Asthma and Allergic Rhinitis are common respiratory conditions that often coexist, leading to a range of symptoms such as coughing, shortness of breath, and nasal congestion. Asthma is characterized by inflamed airways and increased mucus production, while allergic rhinitis, also known as hay fever, is an allergic reaction affecting the nasal passages. Both conditions share triggers such as allergens and exhibit overlapping symptoms, making it crucial to understand their connection and how to effectively manage them for improved respiratory health.
Definition of Asthma
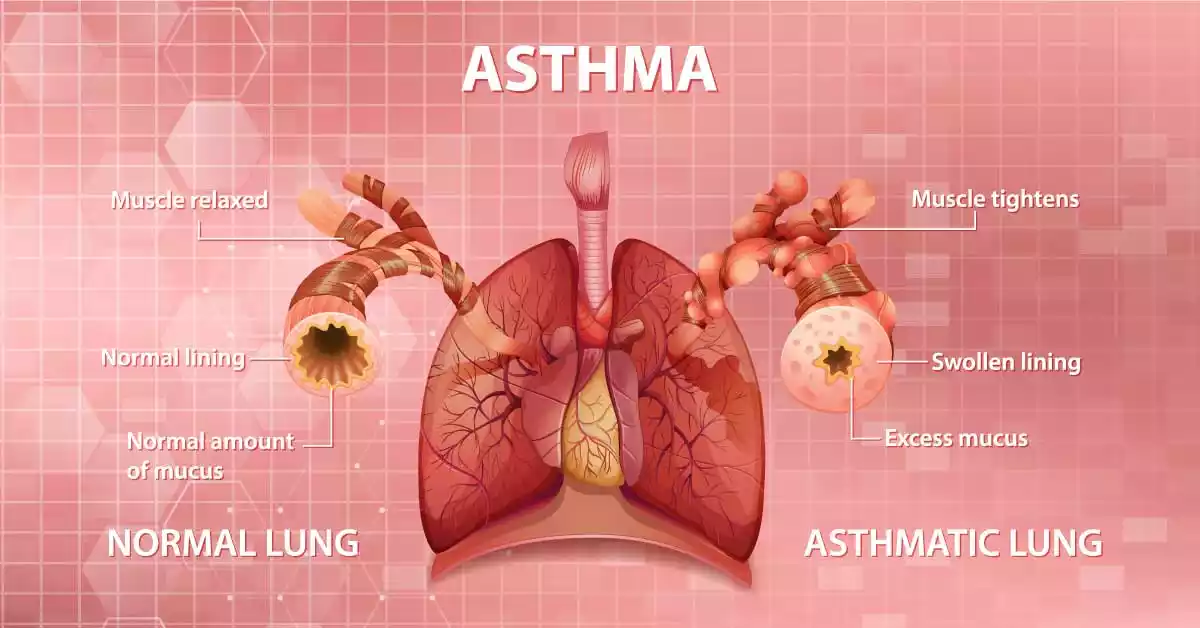
Asthma is a chronic respiratory illness characterized by inflammation and obstruction in the airways of the lungs. This narrowing makes it difficult for individuals with asthma to breathe properly, leading to symptoms such as wheezing, coughing, shortness of breath, and chest tightness.
Asthma symptoms can vary in severity and may be triggered or worsened by factors like allergens, respiratory infections, exercise, and exposure to irritants. While asthma is a long-term condition, it can be managed with medications and lifestyle modifications to control symptoms and prevent asthma attacks.
Symptoms of Asthma
Asthma symptoms can vary in terms of frequency and intensity among individuals. They typically involve the airways becoming inflamed and narrowed, leading to difficulty in breathing.
Common asthma symptoms include:
-
- Shortness of Breath: Asthma patients may have difficulty breathing during physical activities or sleep. They may find their airways blocked off entirely.
- Coughing: Persistent coughing, especially at night or early in the morning, is a common asthma symptom. Your throat could either become dry or produce mucus.
- Wheezing: Wheezing is a high-pitched whistling or squeaky sound that occurs when breathing. It is often more pronounced during exhalation and is a classic sign of asthma.
