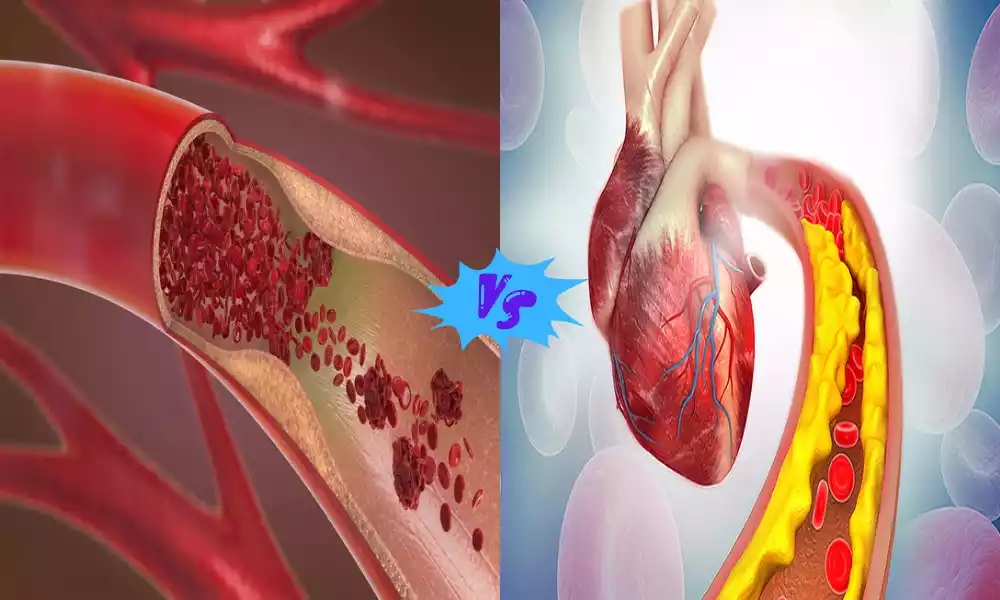
Arteriosclerosis and Atherosclerosis are two closely related but distinct cardiovascular conditions. Arteriosclerosis refers to a general thickening and stiffening of the arteries, often associated with aging. Atherosclerosis, on the other hand, is a specific type of arteriosclerosis characterized by the buildup of fatty deposits and plaques within the arterial walls. Both conditions can lead to serious health problems, including heart disease and stroke, making it crucial to understand their differences and take steps to manage and prevent them.
What is Arteriosclerosis?
Arteriosclerosis is a general term used to describe a group of diseases in which the arteries, the blood vessels that carry oxygenated blood from the heart to the rest of the body, become thickened and less elastic. This thickening and loss of elasticity can occur naturally with age, but it can also result from various pathological processes.
Arteriosclerosis can restrict blood flow and reduce the arteries’ ability to expand and contract, potentially leading to various cardiovascular problems, including hypertension (high blood pressure) and decreased blood supply to vital organs. It is important to note that atherosclerosis, a specific type of arteriosclerosis characterized by the buildup of fatty plaques within the artery walls, is one of the most common and significant forms of arteriosclerosis.
Causes and Risk Factors of Arteriosclerosis
Arteriosclerosis is a general term encompassing several types of arterial wall thickening and stiffening. The causes and risk factors for arteriosclerosis can vary depending on the specific type of arteriosclerosis, but here are some general factors that can contribute to or increase the risk of arteriosclerosis:
Causes:
- Aging: Arteriosclerosis is often a natural part of the aging process, as arteries naturally become less flexible and may thicken over time.
- Genetics: Family history can play a role in the development of arteriosclerosis, as some individuals may inherit genetic factors that predispose them to arterial changes.
Risk Factors:
- High Blood Pressure (Hypertension): Elevated blood pressure puts constant stress on the arterial walls, contributing to their thickening and stiffening.
- High Cholesterol Levels: Elevated levels of LDL (low-density lipoprotein) cholesterol, often referred to as “bad” cholesterol, can contribute to the buildup of fatty deposits in arterial walls.
- Smoking: Smoking is a major risk factor for arteriosclerosis, as it can damage the endothelial lining of arteries and promote inflammation.
- Diabetes: Individuals with diabetes are at a higher risk of arteriosclerosis due to the effects of chronic high blood sugar on the arteries.
