Introduction of Compact and Cancellous Bone
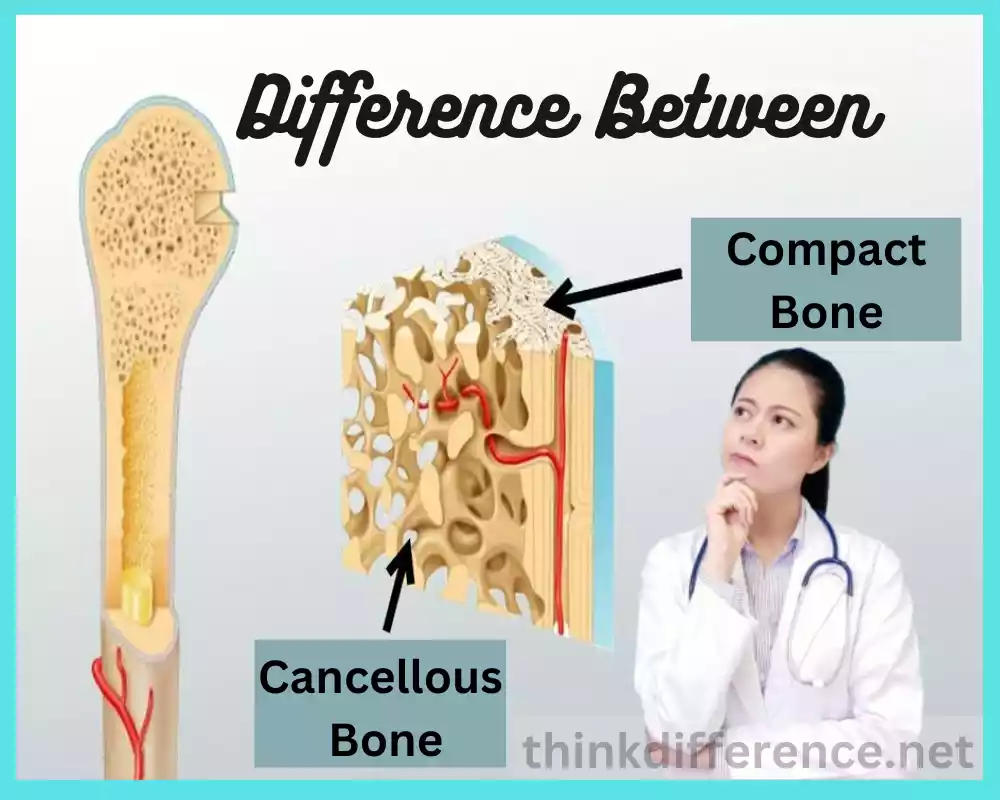
Each type of bone tissue possesses specific properties and functions. There are two major categories of this tissue – Cancellous bone and Compact bone. Both varieties differ significantly in structure, location, and composition while serving various roles within our bodies.
Compact Bone: Compact bone is the outer layer of most bones found within humans and serves to give strength and protection to structures beneath. Compact bones bear weight while withstanding mechanical stress.
Cancellous Bone: Cancellous bones form the innermost layer of bone structure. Characterized by porous and porous structures with interconnected trabeculae arranged lattice-style framework, cancellous bone helps provide flexibility while simultaneously acting as shock absorption for shock-resistant bodies.
Understanding the difference between cancellous and compact bone is critical for comprehending how complex bone structures operate. These differences include microscopic structures, locations within bones, composition of tissues within each type, composition, functions, and clinical significance – offering researchers and medical practitioners insight into bone formation processes like remodeling or fracture healing by studying these unique characteristics of each type.
As we move through each section, we will investigate the characteristics of cancellous and compact bone tissues – their structure, function, location, microscopic details, blood supply, healing abilities, and clinical implications will be addressed. You’ll gain more knowledge regarding their similarities and distinctions and discover how both types contribute towards maintaining the integrity of skeletal systems.
What is Compact Bone?
Compact bone or cortical bone as it’s commonly referred to is one of two major forms of human skeletal structure bone tissue types. As its outermost layer, it provides support and strength to our bodies.
Characteristics of Compact Bone:
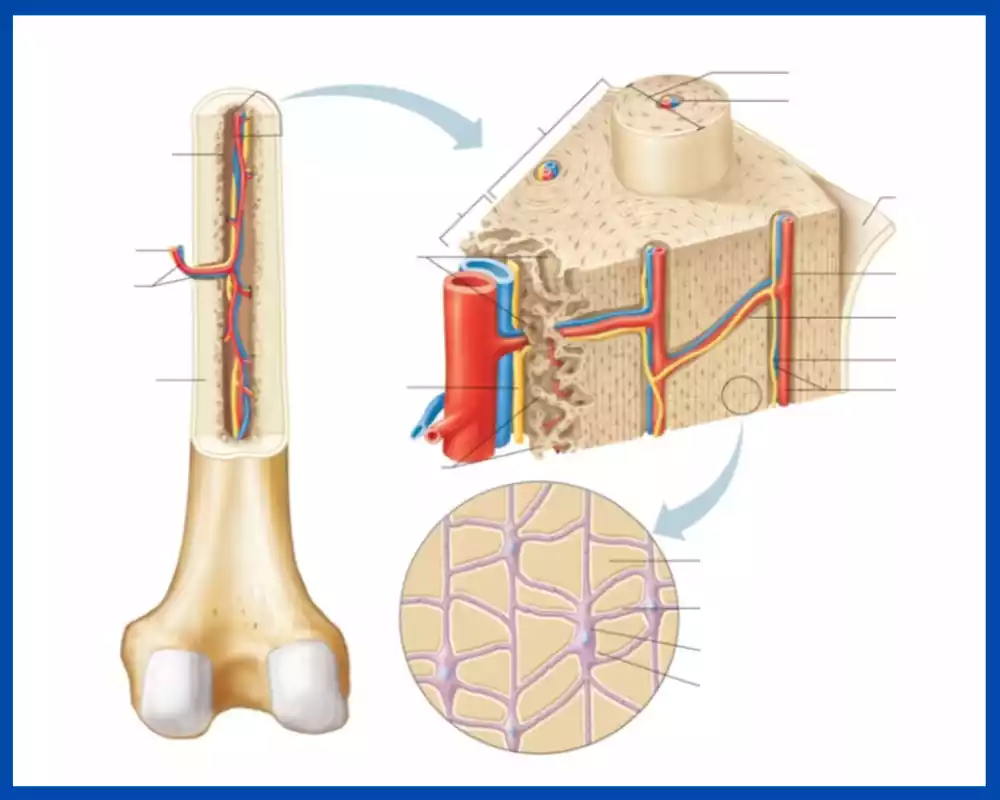
- Structure: Compact bone is characterized by its tightly packed, solid structure. It appears solid to the naked eye and forms a smooth, hard surface. It is the more rigid and dense of the two bone types.