- Chest Tightness: Many individuals with asthma describe a feeling of tightness or pressure in the chest, which can be uncomfortable and distressing.
- Increased Mucus Production: Some people with asthma may experience an increase in the production of thick mucus in the airways, contributing to coughing and difficulty breathing.
- Difficulty Sleeping: Asthma symptoms often worsen at night, leading to difficulty falling asleep or disrupted sleep.
- Difficulty Speaking: Severe asthma attacks can make it challenging to speak full sentences due to the limited ability to inhale and exhale effectively.
- Anxiety or Panic: As a result of breathing difficulties, asthma can trigger feelings of anxiety or panic, further exacerbating symptoms.
Asthma symptoms can be intermittent or chronic, and they can range from mild to severe. Asthma exacerbations, also known as asthma attacks, can occur when symptoms suddenly worsen and require prompt medical attention. These attacks may be triggered by allergens, respiratory infections, exposure to irritants, or other factors.
Definition of Allergic Rhinitis
Allergic rhinitis, commonly known as hay fever or seasonal allergies, is an allergic reaction that primarily affects the nasal passages. Allergies occur when our immune systems respond negatively to allergens such as dust mites, pollen grains or pet dander; or spores. The result is inflammation of the nasal lining, leading to symptoms like sneezing, runny or stuffy nose, itching in the nose and throat, and watery eyes.

Allergic rhinitis can be categorized as seasonal, occurring during specific times of the year when certain allergens are prevalent, or perennial, where symptoms persist throughout the year due to exposure to year-round allergens. It can significantly impact an individual’s quality of life but can often be managed with medications, allergen avoidance, and other treatment strategies.
Symptoms of Allergic Rhinitis
Allergic rhinitis, commonly referred to as hay fever or seasonal allergies, is characterized by inflammation of the nasal passages due to an allergic response to specific allergens.
Allergic Rhinitis symptoms may be severe and include:
-
- Sneezing: Frequent and repetitive sneezing is a common symptom of allergic rhinitis, especially when exposed to allergens like pollen, dust, or pet dander.
- Runny or Stuffy Nose: Individuals with allergic rhinitis often experience a runny or congested nose. This can lead to a clear discharge or thicker mucus.
- Itchy or Watery Eyes: Allergic rhinitis can cause itching, redness, and excessive tearing of the eyes, known as allergic conjunctivitis.
- Itchy Throat or Ears: Some people with allergic rhinitis may also experience itching in the throat or ears.
- Postnasal Drip: Excess mucus production can result in postnasal drip, leading to a sensation of mucus dripping down the back of the throat.
- Coughing: Chronic coughing may occur as a result of postnasal drip or throat irritation.
- Fatigue: Persistent allergic rhinitis symptoms, especially if they disrupt sleep, can lead to fatigue and a decreased ability to concentrate.
- Ear Pressure or Fullness: Some individuals with allergic rhinitis may experience a feeling of pressure or fullness in the ears due to congestion.
- Reduced Sense of Smell or Taste: Nasal congestion can impair the sense of smell and, subsequently, the sense of taste.
- Worsening of Asthma Symptoms: In individuals with coexisting asthma and allergic rhinitis, allergic rhinitis can exacerbate asthma symptoms, leading to increased coughing and wheezing.
- Facial Pressure or Headache: Sinus congestion and inflammation can cause facial pressure or headaches in some individuals.
The severity and duration of allergic rhinitis symptoms can vary depending on the specific allergens involved (e.g., pollen, mold, dust mites, animal dander) and the individual’s sensitivity to these allergens. Symptoms are typically seasonal for those with seasonal allergic rhinitis but can persist year-round (perennial allergic rhinitis) in response to indoor allergens.