- Obesity: Being overweight or obese is associated with an increased risk of arteriosclerosis, as it often leads to other risk factors like high blood pressure and diabetes.
- Physical Inactivity: A sedentary lifestyle can contribute to obesity, high blood pressure, and other risk factors for arteriosclerosis.
- Unhealthy Diet: Consuming a diet high in saturated fats, trans fats, and excessive sodium can contribute to high blood pressure and high cholesterol levels, increasing the risk of arteriosclerosis.
- Chronic Inflammation: Conditions associated with chronic inflammation, such as rheumatoid arthritis or lupus, can accelerate the development of arteriosclerosis.
- Certain Medications: Some medications, such as corticosteroids and immunosuppressants, can potentially increase the risk of arteriosclerosis.
- Stress: High levels of chronic stress may contribute to unhealthy behaviors (e.g., overeating, smoking) and affect blood pressure, which can impact the arteries.
- Other Medical Conditions: Conditions like chronic kidney disease and autoimmune disorders can increase the risk of arteriosclerosis.
- Radiation Therapy: Radiation therapy for cancer treatment, especially when directed at the chest area, can damage arteries and increase the risk of arteriosclerosis.
- Chemical Exposure: Prolonged exposure to certain chemicals, such as lead or arsenic, can contribute to arterial damage and thickening.
While these factors can increase the risk of arteriosclerosis, the condition can also develop for no apparent reason, especially as a part of the aging process. Managing and controlling these risk factors through lifestyle changes, medications, and regular medical check-ups can help reduce the risk of arteriosclerosis and its associated complications.
Symptoms of Arteriosclerosis
Arteriosclerosis is a condition characterized by the thickening and hardening of arterial walls. It often develops gradually over many years and may not cause noticeable symptoms in its early stages. As the condition progresses and affects blood flow, some individuals may experience symptoms, which can vary depending on the specific arteries involved and the extent of the arteriosclerosis.
Common symptoms of arteriosclerosis include:
- Angina: Chest pain or discomfort is a common symptom when arteriosclerosis affects the coronary arteries that supply blood to the heart muscle. Coronary Artery Disease may be present.
- Intermittent Claudication: Pain, cramping, or weakness in the legs during physical activity or exercise, which typically subsides with rest. This is a common symptom when arteriosclerosis affects the arteries in the legs.
- Cold Extremities: Reduced blood flow to the extremities (hands and feet) can lead to coldness or numbness in these areas, especially during colder weather.
- Muscle Weakness: Weakness or fatigue in muscles, particularly in the arms and legs, may occur due to reduced blood supply.
- Impotence: Men with arteriosclerosis affecting the arteries in the pelvis may experience erectile dysfunction (impotence) due to insufficient blood flow to the genital area.
- High Blood Pressure: In some cases, arteriosclerosis can lead to hypertension (high blood pressure), which may result in symptoms such as headaches, dizziness, or nosebleeds.
- Vision Problems: If arteriosclerosis affects the arteries supplying blood to the eyes, it can lead to vision problems or even vision loss.
- Renal Symptoms: Arteriosclerosis in the renal arteries may cause kidney dysfunction, which can manifest as high blood pressure or changes in urination patterns.
- Cognitive Impairment: In rare cases, arteriosclerosis in the arteries supplying blood to the brain can contribute to cognitive impairment, memory problems, or dementia.
Arteriosclerosis is asymptomatic until it reaches an advanced stage or leads to complications such as heart attacks, strokes, or peripheral artery disease. Moreover, individuals may experience symptoms differently, and the severity of symptoms can vary widely.
If you or someone you know is experiencing symptoms that may be related to arteriosclerosis, it is essential to seek medical evaluation and advice promptly. Early diagnosis and management of arteriosclerosis can help prevent further progression and reduce the risk of associated complications.
What is Atherosclerosis?
