the skin or mucous membranes.
- Direct Contact: The most common mode of transmission is direct contact with an active herpetic lesion. This can occur through activities such as kissing (oral herpes), sexual contact (genital herpes), or sharing items like eating utensils, towels, or lip balm with someone who has an active outbreak.
- Asymptomatic Shedding: Even when no visible symptoms are present, individuals infected with HSV can shed the virus and potentially transmit it to others. Asymptomatic shedding is more common with genital herpes but can also occur with oral herpes.
- Vertical Transmission: Herpes can be transmitted from an infected mother to her newborn during childbirth. This can lead to severe complications in the infant.
- Autoinoculation: In some cases, the virus can spread to other parts of the body through self-inoculation. For example, touching an active oral herpes sore and then touching the eyes can result in ocular herpes.
- Stress and Immune System Weakening: Factors such as stress, illness, a weakened immune system, or other underlying health conditions can trigger recurrent outbreaks of herpetic ulcers in individuals who are already infected with HSV.
A person is infected with HSV, the virus remains in their body for life. While there is no cure, antiviral medications can help manage symptoms, reduce the frequency of outbreaks, and decrease the risk of transmission to others. Safer sex practices, including the use of condoms or dental dams, can help reduce the risk of genital herpes transmission during sexual activity. Individuals with herpes should also avoid close contact with others during active outbreaks to minimize the risk of transmission.
Symptoms of Herpetic Ulcers
Herpetic ulcers, which are caused by the herpes simplex virus (HSV), typically exhibit a set of characteristic symptoms. These symptoms can vary in intensity and presentation depending on whether it’s oral herpes (caused by HSV-1) or genital herpes (caused by HSV-2).
Here are the common symptoms of herpetic ulcers:
-
- Tingling or Burning Sensation: Before the appearance of herpetic ulcers, many individuals experience a tingling, burning, or itching sensation at the site where the ulcers will develop. This is often referred to as a prodrome and can last for a few hours to a day before visible symptoms appear.
- Painful Ulcers: Herpetic ulcers are characterized by the presence of small, fluid-filled blisters that quickly rupture, leaving behind painful, open sores or ulcers. These ulcers are typically shallow and have a red border.
- Clustered Blisters: The blisters associated with herpetic ulcers tend to cluster together, forming a group of tiny, often irregularly shaped vesicles.
- Swelling: The area around the ulcers may become swollen and inflamed, causing additional discomfort.
- Pain and Itching: The ulcers can be painful, causing discomfort during activities such as eating, drinking, urinating (in the case of genital herpes), and speaking. Some individuals also experience itching in the affected area.
- Flu-Like Symptoms: In some cases, particularly during the initial outbreak of genital herpes, individuals may experience flu-like symptoms such as fever, headache, muscle aches, and swollen lymph nodes.
- Crusting and Healing: Over the course of about 2-3 weeks, the herpetic ulcers will gradually crust over and heal. During this time, the ulcers may scab before the skin fully regenerates.
- Recurrence: Herpes infections are often recurrent. After the initial outbreak, the virus remains dormant in nerve cells and can re-activate, causing subsequent outbreaks of herpetic ulcers. Recurrences may be less severe and shorter in duration than the initial outbreak.
Herpes is highly contagious, especially when the ulcers are present and during the prodrome phase when symptoms are felt but ulcers have not yet formed. Safer sex practices and good hygiene are important for reducing the risk of transmission. Antiviral medication may help manage symptoms, decrease outbreak frequency and lessen transmission risk. Individuals with herpes should consult a healthcare provider for proper diagnosis and management.