- Microscopic Units: The basic structural unit of compact bone is called an osteon, also known as a Haversian system. Osteons are cylindrical structures that run parallel to the long axis of the bone. Each osteon consists of concentric layers of bone tissue called lamellae, which surround a central canal known as the Haversian canal. The Haversian canal contains blood vessels, nerves, and connective tissue.
- Lamellae: The lamellae in compact bone are composed of collagen fibers and mineralized calcium salts, primarily hydroxyapatite. These lamellae provide strength and rigidity to the bone tissue.
- Osteocytes and Canaliculi: Within the lamellae, there are small spaces called lacunae, which house mature bone cells called osteocytes. These osteocytes maintain the bone tissue and communicate with each other and with blood vessels through tiny channels called canaliculi. This network of canaliculi allows for the exchange of nutrients and waste products between osteocytes and blood vessels.
- Function: Compact bone serves several important functions. It provides mechanical strength and rigidity to the skeleton, allowing for weight-bearing and locomotion. The ribcage and skull provide essential protection to vital organs like the heart, lungs, and brain. Compact bone acts as a reservoir for minerals primarily calcium and phosphorus which are released into the bloodstream for different physiological uses.
Compact bone is the outer layer of most bones in our bodies and serves to strengthen, protect and provide support. Microscopic structures within compact bones contribute significantly to their strength, for instance, lamellae and canaliculi structures help make up their strength.
Structure and Composition of Compact Bone
The structure and composition of compact bones are integral to their strength, density, and protective function – let’s delve deeper:
- Lamellar Structure: Compact bone has a laminar or layered structure. It consists of multiple layers called lamellae, which are concentrically arranged around Haversian canals. Lamellae are composed of collagen fibers and mineralized matrix, providing strength and rigidity to the bone.
- Osteons (Haversian Systems): The fundamental structural units of compact bone are called osteons or Haversian systems. Each osteon is a cylindrical structure consisting of concentric lamellae surrounding a central canal called the Haversian canal. The Haversian canal contains blood vessels, lymphatic vessels, nerves, and connective tissue. Osteons are aligned parallel to the long axis of the bone, ensuring efficient weight-bearing and mechanical support.
- Canaliculi and Lacunae: Within the lamellae, small spaces called lacunae house mature bone cells called osteocytes. Osteocytes maintain the bone tissue and exchange nutrients and waste materials through delicate channels called canaliculi. Canaliculi connect neighboring lacunae and provide a means of communication and transportation between osteocytes and the blood supply in the Haversian canals.
- Perforating Canals (Volkmann’s Canals): In addition to the central Haversian canals, compact bone contains smaller channels known as perforating canals or Volkmann’s canals. These canals run perpendicular to the long axis of the bone, connecting adjacent osteons and providing additional pathways for blood vessels, nerves, and connective tissue to traverse the compact bone.
- Composition: The composition of compact bone primarily consists of organic and inorganic components. The organic component comprises approximately 35% of the bone’s weight and includes collagen fibers, which provide flexibility and tensile strength. The inorganic component makes up about 65% of the bone’s weight and is mainly composed of mineralized calcium salts, such as hydroxyapatite. These minerals contribute to the hardness and rigidity of the bone tissue.
The structure and composition of compact bone are central to its strength, durability, and protective capabilities. A complex combination of lamellae, osteons, and canaliculi as well as lacunae and Haversian perforating channels ensure effective nutrient transfer, mechanical support, and resistance to strain and stress.
Functions of Compact Bone
Compact bones serve many essential purposes in our bodies, from providing protection and strength to supporting us when needed. Learn about some of the main functions of compact bones:
- Support of Structure: The compact bone serves to support and shape the physical form, including upright posture, weight-bearing, and movement. As an outermost layer of many bones, it serves to hold together body shape by maintaining shape through maintaining posture, weight-bearing, and mobility.
- Protection of Vital Organs: Compact bones play an integral part in protecting vital organs. The skull contains most of this dense structure to shield the brain while its use as part of the ribcage protects the lungs and heart from harm.
- Mechanical Strength: Compact bone is distinguished by its dense, solid structure which grants it exceptional mechanical strength, making it capable of resisting compression forces while bearing weight without fracture or breaking under load. This strength is essential in supporting both the health of compact bones as well as physical activities.