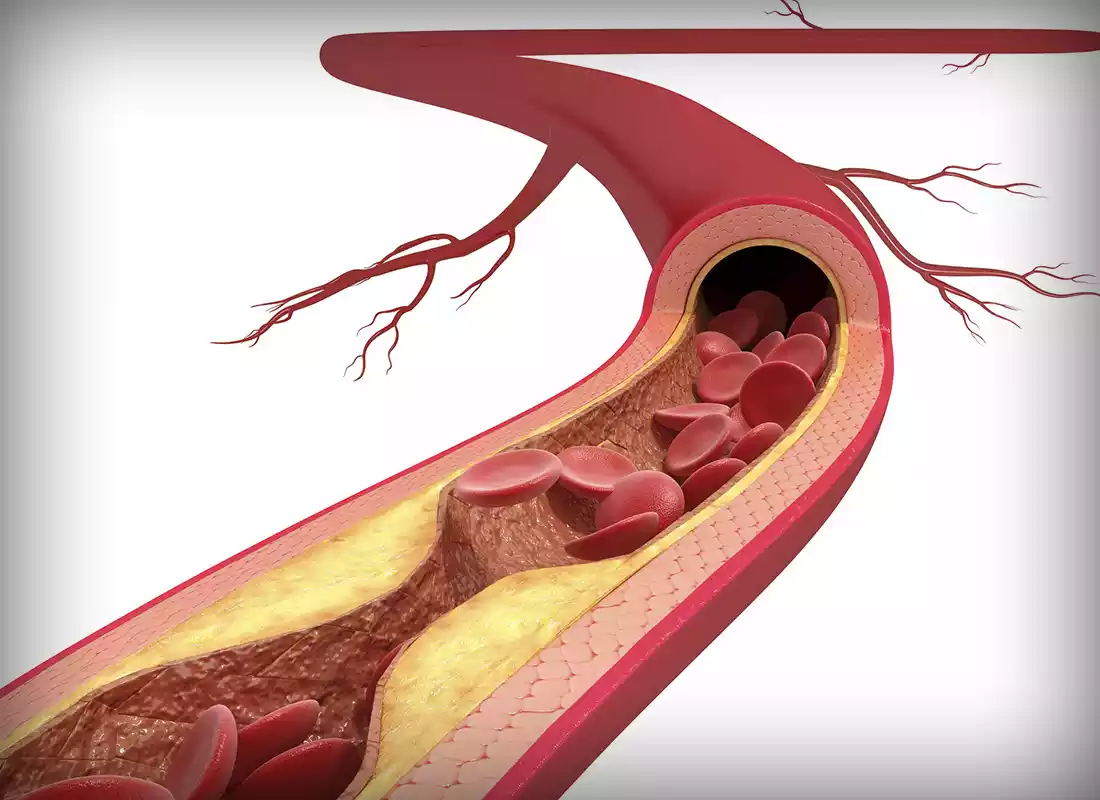
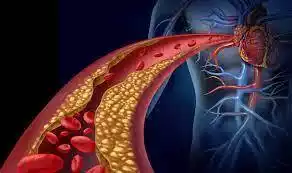
Atherosclerosis is one of the more prevalent and distinctive forms of arteriosclerosis. It is a chronic and progressive disease characterized by the buildup of fatty deposits, cholesterol, cellular waste products, calcium, and other substances within the walls of arteries. These deposits, known as plaques, can gradually narrow and stiffen the arteries, restricting blood flow to vital organs and tissues.
The process of atherosclerosis typically begins when the inner lining of an artery (the endothelium) is damaged, often due to factors like high blood pressure, smoking, or high levels of cholesterol in the bloodstream. In response to this damage, the body’s immune system and inflammatory processes are triggered, leading to the accumulation of plaque over time.
Atherosclerosis is a major contributor to cardiovascular diseases, including coronary artery disease (which can lead to heart attacks), carotid artery disease (which can lead to strokes), and peripheral artery disease (which affects blood flow to the limbs). It is a significant public health concern and requires lifestyle changes, medications, and sometimes invasive procedures to manage and prevent its complications.
Causes and Risk Factors of Atherosclerosis
Atherosclerosis is a specific type of arteriosclerosis characterized by the buildup of fatty deposits and plaques within arterial walls. The causes and risk factors for atherosclerosis are multifactorial and complex, involving various aspects of lifestyle, genetics, and overall health.
Here are the key causes and risk factors associated with atherosclerosis:
Causes:
- Endothelial Damage: The inner lining of arteries, known as the endothelium, can be damaged by factors such as high blood pressure, smoking, and high levels of cholesterol in the bloodstream. This endothelial damage is a primary trigger for atherosclerosis.
