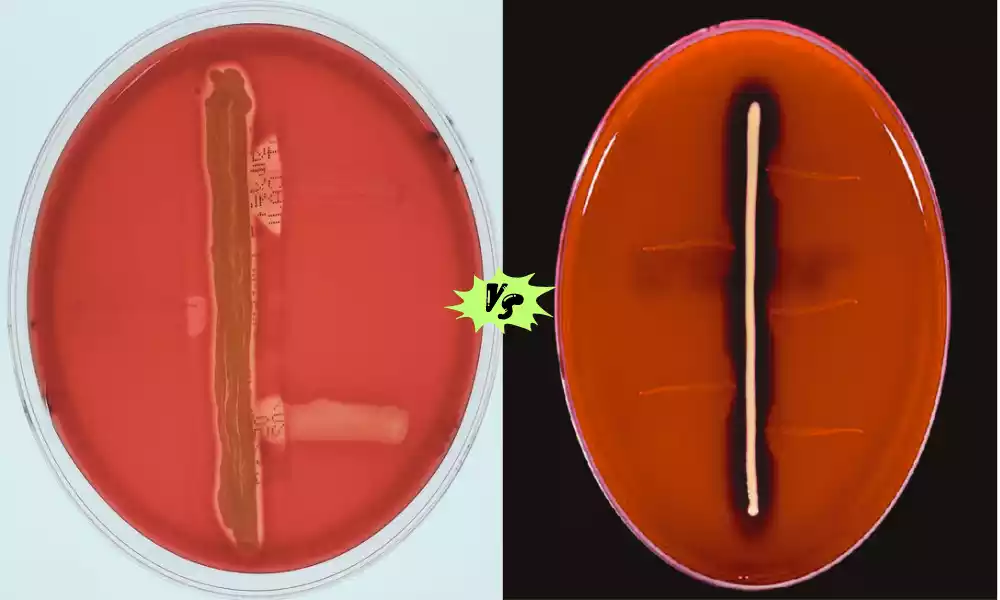
The CAMP and Reverse CAMP tests are two diagnostic tools used in microbiology to identify specific bacterial species within the Streptococcus genus. These tests are valuable in distinguishing between different types of streptococci, particularly Streptococcus agalactia (Group B Streptococcus or GBS) and other beta-hemolytic streptococci. While both tests share a common goal of bacterial differentiation, they employ distinct methodologies and have unique clinical applications. We will briefly introduce the CAMP and Reverse CAMP tests, highlighting their fundamental differences and clinical significance.
What is CAMP Test?

The CAMP test, or Christie-Atkins-Munch-Petersen test, is a laboratory diagnostic method used to identify the presence of a specific bacterium, Streptococcus agalactiae (commonly known as Group B Streptococcus or GBS), in clinical samples. This test is primarily employed in microbiology to differentiate between different beta-hemolytic streptococcal species, particularly S. agalactiae, which can have significant clinical implications.
In the CAMP test, a culture of the test organism (usually Staphylococcus aureus) and the target bacterium (S. agalactiae) are streaked together on a blood agar plate. If S. agalactiae is present, it produces a protein called the CAMP factor, which synergizes with a diffusible factor produced by Staphylococcus aureus.
This synergistic interaction results in enhanced hemolysis, creating a characteristic arrowhead-shaped zone of clearing where the two streaks intersect. This formation of the arrowhead is indicative of a positive CAMP test, confirming the presence of S. agalactiae in the sample.
The CAMP test is particularly useful in clinical settings, especially for pregnant women, as GBS is a leading cause of neonatal infections and can also cause serious illnesses in adults.
Identifying and promptly treating GBS infections in pregnant women can prevent neonatal transmission and related complications. The CAMP test plays a crucial role in the early detection and management of GBS infections, ensuring better maternal and neonatal health outcomes.
Principle Behind CAMP Test
- CAMP test stands for Christie-Atkins-Munch-Petersen test.