- Calcium and Mineral Storage: Compact bone acts as an invaluable repository of essential body minerals such as calcium and phosphorus, stored within its matrix to support various physiological functions including muscle contraction, nerve signals, mineral balance maintenance, and more.
- Blood Cell Production: Compact bone contains specific areas with red bone marrow where hematopoiesis occurs (formation of new blood cells). Red marrow stem cells produce red and white blood cells along with platelets; these are vital cells necessary for oxygen transport, immune responses, and blood clotting processes.
- Metabolic Regulation: Compact bones can be subject to metabolic regulation via osteoblasts and osteoclasts, with osteoblasts synthesizing new bone tissue while osteoclasts remove damaged or old tissues, inducing mineral deposition along the way.
- Remodeling and Repair: Compact bones undergo constant remodeling as part of normal body function, adapting their structure in response to mechanical stresses. If any fracture occurs in one of those bones, compact bone helps repair its damage to promote healing while upholding bone integrity.
Compact bone serves many roles within our bodies and the system as a whole providing structural support, protecting organs of primary importance to life functions such as breathing or heartbeats, offering mechanical resistance, storing minerals for blood cell formation and even helping regulate metabolism and bone remodeling and repairs – all contributing to overall health and performance within this vital element of health and function of both bones and bodies alike.
What is Cancellous Bone?
Cancellous (trabecular) bone is one of two primary bone tissues found within the human skeleton and differs significantly from compact in terms of both structure and composition. Cancellous bones typically reside inside compact bone encasings for protection.
Characteristics of Cancellous Bone:
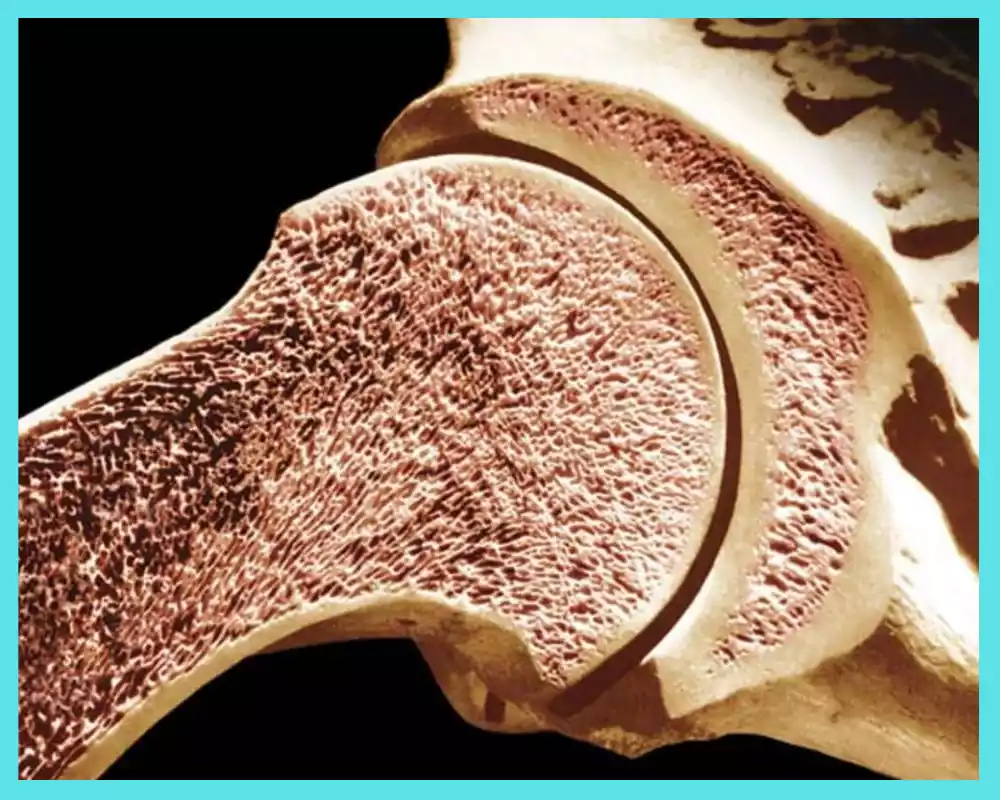
- Porous Structure: Cancellous bone has a spongy or porous structure characterized by a network of interconnected struts or beams called trabeculae. These trabeculae create a lattice-like framework, leaving spaces or cavities between them. The presence of open spaces contributes to the bone’s lightweight nature.
- Composition: Cancellous bone is composed of a combination of collagen fibers, bone cells (osteocytes), and a matrix made up of mineralized calcium salts. Compared to compact bone, cancellous bone has a higher proportion of spaces and a lower proportion of mineralized matrix.
- Trabeculae: Trabeculae are the structural units of cancellous bone. They form a three-dimensional network of interconnected struts, creating a honeycomb-like structure. The arrangement and alignment of trabeculae follow the lines of stress within the bone, providing strength and support while minimizing the weight of the bone.
- Bone Marrow: The spaces between trabeculae in cancellous bone are filled with bone marrow. Red bone marrow, which is responsible for the production of blood cells is predominantly found in the spaces of cancellous bone. Adults typically possess red bone marrow in the cancellous bones of flat bones such as the sternum and pelvis; yellow-hued bone marrow, made up mostly of fat cells, may also be found within central cavities within long bones.
- Flexibility and Shock Absorption: The spongy nature of cancellous bone provides flexibility and shock-absorbing properties. It can absorb impact forces and distribute stresses across the bone, reducing the risk of fractures and injuries.
- Surface Area: Cancellous bone has a significantly larger surface area compared to compact bone. This increased surface area allows for increased metabolic activity, including interactions between bone cells, nutrient exchange, and the deposition or resorption of bone tissue.