- Inflammation: Chronic inflammation in the body, often due to conditions like autoimmune diseases or infections, can contribute to endothelial damage and promote the formation of atherosclerotic plaques.
- Cholesterol and Lipoproteins: Elevated levels of low-density lipoprotein (LDL) cholesterol, often referred to as “bad” cholesterol, can lead to the accumulation of cholesterol in artery walls, a key component of atherosclerotic plaques.
- Oxidation: Oxidized LDL cholesterol is more likely to be deposited in artery walls, initiating plaque formation.
- Immune Response: The body’s immune system can play a role in atherosclerosis by attempting to repair damaged arterial walls. This response can lead to the buildup of fatty deposits and plaque formation.
Risk Factors:
- Age: The risk of atherosclerosis increases with age, as the condition often develops gradually over many years.
- Gender: Men are generally at a higher risk of atherosclerosis compared to premenopausal women. Postmenopausal women’s risk approaches that of men.
- Family History: A family history of heart disease or atherosclerosis can increase an individual’s risk, suggesting a genetic component.
- High Blood Pressure (Hypertension): Hypertension puts added stress on artery walls, making them more susceptible to damage.
- Smoking: Smoking damages the endothelium and increases inflammation, greatly elevating the risk of atherosclerosis.
- Diet: Consuming a diet high in saturated fats, trans fats, and cholesterol can contribute to elevated LDL cholesterol levels.
- Physical Inactivity: A sedentary lifestyle can lead to weight gain, high blood pressure, and abnormal cholesterol levels, all of which promote atherosclerosis.
- Diabetes: People with diabetes often have higher levels of glucose in their blood, which can damage blood vessels and accelerate atherosclerosis.
- Obesity: Being overweight or obese can lead to increased inflammation and higher levels of LDL cholesterol.
- High Stress Levels: Chronic stress may contribute to unhealthy behaviors (e.g., overeating, smoking) and affect blood pressure, increasing the risk of atherosclerosis.
- Alcohol Consumption: Excessive alcohol intake can raise blood pressure and contribute to obesity, potentially increasing the risk of atherosclerosis.
- Certain Medical Conditions: Conditions like rheumatoid arthritis and lupus that involve chronic inflammation can increase the risk of atherosclerosis.
- Genetics: Some genetic factors can predispose individuals to higher cholesterol levels and a greater risk of atherosclerosis.
Understanding these causes and risk factors is crucial for assessing an individual’s risk and taking preventive measures to reduce the likelihood of developing atherosclerosis and its associated complications, such as heart disease and stroke. Lifestyle modifications, medications, and regular medical check-ups are important components of prevention and management.
Symptoms of Atherosclerosis
Atherosclerosis is a specific type of arteriosclerosis characterized by the buildup of fatty deposits and plaques within arterial walls. This condition often develops silently over many years and may not cause noticeable symptoms until it reaches an advanced stage or leads to complications. When symptoms do occur, they can vary depending on the arteries affected and the degree of blockage or narrowing.
Common symptoms of atherosclerosis include:
- Angina: Chest pain or discomfort, often described as pressure, squeezing, or heaviness, can occur when atherosclerosis affects the coronary arteries that supply blood to the heart muscle. This is a common symptom of coronary artery disease and may be triggered by physical exertion or emotional stress.
- Shortness of Breath: Difficulty breathing or shortness of breath, especially during physical activity, can be a symptom of reduced blood flow to the heart due to coronary artery disease.
- Intermittent Claudication: Pain, cramping, or weakness in the legs during physical activity or exercise, which typically subsides with rest. This is a common symptom when atherosclerosis affects the arteries in the legs.
- Cold Extremities: Reduced blood flow to the extremities (hands and feet) can lead to coldness, numbness, or tingling in these areas, especially during colder weather.
- Weak Pulse: Weakened or absent pulses in the affected limbs (arms or legs) can be a sign of reduced blood flow.
- Impotence: Men with atherosclerosis affecting the arteries in the pelvis may experience erectile dysfunction (impotence) due to insufficient blood flow to the genital area.
- High Blood Pressure: Atherosclerosis can contribute to hypertension (high blood pressure), which may result in symptoms such as headaches, dizziness, or nosebleeds.
- Vision Problems: If atherosclerosis affects the arteries supplying blood to the eyes, it can lead to vision problems or even vision loss.