Comparison Table of Asthma and Allergic Rhinitis
Here’s a comparison table highlighting the key differences between asthma and allergic rhinitis:
| Aspect | Asthma | Allergic Rhinitis |
|---|---|---|
| Definition | Chronic respiratory condition | Allergic reaction affecting nasal passages |
| Affected Areas | Lower airways (bronchi) | Upper airways (nose and nasal passages) |
| Primary Symptoms | Wheezing, coughing, shortness of breath, chest tightness | Sneezing, runny/stuffy nose, itchy/watery eyes |
| Secondary Symptoms | May include coughing, mucus production, chest pain, fatigue | Coughing, postnasal drip, fatigue |
| Diagnostic Tools | Spirometry, peak flow measurement, chest X-rays, allergy testing | Clinical evaluation, allergy testing |
| Treatment Approaches | Medications (e.g., bronchodilators, corticosteroids), inhalers, lifestyle management | Medications (e.g., antihistamines, nasal corticosteroids), allergen avoidance |
| Long-term Outlook | Can be managed effectively with treatment, but may not be curable | Often manageable with treatment, not typically curable |
| Common Triggers | Allergens, respiratory infections, exercise, irritants, stress | Pollen, dust mites, pet dander, mold, irritants, pollution |
| Coexistence with the Other Condition | Asthma and allergic rhinitis can coexist and share some triggers | Coexistence is common, and allergic rhinitis can exacerbate asthma symptoms |
This table highlights key differences, asthma and allergic rhinitis can co-occur in individuals, and managing both conditions simultaneously may require a coordinated approach involving healthcare providers. Additionally, the severity and specific symptoms can vary among individuals with these conditions.
Diagnosing Asthma and Allergic Rhinitis
Diagnosing asthma and allergic rhinitis involves a combination of clinical evaluation, medical history assessment, and diagnostic tests. Here’s an overview of how these two conditions are typically diagnosed:
Diagnosing Asthma:
- Medical History: The process usually begins with a detailed medical history, where the healthcare provider will ask about your symptoms, their frequency, and any triggers that worsen or alleviate your breathing problems. Be prepared to discuss your family history of asthma or other respiratory conditions.
- Physical Examination: A physical examination may be conducted to listen for wheezing or other respiratory sounds and to assess your overall lung function.
- Spirometry: This is a common test used to assess lung function. Your test involves breathing deeply and exhaling quickly through a device called the Spirometer to measure how much air can be exhaled at one time and how fast. This test helps measure both of these factors.
- Peak Flow Measurement: A peak flow meter is a portable device that measures how fast you can exhale air. Regular peak flow measurements can help monitor asthma and detect changes in lung function.
- Allergy Testing: Allergy skin tests or blood tests may be performed to identify specific allergens that could be triggering your asthma symptoms.
- Bronchial Provocation Tests: In cases where spirometry results are inconclusive, bronchial provocation tests (e.g., methacholine challenge) may be used to assess airway responsiveness.
- Chest X-rays or CT Scans: These imaging studies may be ordered to rule out other lung conditions that could mimic asthma symptoms.
Diagnosing Allergic Rhinitis:
- Medical History: As with asthma, a detailed medical history is essential. Describe your symptoms, their duration, any seasonal patterns, and factors that worsen or alleviate your symptoms.
- Physical Examination: A healthcare provider may perform a physical examination to check for signs such as nasal congestion, redness or swelling of the nasal passages, or throat irritation.
- Allergy Testing: Allergic rhinitis is often diagnosed through allergy testing. Skin prick tests or blood tests (e.g., RAST or ImmunoCAP) can help identify specific allergens that trigger your symptoms.
- Nasal Endoscopy: In some cases, a nasal endoscopy may be performed, where a thin, flexible tube with a camera is inserted into the nasal passages to visualize any abnormalities.
- Imaging Studies: Imaging studies like CT scans may be ordered if there is suspicion of complications or other underlying conditions.
- Response to Treatment: If there is uncertainty about the diagnosis, a healthcare provider may prescribe allergy medications (e.g., antihistamines or nasal corticosteroids) to see if they alleviate your symptoms. Improvement with treatment can further support the diagnosis.
Consult a healthcare professional for a proper diagnosis, as both asthma and allergic rhinitis have overlapping symptoms with other conditions. Additionally, accurate diagnosis is crucial for developing an appropriate treatment plan tailored to your specific needs. If you suspect you have either condition, seek medical evaluation and guidance.