- It’s used to identify Streptococcus agalactiae (Group B Streptococcus or GBS) in clinical samples.
- The test is based on synergistic hemolysis, an interaction between two bacterial species.
- S. agalactiae produces a protein called the CAMP factor.
- Staphylococcus aureus, another bacterium used in the test, produces a diffusible substance.
- When both S. agalactiae and S. aureus are cultured together on a blood agar plate:
- The CAMP factor from S. agalactiae interacts with the diffusible substance from S. aureus.
- This interaction leads to enhanced hemolysis at their intersection.
- The result is an arrowhead-shaped zone of clearing on the plate.
- The presence of this arrowhead pattern indicates a positive CAMP test, confirming the presence of S. agalactiae.
What is Reverse CAMP Test?
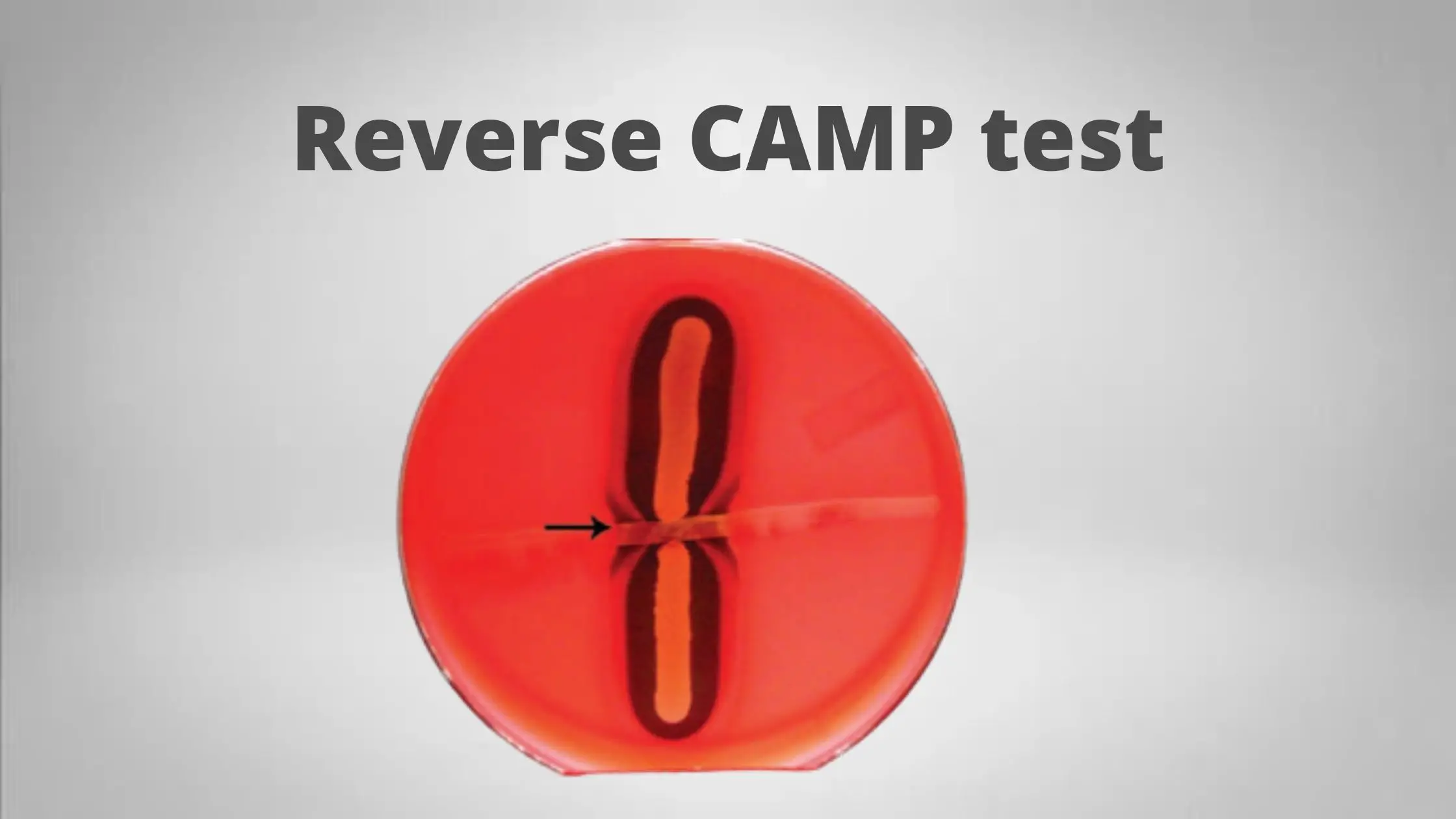
The Reverse CAMP test, also known as the Streptococcus agalactiae (Group B Streptococcus or GBS) differentiation test, is a laboratory technique used to distinguish S. agalactiae from other beta-hemolytic streptococci, particularly Streptococcus dysgalactiae subsp. equisimilis. Unlike the standard CAMP test where S. agalactiae enhances hemolysis, in the Reverse CAMP test, S. agalactiae inhibits the hemolytic activity of S. dysgalactiae subsp. equisimilis.
The principle of the Reverse CAMP test involves streaking two bacterial cultures, S. agalactiae and S. dysgalactiae subsp. equisimilis, perpendicular to each other on a blood agar plate. If S. agalactiae is present, it produces an inhibitory substance that interferes with the hemolysis induced by S. dysgalactiae subsp. equisimilis.
This interference results in a characteristic inverted arrowhead-shaped zone of reduced or inhibited hemolysis where the two bacterial streaks intersect. The formation of this inverted arrowhead pattern is indicative of a positive Reverse CAMP test, confirming the presence of S. agalactiae and distinguishing it from other beta-hemolytic streptococci.