- Renal Symptoms: Atherosclerosis in the renal arteries may cause kidney dysfunction, which can manifest as high blood pressure, changes in urination patterns, or fluid retention.
- Neurological Symptoms: In cases where atherosclerosis affects the arteries supplying blood to the brain, it can lead to neurological symptoms, including transient ischemic attacks (mini-strokes), stroke, or cognitive impairment.
It’s important to note that atherosclerosis can progress silently, and many individuals may have advanced plaque buildup without experiencing symptoms. Additionally, the severity and type of symptoms can vary widely among individuals.
Diagnosis and Screening of Arteriosclerosis and Atherosclerosis
The diagnosis and screening of arteriosclerosis and atherosclerosis typically involve a combination of medical history assessment, physical examinations, and various diagnostic tests. These tests are essential for evaluating the condition of the arteries and identifying the extent of arterial thickening and plaque buildup.
Here are the key methods used for diagnosis and screening:
1. Medical History and Physical Examination:
- The healthcare provider will inquire about your medical history, including risk factors such as family history, smoking, diet, exercise, and other relevant factors.
- A physical examination may reveal signs such as diminished or absent pulses, cold extremities, or other symptoms suggestive of arterial disease.
2. Blood Pressure Measurement:
- High blood pressure (hypertension) is a common risk factor for both arteriosclerosis and atherosclerosis. Regular blood pressure checks are essential for assessing cardiovascular health.
3. Blood Tests:
- Lipid Profile: A lipid panel measures cholesterol levels, including LDL (low-density lipoprotein) and HDL (high-density lipoprotein) cholesterol. Elevated LDL cholesterol is associated with an increased risk of atherosclerosis.
- Blood Glucose: Elevated blood sugar levels may indicate diabetes, a risk factor for both conditions.
- Inflammatory Markers: Certain blood markers, such as C-reactive protein (CRP), can indicate inflammation, which plays a role in atherosclerosis.
4. Imaging Studies:
- Angiography: This can involve various imaging techniques, including:
- Coronary Angiography: To visualize coronary arteries.
- Peripheral Angiography: To evaluate arteries in the limbs.
- Carotid Ultrasound: To assess carotid arteries in the neck.
- Computed Tomography Angiography (CTA): Uses X-rays and computer technology to create detailed images of blood vessels, often for coronary or peripheral artery assessment.
- Magnetic Resonance Angiography (MRA): Uses magnetic fields and radio waves to produce images of blood vessels, commonly for assessing larger arteries.
- Doppler Ultrasound: To measure blood flow and identify areas of narrowing or blockage.
- Intravascular Ultrasound (IVUS): An invasive procedure that uses ultrasound to assess the inside of coronary arteries.
5. Stress Tests:
- Exercise Stress Test (Treadmill Test): Monitors heart activity and symptoms during physical activity to evaluate coronary artery disease.
- Nuclear Stress Test: Combines exercise with nuclear imaging to assess blood flow to the heart.
- Stress Echocardiogram: Uses ultrasound to assess heart function during stress.
6. Coronary Calcium Scoring: A specialized CT scan that measures calcium buildup in the coronary arteries, providing information about atherosclerotic plaque.
7. Electrocardiogram (ECG or EKG): Records electrical activity of the heart to identify irregularities or signs of coronary artery disease.
8. Carotid Intima-Media Thickness (CIMT) Test: Measures the thickness of carotid artery walls using ultrasound to assess early signs of atherosclerosis in the carotid arteries.
9. Ankle-Brachial Index (ABI): Measures blood pressure in the arms and legs to assess peripheral artery disease.
10. Genetic Testing: In some cases, genetic tests may be used to identify inherited conditions that increase the risk of arteriosclerosis or atherosclerosis.
The choice of diagnostic tests may vary depending on an individual’s risk factors, symptoms, and clinical presentation. Early detection and diagnosis are crucial for initiating appropriate treatment and preventive measures to manage and reduce the progression of arteriosclerosis and atherosclerosis.
Treatment Options for Arteriosclerosis and Atherosclerosis
The treatment options for arteriosclerosis and atherosclerosis primarily focus on reducing risk factors, managing symptoms, preventing complications, and improving overall cardiovascular health. The specific treatment plan can vary depending on the severity of the condition and the arteries involved.