Treatment Approaches for Asthma and Allergic Rhinitis
The treatment approaches for asthma and allergic rhinitis vary, as these conditions affect different parts of the respiratory system and have distinct management strategies.
Here’s an overview of the treatment options for each condition:
Treatment Approaches for Asthma:
- Medications:
- Bronchodilators: These medications help ease breathing by relaxing airways. Short-acting bronchodilators provide quick relief during asthma attacks, while long-acting bronchodilators provide sustained relief.
- Inhaled Corticosteroids: These anti-inflammatory drugs reduce airway inflammation and help prevent asthma symptoms. They are often used as a long-term controller medication.
- Combination Inhalers: Some inhalers combine bronchodilators and corticosteroids to provide both immediate relief and long-term control.
- Leukotriene Modifiers: These medications block leukotrienes, which play a role in inflammation and asthma symptoms.
- Biologics: In severe cases of asthma, biologic drugs targeting specific immune pathways may be prescribed.
- Inhalers: Inhalers, also known as metered-dose inhalers (MDIs) or dry powder inhalers (DPIs), are devices used to deliver medication directly into the airways for quick relief or long-term control.
- Lifestyle Management:
- Asthma Action Plan: Develop a personalized asthma action plan with your healthcare provider to monitor symptoms and know when to adjust medications.
- Identify and Avoid Triggers: Recognize and minimize exposure to asthma triggers, such as allergens, smoke, and pollution.
- Regular Exercise: Exercise can improve both lung health and overall wellness. Consult with your healthcare provider on which exercises may best benefit your lungs.
- Smoking Cessation: If you smoke, quitting is essential, as smoking can worsen asthma symptoms.
- Stress Management: Reducing stress through relaxation techniques can help prevent asthma exacerbations.
Treatment Approaches for Allergic Rhinitis:
- Medications:
- Antihistamines: These drugs block the action of histamines, reducing symptoms like sneezing, itching, and runny nose.
- Nasal Corticosteroids: These medications reduce nasal inflammation and congestion and are often considered the most effective treatment for allergic rhinitis.
- Decongestants: These drugs provide temporary relief from nasal congestion but should be used sparingly and under the guidance of a healthcare provider to avoid rebound congestion.
- Leukotriene Modifiers: In some cases, leukotriene modifiers may be prescribed to manage allergic rhinitis symptoms.
- Allergen Avoidance:
- Identify and minimize exposure to allergens that trigger your symptoms, such as pollen, dust mites, or pet dander.
- Implement measures like using air purifiers, keeping windows closed during high pollen seasons, and using allergen-proof covers on pillows and mattresses.
- Immunotherapy (Allergy Shots): In cases of severe or uncontrolled allergic rhinitis, allergen immunotherapy may be recommended. This treatment involves gradually exposing the patient to allergens to desensitize the immune system.
- Nasal Irrigation: Saline nasal irrigation using a neti pot or nasal spray can help rinse out allergens and relieve nasal congestion.
- Lifestyle Modifications: Maintain overall health through a balanced diet, regular exercise, and stress management to help reduce allergic rhinitis symptoms.
- Prescription Medications: In cases of severe allergic rhinitis, prescription medications or combination therapies may be considered under the guidance of a healthcare provider.
It’s essential to work closely with your healthcare provider to determine the most appropriate treatment plan for your specific condition, considering its severity, triggers, and individual factors. An individualized approach to management can help control symptoms and improve your quality of life for both asthma and allergic rhinitis.
Preventing Asthma and Allergic Rhinitis Flare-ups
Preventing asthma and allergic rhinitis flare-ups involves a combination of strategies, including allergen avoidance, medication management, and lifestyle adjustments.
Here are some tips to help minimize the risk of flare-ups for both conditions:
Preventing Asthma Flare-ups:
- Identify and Avoid Triggers:
- Determine your asthma triggers through allergen testing and observation. Common triggers include allergens like pollen, dust mites, pet dander, smoke, and pollutants.