The Reverse CAMP test is clinically valuable, especially where differentiating between S. agalactiae and S. dysgalactiae subsp. equisimilis is crucial for appropriate patient management and treatment decisions. This test aids healthcare professionals in accurately identifying the specific strain of bacteria responsible for an infection, allowing for targeted therapy and improved patient outcomes.
How Does Reverse CAMP Test Work?
The Reverse CAMP test is used to differentiate Streptococcus agalactiae (Group B Streptococcus or GBS) from other beta-hemolytic streptococci, particularly Streptococcus dysgalactiae subsp. equisimilis. It works by assessing the inhibitory effect S. agalactiae has on the hemolysis caused by S. dysgalactiae subsp. equisimilis. Here’s how it works:
- Bacterial Cultures: Two bacterial cultures, S. agalactiae and S. dysgalactiae subsp. equisimilis, are streaked perpendicularly to each other on a blood agar plate.
- Inhibitory Interaction: If S. agalactiae is present, it releases an inhibitory substance that interferes with the hemolytic activity of S. dysgalactiae subsp. equisimilis.
- Distinct Pattern: This interference results in a unique inverted arrowhead-shaped zone of reduced or inhibited hemolysis at the intersection of the two bacterial streaks.
- Positive Test: The formation of this inverted arrowhead pattern indicates a positive Reverse CAMP test, confirming the presence of S. agalactiae and distinguishing it from other beta-hemolytic streptococci.
The test is valuable for clinical purposes, helping healthcare professionals identify the specific bacterial strain causing an infection, enabling targeted treatment strategies for improved patient care.
Significance of CAMP and Reverse CAMP Tests
The CAMP and Reverse CAMP tests hold significant importance in microbiology and clinical diagnostics:
- CAMP Test Significance:
- Identification of Group B Streptococcus (GBS): The CAMP test is crucial for detecting GBS, especially in pregnant women. GBS can cause serious infections in newborns, and early identification allows for preventive measures during childbirth.