Comparison Table of Aphthous Ulcers and Herpetic Ulcers
Here is a comparison table highlighting the key differences between aphthous ulcers and herpetic ulcers:
| Characteristic | Aphthous Ulcers | Herpetic Ulcers |
|---|---|---|
| Cause | Unknown, likely immune-related factors | Caused by the herpes simplex virus |
| Contagious | Non-contagious | Highly contagious, especially during outbreaks |
| Appearance | Small, round or oval, white/yellow center, red border | Cluster of small, fluid-filled blisters that rupture |
| Location | Inside the mouth (tongue, cheeks, soft palate) | Around the mouth (oral herpes) or genital area (genital herpes) |
| Pain | Painful and sensitive | Painful and uncomfortable |
| Tingling/Burning Sensation | Rarely precedes ulcers | Often precedes ulcers (prodrome) |
| Duration | Typically 1-2 weeks | About 2-3 weeks, including blistering stage |
| Recurrence | May recur, but not always | Often recurs, especially in genital herpes |
| Treatment | Topical analgesics, lifestyle adjustments | Antiviral medications, pain relief, hygiene practices |
| Contagious Phase | Not contagious | Highly contagious during outbreaks |
While this table provides a concise comparison, individual experiences with these ulcers can vary, and it’s important to consult a healthcare provider for accurate diagnosis and appropriate treatment if you suspect you have either type of ulcer.
Treatment for Aphthous Ulcers and Herpetic Ulcers
The treatment for aphthous ulcers (canker sores) and herpetic ulcers (oral or genital herpes) differs due to their distinct causes. Below is a brief outline of treatments available for each of the following conditions:
Treatment for Aphthous Ulcers (Canker Sores):
- Topical Analgesics: Over-the-counter topical gels or ointments containing ingredients like benzocaine, lidocaine, or dyclonine can provide temporary pain relief and help reduce discomfort.
- Oral Rinses: Antiseptic mouth rinses or oral solutions can help clean the ulcer and prevent infection.
- Corticosteroids: In severe cases, your healthcare provider may prescribe corticosteroid ointments or mouth rinses to reduce inflammation and speed up healing.
- Avoidance of Triggers: Identifying and avoiding trigger factors, such as certain foods (acidic, spicy), stress, and oral trauma, can help prevent future outbreaks.
- Dietary Supplements: Some studies suggest that supplements like vitamin B12, zinc, and lysine may help reduce the frequency and severity of aphthous ulcers in some individuals.
Treatment for Herpetic Ulcers (Oral and Genital Herpes):
- Antiviral Medications: Antiviral drugs, such as acyclovir, valacyclovir, and famciclovir, are prescribed to manage herpetic ulcers. These medications can help reduce symptoms, shorten the duration of outbreaks, and decrease viral shedding (the period when the virus is most contagious).
- Pain Relief: Over-the-counter pain relievers like acetaminophen or ibuprofen can help manage the pain associated with herpetic ulcers.
- Good Hygiene Practices: To prevent the spread of herpes, it’s crucial to practice good hygiene. Wash your hands frequently, avoid touching the ulcers, and maintain proper genital hygiene in the case of genital herpes.
- Safer Sex: For genital herpes, the use of condoms or dental dams during sexual activity can reduce the risk of transmission to a partner.
- Stress Reduction: Managing stress can help reduce the frequency of herpes outbreaks, as stress can trigger or exacerbate them.
It’s essential to consult with a healthcare provider or dentist for a proper diagnosis and treatment plan if you have aphthous ulcers or herpetic ulcers, especially if the symptoms are severe, persistent, or if you have concerns about transmission. Additionally, individuals with herpetic ulcers should be mindful of their contagious nature and take appropriate precautions to prevent spreading the virus to others.
Conclusion
Aphthous Ulcers and Herpetic Ulcers represent two distinct types of oral lesions with different causes, characteristics, and implications. Aphthous ulcers, also known as canker sores, are non-contagious, typically small, painful sores that occur inside the mouth and often result from factors like immune dysfunction or triggers such as stress and diet.
Herpetic ulcers, caused by the herpes simplex virus, are highly contagious and manifest as clusters of fluid-filled blisters that rupture, leading to painful ulcers on or around the mouth (oral herpes) or genital area (genital herpes). Understanding these differences is essential for proper diagnosis and treatment, as well as for preventing transmission in the case of herpetic ulcers.