- Take proactive steps to minimize exposure to identified triggers. For example, use allergen-proof covers on pillows and mattresses, maintain a clean indoor environment, and avoid smoking or exposure to secondhand smoke.
- Adhere to Medication Plans:
- Follow your healthcare provider’s prescribed asthma action plan, which may include daily controller medications and quick-relief (rescue) medications.
- Ensure you have an adequate supply of medications and use them as directed, even when you feel well, to maintain control and prevent exacerbations.
- Regular Monitoring:
- Keep track of your asthma symptoms and peak flow measurements as advised by your healthcare provider.
- Adjust medication doses as directed by your healthcare provider based on your symptoms and peak flow readings.
- Flu and Pneumonia Vaccination:
- Get annual influenza (flu) vaccines and consider the pneumococcal vaccine to reduce the risk of respiratory infections that can trigger asthma exacerbations.
- Exercise Safely:
- If exercise triggers your asthma, discuss a safe and effective exercise plan with your healthcare provider.
- Use your bronchodilator inhaler before exercise as prescribed.
- Stress Management:
- Practice stress-reduction techniques, as stress can worsen asthma symptoms. Relaxation exercises, mindfulness, and yoga may be helpful.
Preventing Allergic Rhinitis Flare-ups:
- Allergen Avoidance:
- Identify your specific allergens through allergy testing (e.g., skin tests or blood tests).
- Take measures to minimize exposure to allergens:
- Keep windows closed during high pollen seasons.
- Use air purifiers with HEPA filters in your home.
- Wash bedding regularly in hot water to control dust mites.
- Implement pet allergen reduction strategies if you have pets.
- Medication Adherence:
- Take prescribed allergy medications, such as antihistamines and nasal corticosteroids, as directed by your healthcare provider.
- Start medications before the allergy season begins, especially if you have seasonal allergic rhinitis.
- Nasal Irrigation:
- Consider saline nasal irrigation to flush out allergens and reduce congestion.
- Immunotherapy:
- Discuss allergen immunotherapy (allergy shots) with your healthcare provider if your symptoms are severe or not well-controlled with medications.
- Lifestyle Modifications:
- Maintain a healthy lifestyle with a balanced diet and regular exercise to support overall immune health.
- Stay well-hydrated to keep mucous membranes moist.
- Limit Outdoor Activities During High Allergen Levels:
- Check local pollen counts and plan outdoor activities accordingly, reducing exposure during high pollen days.
- Vacuum and Clean Regularly:
- Use a vacuum cleaner with a HEPA filter to reduce allergens in your home.
- Keep living spaces clean and dust-free.
Remember to work closely with your healthcare provider to develop a personalized plan for managing asthma and allergic rhinitis. Regular check-ups and communication with your healthcare team are crucial for effective prevention and management of flare-ups for both conditions.
When to Seek Medical Help
Knowing when to seek medical help for asthma and allergic rhinitis is crucial to effectively manage these conditions and prevent serious complications. Here are guidelines for when to seek medical assistance for each condition:

Asthma:
- Severe Symptoms: If you experience severe asthma symptoms, such as extreme shortness of breath, inability to speak in full sentences, or bluish lips or nails, seek immediate medical attention. These are signs of a severe asthma attack that requires urgent treatment.
- Uncontrolled Symptoms: If your asthma symptoms are not responding to your prescribed rescue inhaler or are getting worse despite using it, contact your healthcare provider promptly.
- Frequent Use of Rescue Inhaler: If you find yourself using your rescue inhaler frequently, such as more than twice a week for symptom relief, this indicates poor asthma control and should prompt a discussion with your healthcare provider to adjust your treatment plan.
- Nighttime Symptoms: If asthma symptoms frequently disrupt your sleep or occur at night, it may be a sign that your asthma is not well-controlled.
- Sudden Onset of Symptoms: If you experience a sudden onset of wheezing, coughing, or difficulty breathing, especially if you have a history of asthma, seek medical attention to rule out an asthma exacerbation or other respiratory conditions.