- Neonatal Health: Timely detection through the CAMP test helps prevent GBS-related neonatal infections, reducing morbidity and mortality in newborns.
- Guiding Antibiotic Therapy: Positive CAMP test results in pregnant women prompt antibiotic prophylaxis during labor, significantly reducing the risk of GBS transmission to infants.
- Reverse CAMP Test Significance:
- Distinguishing S. agalactiae from Other Streptococci: The Reverse CAMP test is invaluable in differentiating S. agalactiae from other beta-hemolytic streptococci like S. dysgalactiae subsp. equisimilis, ensuring accurate diagnosis and appropriate treatment.
- Patient Care Precision: Accurate identification through the Reverse CAMP test aids in targeted antibiotic therapy, improving patient outcomes and reducing the risk of complications.
Both tests play critical roles in ensuring the health and well-being of newborns, pregnant women, and other patients by guiding appropriate medical interventions and contributing to overall healthcare quality.
Applications in Microbiology
The CAMP and Reverse CAMP tests have several important applications in the field of microbiology:
CAMP Test Applications:
- Identification of Group B Streptococcus (GBS): The primary use of the CAMP test is to identify GBS (Streptococcus agalactiae) in clinical samples, especially in pregnant women.
- Neonatal Health: This test is crucial for assessing the risk of GBS transmission to newborns during childbirth, allowing for appropriate preventive measures and antibiotic prophylaxis.
- Microbiological Research: In research settings, the CAMP test can be used to study hemolysis and synergistic interactions between different bacterial species.
Reverse CAMP Test Applications:
- Distinguishing Streptococcus Species: The Reverse CAMP test is specifically employed to differentiate S. agalactiae from other beta-hemolytic streptococci, such as Streptococcus dysgalactiae subsp. equisimilis.
- Clinical Microbiology: It is vital for accurate identification in clinical microbiology, ensuring the appropriate diagnosis and treatment of bacterial infections caused by S. agalactiae.
- Antibiotic Stewardship: The test contributes to antibiotic stewardship efforts by guiding the selection of targeted antibiotics, reducing the unnecessary use of broad-spectrum antibiotics.
Both tests have clinical applications that impact patient care, particularly in maternal and neonatal health, as well as broader implications for microbiological research and the responsible use of antibiotics.
Performing CAMP and Reverse CAMP Tests
Performing the CAMP and Reverse CAMP tests:
CAMP Test:
- Streak S. agalactiae and S. aureus perpendicularly on a blood agar plate.
- Incubate at 35-37°C for 18-24 hours.
- Look for an arrowhead-shaped zone of enhanced hemolysis.
- Positive result: Arrowhead present, indicating S. agalactiae.
Reverse CAMP Test:
- Streak S. dysgalactiae subsp. equisimilis and S. agalactiae on a blood agar plate.
- Incubate at 35-37°C for 18-24 hours.
- Look for an inverted arrowhead-shaped zone of reduced hemolysis.
- Positive result: Inverted arrowhead present, confirming S. agalactiae.
Comparison table of CAMP and Reverse CAMP Test
Here’s a comparison table of the CAMP and Reverse CAMP tests:
| Aspect | CAMP Test | Reverse CAMP Test |
|---|---|---|
| Purpose | Identifying Streptococcus agalactiae (GBS) | Distinguishing S. agalactiae from other streptococci |
| Principle | Enhanced hemolysis by GBS when interacting with S. aureus | Inhibition of hemolysis in S. dysgalactiae subsp. equisimilis by S. agalactiae |
| Result Interpretation | Positive: Arrowhead-shaped zone of enhanced hemolysis | Positive: Inverted arrowhead-shaped zone of reduced hemolysis |
| Clinical Application | Identifying GBS in clinical samples, neonatal health, antibiotic prophylaxis in pregnancy | Species differentiation, accurate identification in clinical microbiology |
| Specificity | Identifies GBS but not other streptococcal species | Distinguishes S. agalactiae from other beta-hemolytic streptococci |
| Limitations | May produce false negatives, requires specific growth conditions | May produce false negatives, specialized use, skill-dependent |
| Future Prospects | Improved specificity, automation, point-of-care applications | Improved specificity, automation, point-of-care applications, molecular techniques, antibiotic stewardship, global health impact |
This table highlights the key differences and similarities between the two tests, including their purposes, principles, interpretation of results, clinical applications, specificity, limitations, and future prospects.