Here are the key treatment options:
1. Lifestyle Modifications:
- Diet: Adopting a heart-healthy diet that is low in saturated fats, trans fats, cholesterol, and sodium while emphasizing fruits, vegetables, whole grains, and lean proteins can help manage these conditions.
- Physical Activity: Regular exercise, as recommended by a healthcare provider, can improve cardiovascular health, lower blood pressure, and manage weight.
- Smoking Cessation: Quitting smoking is essential to prevent further damage to arteries and reduce the risk of complications.
- Weight Management: Achieving and maintaining a healthy weight can lower the risk of atherosclerosis and arteriosclerosis, especially if obesity is a contributing factor.
- Stress Reduction: Stress management techniques such as meditation, deep breathing, or yoga can help reduce the impact of chronic stress on cardiovascular health.
2. Medications:
- Cholesterol-Lowering Medications: Statins, fibrates, and other lipid-lowering medications can help reduce elevated LDL cholesterol levels.
- Blood Pressure Medications: Antihypertensive drugs are prescribed to control high blood pressure and reduce the risk of further arterial damage.
- Antiplatelet Medications: Aspirin or other antiplatelet drugs may be recommended to reduce the risk of blood clots forming on atherosclerotic plaques.
- Anti-inflammatory Medications: In some cases, anti-inflammatory medications may be prescribed to reduce inflammation within the arteries.
- Medications to Control Blood Sugar: If diabetes is present, medications or insulin therapy may be needed to manage blood sugar levels effectively.
3. Invasive Procedures:
- Angioplasty and Stent Placement: In cases of severe blockages, a minimally invasive procedure called angioplasty may be performed to open narrowed arteries. A stent (a small metal mesh tube) may be inserted to keep the artery open.
- Coronary Artery Bypass Surgery: For advanced coronary artery disease, bypass surgery may be necessary to create new routes for blood to flow around blocked arteries.
- Carotid Endarterectomy: This surgical procedure removes plaque from the carotid arteries to reduce the risk of stroke.
4. Medications for Symptom Management:
- Anti-anginal Medications: These drugs can help relieve chest pain (angina) associated with atherosclerosis.
- Pain Relief: Over-the-counter or prescription pain medications may be used to manage intermittent claudication pain.
5. Blood Sugar Control: For individuals with diabetes, maintaining good control of blood sugar levels is crucial to managing atherosclerosis and arteriosclerosis.
6. Hypertension Management: Effective management of high blood pressure through lifestyle changes and medications can slow the progression of arterial damage.
7. Cardiac Rehabilitation: Following a cardiovascular event or intervention, cardiac rehabilitation programs can provide supervised exercise, education, and support to improve heart health and reduce the risk of recurrence.
8. Regular Follow-Up: Ongoing monitoring by a healthcare provider is essential to track progress, adjust treatment plans, and manage risk factors effectively.
Treatment plans are individualized based on the patient’s specific condition, risk factors, and overall health. Lifestyle changes and preventive measures play a significant role in managing arteriosclerosis and atherosclerosis, as they address the underlying causes and reduce the risk of complications. Patients should work closely with their healthcare team to develop and follow a personalized treatment plan.
Comparison Table of of Arteriosclerosis and Atherosclerosis
Here’s a comparison table of arteriosclerosis and atherosclerosis to highlight their key differences:
| Characteristic | Arteriosclerosis | Atherosclerosis |
|---|---|---|
| Definition | General term for arterial wall thickening and stiffening. | A specific type of arteriosclerosis characterized by the buildup of plaques within arterial walls. |
| Primary Affected Tissues | Arterial walls in various parts of the body. | Arterial walls throughout the body, with a focus on specific arteries like coronary, carotid, and peripheral arteries. |
| Underlying Cause | Aging and genetic factors are common contributors. | Lipid accumulation, inflammation, endothelial damage, and other factors play a prominent role. |
| Pathological Changes | Thickening and loss of elasticity in arterial walls. | Buildup of fatty deposits (plaques) within arterial walls, leading to narrowing and hardening of the arteries. |
| Risk Factors | Hypertension, smoking, age, genetic factors. | High LDL cholesterol, smoking, hypertension, diabetes, age, genetic factors. |
| Common Symptoms | May be asymptomatic or present with non-specific symptoms such as cold extremities, muscle weakness. | Angina (chest pain), shortness of breath, intermittent claudication, vision problems, renal dysfunction, neurological symptoms. |
| Diagnostic Tests | Blood pressure measurement, lipid profile, physical examination. | Imaging (angiography, CT, MRI), blood tests (lipid profile, CRP), stress tests, ECG, ultrasound, ABI, coronary calcium scoring. |
| Treatment Options | Lifestyle modifications, medications for risk factor control, symptom management, surgical interventions if necessary. | Lifestyle modifications, cholesterol-lowering medications, blood pressure control, antiplatelet drugs, surgical interventions (angioplasty, bypass surgery). |
This table provides a concise overview of the key differences between arteriosclerosis and atherosclerosis, highlighting their definitions, primary affected tissues, underlying causes, pathological changes, risk factors, common symptoms, diagnostic tests, and treatment options. Keep in mind that both conditions involve arterial wall changes and can have significant implications for cardiovascular health.