- Exacerbation Triggers: If you are exposed to known asthma triggers, such as allergens, respiratory irritants, or infections, and your symptoms worsen, consult your healthcare provider for guidance.
Allergic Rhinitis:
- Severe Symptoms: If you have severe allergic rhinitis symptoms that are not relieved by over-the-counter medications or prescribed treatments, consult your healthcare provider.
- Chronic or Persistent Symptoms: If allergic rhinitis symptoms persist for an extended period, consult your healthcare provider for a review of your treatment plan and potential adjustments.
- Complications: Seek medical help if you develop complications of allergic rhinitis, such as sinusitis (sinus infections) or ear infections, which may require antibiotic treatment.
- Unusual or Atypical Symptoms: If you experience unusual symptoms such as bloody nasal discharge, facial pain, or persistent headaches, it’s essential to consult a healthcare provider to rule out other conditions.
- Ineffectiveness of Medications: If prescribed medications do not provide relief or if you experience side effects, discuss this with your healthcare provider to explore alternative treatment options.
- Exacerbations: Be aware of situations that trigger or worsen your allergic rhinitis, such as exposure to specific allergens or environmental changes, and seek medical advice if your symptoms worsen during these times.
Remember that early intervention and effective management can help prevent complications and improve your quality of life for both asthma and allergic rhinitis. It’s important to maintain regular follow-ups with your healthcare provider to monitor your condition and make any necessary adjustments to your treatment plan.
Similarities Between Asthma and Allergic Rhinitis
Asthma and allergic rhinitis, while distinct respiratory conditions, share several similarities:
- Allergic Triggers: Both conditions are often triggered or exacerbated by allergens. Common allergens for both asthma and allergic rhinitis include pollen, dust mites, pet dander, mold spores, and certain foods.
- Inflammatory Response: Both conditions involve an immune system response that leads to inflammation in the respiratory system. In asthma, this inflammation occurs in the lower airways (bronchi), while in allergic rhinitis, it primarily affects the upper airways (nasal passages).
- Airway Hyperresponsiveness: Individuals with both asthma and allergic rhinitis may experience heightened sensitivity of the airways, leading to exaggerated reactions to irritants and allergens.
- Shared Symptoms: There is overlap in symptoms between the two conditions. For instance, both may cause coughing, especially at night or in response to triggers, and can lead to fatigue or disrupted sleep.
- Coexistence: It’s not uncommon for individuals to have both asthma and allergic rhinitis simultaneously. This coexistence is referred to as “allergic asthma” and can result in more complex and interconnected symptom management.
- Treatment Strategies: While the specific medications and management plans may differ, the overall approach to managing both conditions includes allergen avoidance, medication management, and lifestyle adjustments.
- Impact on Quality of Life: Both asthma and allergic rhinitis can significantly impact an individual’s quality of life due to symptoms such as coughing, difficulty breathing, and sleep disruption.
- Seasonal Variations: In some cases, both conditions may exhibit seasonal patterns. For example, pollen allergies can trigger both allergic rhinitis and asthma symptoms during specific times of the year.
It’s important to recognize these similarities, as they underscore the need for comprehensive care and a coordinated approach when managing individuals with both asthma and allergic rhinitis. Accurate diagnosis and a tailored treatment plan are essential to effectively address the unique needs and challenges associated with each condition, whether they coexist or occur independently.
Conclusion
Asthma and Allergic rhinitis are both common respiratory conditions that can significantly impact one’s quality of life. Asthma involves chronic airway inflammation and narrowing, leading to symptoms like wheezing and shortness of breath. Allergic rhinitis, on the other hand, is characterized by inflammation of the nasal passages, causing symptoms such as sneezing and nasal congestion. While these conditions have distinct characteristics, they often coexist and share some triggers, making accurate diagnosis and management essential.
Effective management strategies, including medication, allergen avoidance, and lifestyle adjustments, can help individuals with asthma and allergic rhinitis lead healthier lives with fewer symptoms and fewer exacerbations. Regular communication with healthcare providers and adherence to treatment plans are key to achieving optimal control and preventing complications.