Advantages and Limitations
Advantages of CAMP Test:
- Rapid Detection: Quickly identifies Group B Streptococcus (GBS) in clinical samples.
- Neonatal Health: Preventing GBS-related illnesses in infants is of utmost importance.
- Guided Treatment: Guides appropriate antibiotic prophylaxis during labor for pregnant women.
Limitations of CAMP Test:
- Specificity: Primarily identifies GBS but does not differentiate other streptococcal species.
- False Negatives: May produce false-negative results if conditions for hemolysis are not optimal.
- Requires Expertise: Proper technique and interpretation are essential, which may require training.
Advantages of Reverse CAMP Test:
- Species Differentiation: Accurately distinguishes S. agalactiae from other beta-hemolytic streptococci.
- Targeted Therapy: Guides specific antibiotic treatment based on accurate identification.
Limitations of Reverse CAMP Test:
- Specialized Use: Specific to identifying S. agalactiae, limiting its broader applications.
- False Negatives: As with the CAMP test, may produce false negatives if conditions are not optimal.
- Skill Dependent: Requires skilled laboratory personnel for accurate execution.
Troubleshooting Common Issues
Common CAMP Test Issues:
- No Arrowhead Formation (Negative Result): Ensure proper streaking and ideal growth conditions.
Common Reverse CAMP Test Issues:
- No Inverted Arrowhead Formation (Negative Result): Verify correct streaking and optimal growth conditions.
- Unclear Result: Ensure well-defined hemolysis zones for clear interpretation.
- Contamination Issues: Practice aseptic techniques and confirm culture purity.
- Inconsistent Results: Standardize incubation conditions and use reliable bacterial cultures.
- Quality Control Failure: Regularly perform quality control tests.
- Technical Error: Follow the protocol meticulously and double-check reagents and incubation conditions.
Future Prospects
The future prospects for the CAMP and Reverse CAMP tests, as well as related diagnostic methods in microbiology, are promising:
- Enhanced Specificity: Ongoing research aims to improve the specificity of these tests to accurately identify various strains and species within the Streptococcus genus, contributing to more targeted treatments.
- Automation: Automation of these tests can increase efficiency, reduce human error, and make them more accessible for routine clinical diagnostics.
- Point-of-Care Testing: The development of rapid point-of-care versions of these tests could revolutionize diagnosis and treatment decisions, particularly in resource-limited settings.
- Advanced Molecular Techniques: Advances in molecular biology, such as PCR-based assays, may complement or replace traditional tests, offering even greater accuracy and specificity.
- Antibiotic Stewardship: These tests will continue to play a crucial role in antibiotic stewardship efforts, ensuring the judicious use of antibiotics and helping combat antibiotic resistance.
- Global Health Impact: As the significance of neonatal and maternal health is recognized worldwide, these tests will remain essential tools in reducing the impact of Streptococcus-related infections on global health.
The future of CAMP and Reverse CAMP tests is bright, with ongoing research and technological advancements set to enhance their accuracy, accessibility, and clinical utility. These tests will continue to be vital in the field of microbiology and clinical diagnostics.
Final Opinion
The CAMP and Reverse CAMP tests, while currently valuable diagnostic tools, have promising futures with advancements in specificity, automation, point-of-care applications, molecular techniques, and their continued role in global health and antibiotic stewardship.