Exercise and Physical Activity

Lifestyle changes play a crucial role in the prevention and management of arteriosclerosis and atherosclerosis. These changes can help reduce risk factors and improve overall cardiovascular health.
Here are key lifestyle modifications for prevention:
- Healthy Diet:
- Heart-Healthy Eating: Adopt a diet low in saturated fats, trans fats, cholesterol, and sodium while emphasizing fruits, vegetables, whole grains, lean proteins (such as poultry, fish, and legumes), and nuts.
- Limit Processed Foods: Minimize the consumption of processed and fried foods, which often contain unhealthy fats and high levels of salt.
- Portion Control: Keep an eye on your portions to reduce calories and maintain an ideal weight.
- Limit Sugary Beverages: Reduce or eliminate sugary drinks and opt for water, herbal tea, or unsweetened beverages.
- Regular Physical Activity:
- Aim for at least 150 minutes of moderate-intensity aerobic exercise (e.g., brisk walking, cycling) or 75 minutes of vigorous-intensity aerobic exercise (e.g., running, swimming) per week.
- Make time for strength-training exercises at least twice each week in order to strengthen and develop endurance in your muscles.
- Consult with a healthcare provider before starting a new exercise program, especially if you have existing medical conditions.
- Tobacco Cessation:
- Quit smoking and avoid exposure to secondhand smoke. Smoking is a major risk factor for both arteriosclerosis and atherosclerosis.
- Stress Management:
- Practice stress-reduction techniques such as meditation, deep breathing exercises, yoga, or mindfulness to manage stress effectively.
- Moderate Alcohol Consumption:
- If you consume alcohol, do so in moderation. Women should aim to consume at least one drink daily while men should aim to have two beverages daily.
- Weight Management:
- Achieve and maintain a healthy weight through a combination of balanced eating and regular physical activity.
- Consult with a healthcare provider or registered dietitian for personalized weight management guidance.
- Medication Adherence:
- If prescribed medications to control blood pressure, cholesterol levels, or other risk factors, take them as directed by your healthcare provider.
- Regular Health Check-Ups:
- Consistent visits with your physician will enable you to maintain healthy cholesterol, blood pressure and cardiovascular wellbeing.
- Discuss any concerns or symptoms related to arteriosclerosis or atherosclerosis with your healthcare provider promptly.
- Blood Sugar Control:
- If you suffer from diabetes, be sure to collaborate closely with your medical team in order to manage your blood sugar effectively.
- Education and Awareness:
- Stay informed about your condition and risk factors. Be mindful of the significance of early intervention.
By incorporating these lifestyle changes into your daily routine, you can reduce your risk of arteriosclerosis and atherosclerosis, as well as other cardiovascular diseases. Prevention is a powerful tool in maintaining long-term cardiovascular health and reducing the likelihood of complications.
Final Thoughts
Arteriosclerosis and Atherosclerosis are related yet distinct cardiovascular conditions. Arteriosclerosis refers to the general thickening and stiffening of arterial walls, often associated with aging, while atherosclerosis is a specific type of arteriosclerosis characterized by the buildup of plaques within arteries. Atherosclerosis is a more advanced and clinically significant form of arterial disease, posing a higher risk of complications like heart attacks and strokes.
While both conditions share some common risk factors, they require different diagnostic approaches and treatment strategies. Managing these conditions involves lifestyle changes, medication, and, in some cases, surgical interventions to preserve cardiovascular health and reduce the risk of associated complications.