- Remodeling: Cancellous bone, like compact bone, undergoes continuous remodeling throughout life. It responds to mechanical stresses and hormonal factors by modifying its structure and density to adapt to changing functional demands.
Cancellous bone tissue is porous and spongy. It features a trabecular pattern. Containing both bone marrow and flexible bones. Absorbing shock well while offering ample surface area for metabolic activity. Whilst compact bone provides primary protection, cancellous bones contribute more actively towards strength, support, and blood cell production within bones themselves.
Structure and Composition of Cancellous Bone
Discover its special properties and functions thanks to its structure and composition. Examine some key aspects of cancellous bones:
- Trabecular Structure: Cancellous bone has a porous or trabecular structure characterized by a network of interconnected struts called trabeculae. These trabeculae form a lattice-like arrangement, leaving spaces or cavities between them. The trabeculae align along the lines of stress, providing strength and support to the bone while minimizing its weight.
- Composition: Cancellous bone is composed of a combination of organic and inorganic components. The organic component includes collagen fibers, which provide flexibility and tensile strength to the bone tissue. Mineralized calcium salts (primarily hydroxyapatite ) comprise the inorganic component. They contribute to bone rigidity and hardness by strengthening it structurally.
- Trabeculae and Bone Marrow: The trabeculae in cancellous bone contain bone marrow-filled spaces. Red bone marrow, responsible for the production of blood cells is predominantly found within these spaces. Red bone tissue is composed of hematopoietic cells which produce red blood cells as well as white blood cells and platelets. Yellow bone marrow, composed mainly of fat cells, may also be present in the central cavities of long bones.
- Increased Surface Area: Cancellous bone has a significantly larger surface area compared to compact bone due to its porous structure. This increased surface area allows for increased metabolic activity, including interactions between bone cells, nutrient exchange, and the deposition or resorption of bone tissue.
- Mechanical Properties: The trabecular structure of cancellous bone provides several mechanical advantages. It enhances the bone’s ability to absorb and distribute forces, making it more resilient to compressive forces and impact. The porous nature of cancellous bone also contributes to its lightweight properties.
- Remodeling: Like compact bone, cancellous bone undergoes constant remodeling throughout life. It responds to mechanical stresses, hormonal signals, and changes in functional demands. Remodeling involves osteoclasts removing bone tissue from within bone structures before deposing new layers of it to adapt its structure and density.
- Vascularization: Cancellous bone is well-vascularized, with blood vessels present within the trabeculae. These blood vessels supply oxygen, nutrients, and regulatory factors necessary for the maintenance and function of the bone tissue.
Astral bones exhibit porous, trabecular structures made up of mineralized calcium salts and collagen fibers. There may also be spaces containing bone marrow. They feature increased surface areas with mechanical properties enabling shock absorption as well as blood cell production functions. These qualities enable their existence within our environment to perform multiple roles including shock absorption.
Functions of Cancellous Bone
Cancellous (spongy) bones serve multiple vital roles within our bodies. Lighter and more porous than compact bone, cancellous bone plays a pivotal role in maintaining homeostasis while supporting skeletal function – We will now explore its main purposes:
- Structural Support: Cancellous bone contributes to the structural support of the skeleton. Although compact bone primarily forms the outer layer of bones, cancellous bone fills the interior, providing structural reinforcement and integrity to the bone. It helps distribute forces and stresses throughout the skeletal system, enhancing overall stability.
- Weight Reduction: Cancellous bone’s porous nature allows for a significant reduction in the weight of bones. This is particularly important in long bones, where the presence of cancellous bone in the metaphysis (the region between the diaphysis and epiphysis) reduces the overall bone weight without compromising strength. The lighter weight contributes to improved mobility and agility.
- Shock Absorption: The trabecular structure of cancellous bone provides excellent shock-absorbing properties. When forces or impacts are applied to the skeleton, the cancellous bone acts as a cushion, dispersing and absorbing the energy. This helps protect the more fragile compact bone and surrounding soft tissues from excessive stress and potential injury.
- Red Blood Cell Production: Cancellous bone contains red bone marrow, which is responsible for the production of red blood cells, white blood cells, and platelets. Hematopoietic stem cells present in the red bone marrow continuously generate new blood cells, ensuring an adequate supply for oxygen transport, immune response, and blood clotting.
- Calcium and Mineral Homeostasis: Cancellous bone plays a role in calcium and mineral homeostasis. It serves as a reservoir for calcium, phosphorus, and other minerals, releasing them into the bloodstream when needed for various physiological processes. The cancellous bone helps regulate blood calcium levels, which are crucial for muscle contraction, nerve function, and other vital functions.
- Metabolic Activity: Cancellous bone exhibits increased metabolic activity compared to compact bone due to its larger surface area and rich vascularization. The bone cells within cancellous bone, including osteoblasts and osteoclasts are involved in the continuous remodeling of the bone tissue, regulating mineral deposition and resorption. This remodeling process helps maintain bone strength, repair microdamage, and adapt to changing mechanical stresses.
The cancellous skeleton plays an essential role in providing structural support, weight reduction, shock absorption and red blood cell production, calcium/mineral homeostasis as well as metabolic activity in our bodies. Porous structures such as bone with red marrow help support overall skeletal functions while simultaneously upholding physiological processes within the body and its physiological processes.
Differences Between Compact and Cancellous Bone
Human skeletons comprise two different kinds of bone tissues – cancellous and compact – both having many similarities but there are also key distinctions that set them apart from one another. Here we examine these key distinctions:
1. Structure and Appearance:
- Compact Bone: Compact Bone (Cortical Bone or Outer Layer Bone) forms the outermost layer of most bones and is comprised of densely packed osteons known as Haversian systems encasing concentric layers enclosing a central Haversian Canal.
- Cancellous Bone: Cancellous Bone, also referred to as trabecular bone or spongy bone is located inside compact bones in the interior region. Trabecular structures like cancellous are distinguished by a network of interconnected struts called trabeculae that connect them; bone marrow fills the spaces between these trabeculae.
2. Composition:
- Compact Bone: Compact bones contain higher percentages of the mineralized matrix than cancellous bones and have less space available between osteons (denser packing of osteons that contain lamellae concentric of collagen fibers and mineralized calcium salts), thus offering increased structural support and protection from injury.
- Cancellous Bone: Cancellous bones feature larger gaps between their cells than compact bone, as well as less mineralization matrix. Cancellous bones consist of trabeculae – networks composed of collagen fibers connected by mineralized matrixes which leave porous structures that fill these spaces with bone marrow.
3. Function:
- Compact Bone: Compact bone primarily serves a protective function, forming the outer layer of bones and providing strength, support, and mechanical rigidity. It resists compressive forces and weight-bearing loads, protecting the internal structures and vital organs.
- Cancellous Bone: Cancellous bone contributes to structural support and weight reduction in bones. Its porous structure provides flexibility, shock absorption, and a larger surface area for metabolic activities. Cancellous bone also houses red bone marrow, which is involved in the production of blood cells.
4. Location:
- Compact Bone: Compact bone is predominantly found in the shafts (diaphysis) of long bones, such as the femur and humerus. It also forms the outer layers of flat bones, such as the skull and ribs.
- Cancellous Bone: Cancellous bone is mainly located in the interior (metaphysis and epiphysis) of long bones, as well as in the vertebrae, sternum, and pelvis. It fills the spaces between the cortical bone and provides support to the overall bone structure.
5. Vascularization:
- Compact Bone: Compact bone has a relatively less extensive network of blood vessels compared to cancellous bone. Blood vessels primarily travel through the Haversian canals within the osteons, supplying nutrients and removing waste products.
- Cancellous Bone: Cancellous bone has a highly vascularized structure with a rich network of blood vessels. Blood vessels run through the spaces between trabeculae, ensuring efficient nutrient exchange and metabolic activity.
Compact bone is comprised of dense material found at the outermost layers, providing strength and protection to bones. Cancellous bones feature lattice structures within bones which contribute to weight loss, metabolic activity, and structural support – both contributing factors which provide essential benefits.
Bone Remodeling Process
Bone remodeling is an ongoing, dynamic process that involves the gradual removal and formation of bone tissue over a person’s lifetime. This highly controlled process maintains bone strength while also helping repair small damage repairs as well as adapt to changing mechanical needs.
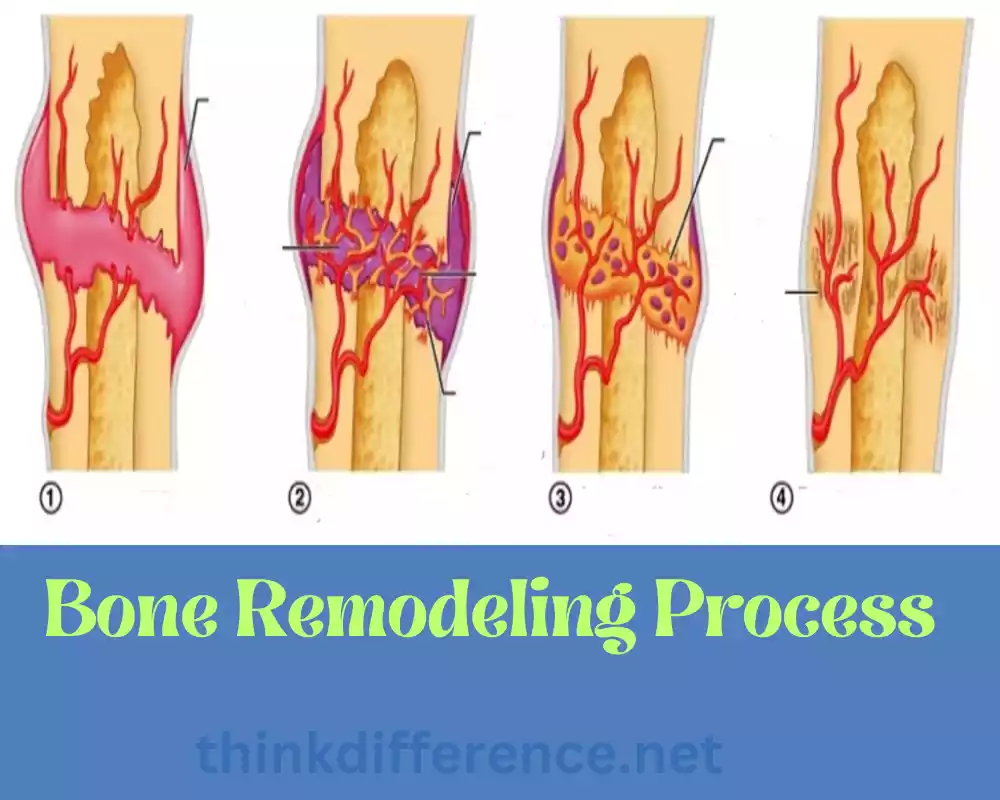
Two cell types play key roles in bone remodeling: Osteoblasts and Osteoclasts.
- Activation: Bone remodeling begins when osteoclasts become active. Various factors mechanical stress, hormones, and cytokines, trigger the activation of osteoclasts.
- Resorption: Once activated, osteoclasts attach to the bone surface and create small pits or cavities called resorption lacunae. They release enzymes and acids that dissolve and break down the mineralized matrix of the bone, liberating calcium and other minerals into the bloodstream. Osteoclasts also play a role in regulating calcium homeostasis.
- Reversal: After bone resorption, the reversal phase begins, during which the resorption site is prepared for bone formation. Osteoblasts, which are responsible for bone formation, are recruited to the resorption site.
- Formation: Osteoblasts synthesize and deposit new bone matrix in the resorption lacunae. They secrete collagen fibers, along with proteins and other substances, which form the unmineralized matrix called osteoid. Osteoblasts then initiate the mineralization process by depositing calcium and other minerals onto the osteoid. The osteoid becomes mineralized, transforming into mature bone tissue.
- Mineralization: Mineralization is the process by which the deposited osteoid is hardened and mineralized with calcium phosphate crystals. This step confers strength and rigidity to the newly formed bone tissue.
- Resting: Following bone formation, some osteoblasts become embedded within the newly formed bone tissue and differentiate into osteocytes. These mature bone cells reside within small spaces called lacunae and maintain communication networks through small channels called canaliculi.
Bone remodeling occurs simultaneously across various sites of the skeleton and is closely managed to maintain homeostasis. It helps repair microdamage caused by everyday activities, redistributes bone mass to accommodate mechanical stressors, releases minerals necessary for physiological processes, and removes old or damaged tissue.
Maintaining bone health requires striking a balance between bone formation and resorption, hormones, growth factors, and other regulatory signals to achieve this objective. Imbalances may lead to disorders like osteoporosis or osteopetrosis if left uncorrected; hormones and growth factor therapies are indispensable tools in helping achieve this aim.
Factors Affecting Bone Health
Various factors influence bone health over time. They may increase or diminish the strength, density, or integrity of bones; understanding these factors is important in maintaining optimal bone health as it prevents osteoporosis from setting in. Here are a few that might affect it:
- Nutrition: Nutrition plays an essential role in supporting bone health. Calcium, phosphorus, and vitamin D all have important functions when it comes to mineralizing and densifying bones; when these vital minerals are deficient, fracture risk increases exponentially. A diet rich in dairy, leafy greens, and fortified food products (in addition to supplements) is key in supporting bone wellness.
- Physical Activity: Exercise is vitally important to bone health. Weight-bearing activities like walking, jogging, and dancing help promote new bone formation while weightlifting or resistance exercises like lifting can promote strength by stressing the bones. A lack of exercise due to inactive lifestyles could result in bone loss.
- Hormonal Factors: Hormones play an integral part in bone health. Women’s estrogen levels play a particularly vital role in maintaining their bone density; subsequent estrogen-low menopausal years increase the risk for osteoporosis as estrogen levels decline and men may also experience testosterone deficit, leading to decreased bone mineralization and loss. Hormone imbalances or medical conditions that alter hormone production could impact this area as well.
- Age: As we get older, bones tend to lose health over time. Bone growth and density peak between childhood and adolescence; by our early 20s peak bone mass has often been reached. Unfortunately, as we get older bone resorption often outpaces formation leading to gradual decreases in density over time; hormonal fluctuations often compound this process more severely for women who have gone through menopause than for others.
- Genetics: Genetic factors play an integral part in bone health. Their genetic makeup determines peak bone mass as well as susceptibility to certain disorders; family histories of fractures or osteoporosis increase an individual’s chances of having these issues, while osteogenesis imperfecta affects the strength and integrity of bones in various ways.
- Medication and health conditions: Certain drugs like corticosteroids and anticonvulsants may interfere with bone metabolism and reduce bone health, potentially worsening osteoarthritis symptoms as well as celiac diseases and eating disorders. Malabsorption issues as well as hormonal imbalances or chronic inflammation could all play a part in bone loss.
- Lifestyle Factors: Smoking, excessive alcohol intake, and caffeine intake all can have negative impacts on bone health. Smoking reduces bone density while interfering with their formation; excessive alcohol intake disrupts remodeling processes as well as calcium absorption processes while caffeine consumption usually has only mild implications on absorption processes.
- Body Mass Index and Weight: Both low body weight and obesity can have detrimental effects on bone health, from decreased density leading to fractures to excessive strain on bones due to obesity resulting in joint problems and eventual breakdown.
Multiple factors can interact and affect bone health. By taking proactive steps such as adopting healthy eating and exercising habits and avoiding harmful behaviors, you can promote and preserve it throughout your lifetime. Having regular check-ups with healthcare providers and discussing any concerns with them about bone health will ensure its maintenance for life.
Common Disorders Affecting Compact and Cancellous Bone
Various conditions may contribute to impairment and abnormalities in bone health and function, most frequently those listed below:
- Osteoporosis: Osteoporosis is a bone condition marked by low bone mass, decreased tissue integrity, and an increase in fracture susceptibility. Osteoporosis affects both compact and cancellous bones in equal measures resulting in decreased strength and density; postmenopausal females may be especially at risk, although anyone may suffer.
- Osteogenesis Imperfecta: Osteogenesis imperfecta (also referred to as Brittle Bone Disease) is a genetic condition in which fragile, easily-breakable bones occur due to abnormalities of collagen proteins essential to bone strength, leading to numerous fractures, deformities, and growth impairment in both compact and cancellous bone tissue.
- Paget’s Disease of Bone: Paget’s is a chronic disorder that leads to abnormal bone remodeling. This abnormal remodeling results from excessive formation and breakdown, leaving structurally abnormal bones. Paget can affect both compact and cancellous bones causing pain, deformities, and increased fracture risk for sufferers – especially older individuals. Paget is more prevalent among these groups.
- Osteomyelitis (bone infection): Osteomyelitis, also referred to as osteomyelitis, is an infectious condition that affects bones. Common causes include bacteria-caused inflammation of both cancellous and compact bone that leads to degradation and reduced strength; severe pain; fever; systemic symptoms may develop rapidly as a result. Therefore osteomyelitis must be identified early and treated quickly with antibiotics for best results.
- Osteopenia: Osteopenia refers to lower than normal bone mineral density that does not yet reach osteoporosis levels, often occurring among cancellous or compact bone types and increasing fracture risks; untreated, it could progress further and develop into osteoporosis.
- Osteomalacia: Osteomalacia occurs when bones soften due to vitamin D deficiency or metabolic issues, impacting both cancellous and compact bone, leading to weak, fragile structures with muscle weakness and bone pain being common symptoms of Osteomalacia as well as increasing fracture risks. This condition affects both cancellous and compact bones and has potential detrimental impacts such as muscle atrophy, decreased fracture risks, and muscle atrophy in general.
- Fibrous Dysplasia: Fibrous dysplasia, a rare genetic condition in which fibrous tissue replaces normal bone and leads to abnormal bone development, may affect both cancellous and compact bone, potentially leading to deformities and fractures; Fibrous Dysplasia may affect either one bone at a time or multiple bones simultaneously.
- Ewing Sarcoma: Ewing Sarcoma (a form of cancerous bone growth), affects most children and young adults between the ages of 2-7. Most often it affects long bones such as the femur or tibia and both compact and cancellous tissue can become affected; both compact and cancellous cells may become cancerous in affected patients; symptoms include pain and swelling to the bone that eventually may result in fractures if untreated.
Here are several disorders that may impact cancellous and compact bone, each condition possessing unique symptoms and treatments. When seeking care, healthcare providers must be involved in accurate diagnosis, management, and treatment of bone-related conditions.
Tips for Maintaining Healthy Bones
Maintaining and promoting bone health is integral to overall well-being, including avoiding conditions like osteoporosis. Here are a few strategies for doing just that:
- Calcium is essential to bone health: Include calcium-rich food sources like dairy products, leafy greens (broccoli kale spinach), plant-based milk fortified with calcium, and other calcium-fortified products in your diet to support it. Please consult with a healthcare provider before making decisions on taking calcium supplements.
- Get Adequate Vitamin D: Vitamin D is vitally important to calcium absorption and bone strength. Spend some time outside enjoying some sun to increase production; add foods containing Vitamin D like fortified dairy, egg yolks, salmon/mackerel/wolfish oil as a staple food source. Vitamin D supplements may be required in areas of low sun exposure or certain medical conditions; fortified milk products provide additional vitamin D benefits as supplements may not.
- Engage in Weight-Bearing Exercises: Weight-Bearing Exercise helps stimulate bone formation and density growth by walking, jogging, and dancing regularly. Strength training should also play an integral part in physical fitness – at least 150 minutes each week of moderate-intensity activity or 75 minutes each week of vigorous-intensity activity along with muscle-strengthening exercises at least twice every month are encouraged for best results.
- Strength Training: Strength training exercises such as weightlifting or resistance training will help maintain and increase bone density. Exercise that target both upper-body movements as well as major muscle groups should be done ideally, starting by lifting lighter weights until strength builds up over time.
- Consume a balanced diet: For bone health, eating plenty of fresh fruits and vegetables as well as whole grains loaded with lean proteins, healthy fats, and lean proteins is crucial. Also make sure your meals include foods rich in vitamin K, magnesium, and phosphorus for maximum bone benefit.
- Reducing Alcohol and Caffeine Consumption: Excessive alcohol intake has the potential to have detrimental effects on bone health, so consume in moderation. Caffeine interferes with calcium absorption so consider restricting how often you drink coffee, tea, or energy drinks as this could interfere with its absorption into your system.
- Avoid Smoking: Smoking can have serious ramifications on bone health. Smoking decreases bone density while increasing fracture risks – harmful both in terms of bone and overall health.
- Maintain a Healthy Weight: Bone health can be compromised when either overweight or underweight individuals consume an unbalanced diet and fail to engage in sufficient physical activity, so making wise food and fitness choices will go far toward keeping you at an ideal weight. When necessary, consult a health provider in developing an appropriate plan.
- Prevent Falls: Be mindful to prevent falls. Take steps to safeguard against them if you’re an older adult more vulnerable to fractures; such as using handrails in your home and eliminating trip hazards with proper lighting as well as wearing appropriate footwear for better balance and coordination to lower the risks of falling.
Exercising regularly may also help strengthen balance and coordination and decrease the risks of falling. If you are concerned or at risk of osteoporosis, speaking to your healthcare provider about regular bone density screenings will allow them to assess your bone health and determine any further interventions or treatments required.
Care for your bones at any age is never too late or too soon. These tips will ensure they stay strong, healthy, and resilient throughout your lifetime.
Importance of Nutrition for Bone Health
Nutrition plays an integral part in supporting bone health. A proper intake of essential nutrients is critical to supporting the development, strength, and growth of bones. Deficiencies can weaken them further increasing fracture risks. Nutrition plays a key role in supporting bone well-being.
- Calcium: Calcium is an essential element to bone strength. Consuming enough calcium will ensure strong bones, as insufficient consumption could cause your body to withdraw calcium from bones over time causing bone density loss. Calcium supplements or foods rich in calcium will ensure you’re receiving enough of this essential mineral to ensure bone health is preserved.
- Vitamin D: Vitamin D is vital in calcium absorption and utilization. It regulates calcium levels within the body while helping incorporate phosphorus into bone matrix formation, with insufficient levels leading to impaired calcium absorption, reduced mineralization of bones, fracture risk increases as well as bone loss risk. Obtaining adequate amounts can be achieved through diet or supplement consumption rich in Vitamin D.
- Vitamin K: Vitamin K plays an integral part in bone mineralization by synthesizing and regulating proteins that control it. Osteocalcin is key for binding calcium to bones’ matrix; activated by vitamin K it ensures calcium can be effectively utilized while improving the density and strength of bones. So make sure to include leafy greens, broccoli, or any other source of Vitamin K into your diet!
- Protein: Essential in building bone tissue, proteins provide amino acids needed for bone repair and formation. A diet rich in proteins will support and maintain strong, dense bones while diets low in proteins may reduce density or impair growth. Good sources of proteins include lean meats/poultry/fish/lentils/nuts.
- Phosphorus and Magnesium: Phosphorus and magnesium work alongside calcium to support bone health. Phosphorus forms part of the hydroxyapatite mineral complex that strengthens bones. Magnesium regulates calcium metabolism and impacts the mineralization of bones; adding foods high in these elements (meats, fish dairy) or high in these elements (nuts seeds whole grains, etc) may support optimal bone wellness and help ensure longevity in our lives.
- Micronutrients: Other micronutrients, including zinc, copper, zinc oxide, and vitamins C and A play an essential part in bone health. Vitamin C plays an essential role in collagen synthesis that forms the basis for bone formation while Vitamin A plays an essential part in remodeling bone tissue while zinc and copper aid mineralization of bones. Eating fruits, vegetables, and whole foods to ensure an adequate supply of these essential minerals will ensure an appropriate intake.
- Weight Control and Bone Health: Diet is also integral in managing body weight, which directly benefits bone health. A healthy weight helps alleviate pressure on bones and reduce fracture risk. Eating right will indirectly benefit bone health through indirect means such as weight control.
- Overall Health & Diet: For optimal bone health, general well-being and adequate nutrition are crucially important. Chronic health conditions, nutritional deficiencies, or poor eating habits can compromise bone health – so making sure that you enjoy a nutritious and well-rounded diet that fulfills all your dietary requirements will go far toward supporting strong bones!
Nutritional needs of different life stages vary significantly; while children and adolescents require sufficient nutrients for healthy development, older adults need to focus on maintaining bone density through optimal diet recommendations from healthcare professionals such as registered dietitians or registered dieticians. Consulting an RDN or healthcare specialist for personalized advice regarding optimal bone health could prove extremely valuable.
Exercise and Bone Strength
Exercise can play an essential role in building and strengthening bone strength. Regular physical activity – specifically weight-bearing exercises and resistance training – is especially helpful to stimulate new bone formation while increasing density. Here are three key ways exercise can positively influence bone health:
- Weight-Bearing Workouts: When engaging in weight-bearing workouts, resistance against gravity must be overcome to increase bone mineralization and build bone tissue. Walking, jogging, dancing, hiking or stair climbing are examples of exercises that stimulate osteoblasts to strengthen and build bone mass. Regular participation in weight-bearing workouts will enhance your bone density while decreasing fracture risk.
- Resistance Training: Exercise that incorporates resistance includes lifting weights or resistance bands and performing bodyweight exercises, inducing tension in your muscles to promote bone strength. Resistance training primarily targets specific muscle groups associated with bones. This increases bone stability and strength. Resistance exercises such as these have proven particularly successful at increasing hips and spine density as key areas where fractures often occur in osteoporosis patients.
- Impact and Plyometric Exercises: High-impact movements like jumping, skiing, or certain sports (e.g. basketball and tennis) exert substantial forces on bones. An impact-loading exercise stimulates bone remodeling to increase density while exercises involving powerful muscle contractions can strengthen them further.
- Progressive Overload: Progressive overload can help facilitate bone growth and adaptation through gradual intensification, frequency, or duration increases of exercise. You can challenge both muscles and bones by gradually ramping up intensity, frequency, or duration levels over time. The gradual increase in workload stimulates formation as well as increases bone density.
- Balance and coordination exercises: Maintaining good balance and coordination is integral for avoiding fractures and falls, particularly among older adults. Tai chi and yoga offer great exercises that can enhance this aspect, helping maintain stable postures as well as prevent falls.
- Lifelong Physical Activity: Exercise is essential in building and maintaining strong bones. Aiming for maximum bone mass means starting early with sports like running and jumping as children grow older – building strong bones early helps protect them against age-related bone loss while simultaneously increasing density over time. Exercise should never be delayed. It should always start early! Exercise helps slow age-related bone loss while simultaneously maintaining bone density over time.
Before beginning an exercise regimen for bone issues or risk for fractures, it’s advisable to seek professional guidance first. They will offer guidance as regards which exercises would best meet their requirements in terms of intensity and safety measures for individual needs.
Consistency is key when it comes to exercise and building bone strength. At least three to four times every week, combine weight-bearing exercises with resistance training and balance exercises and gradually increase difficulty and intensity as your fitness increases. Regular physical activity will help your bones remain strong as well as reduce injuries related to bones.
Conclusion
Compact bone and Cancellous bone are the building blocks of our skeletal system, working harmoniously to provide strength, protection, and flexibility. Understanding the roles of these bone tissues and factors affecting bone health empowers us to take better care of our bones throughout our lives.