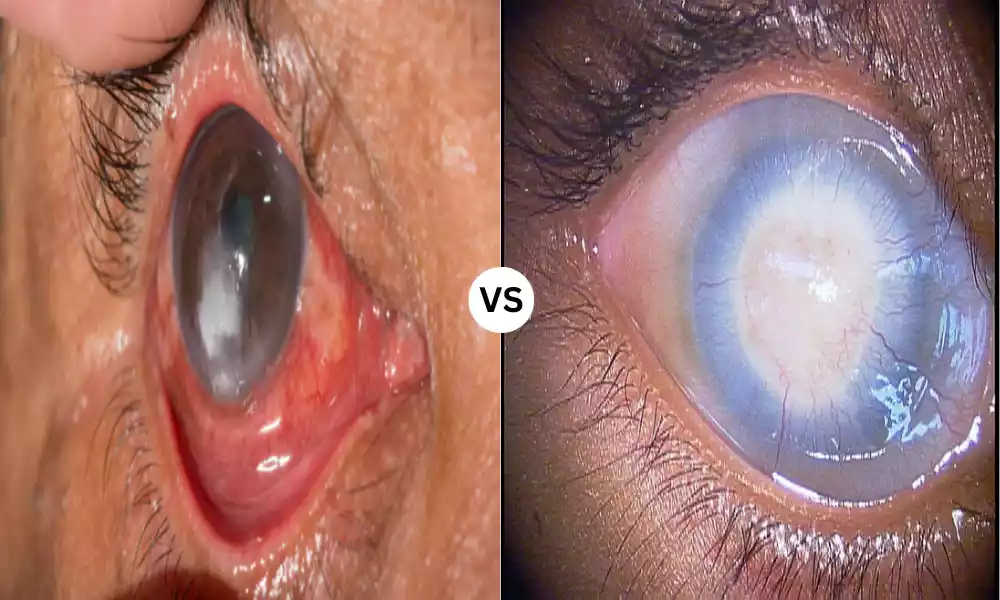
Corneal Ulcer and Corneal Opacity are two significant eye conditions that can affect vision and overall eye health. Corneal ulcers are painful open sores on the cornea, often caused by infections or injuries, while corneal opacity refers to cloudiness or loss of transparency in the cornea. Both conditions can lead to visual impairment if left untreated. We will explore the causes, symptoms, treatments, and preventive measures for corneal ulcers and corneal opacity, providing valuable insights into maintaining optimal corneal health.
Corneal Ulcer
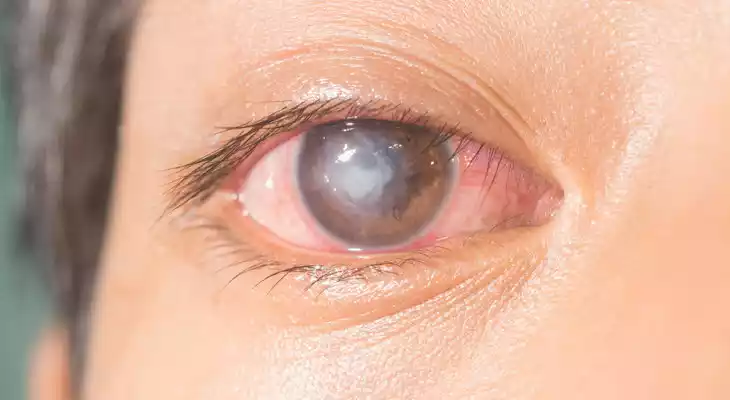
A corneal ulcer is a localized, open sore or lesion that develops on the cornea, which is the clear, dome-shaped outermost layer of the eye’s front surface. These ulcers can vary in size and depth and are typically characterized by the loss of epithelial (outermost) cells on the cornea, exposing the underlying tissue. Corneal ulcers are often painful and can lead to symptoms such as eye redness, tearing, photophobia (sensitivity to light), blurred vision, and a feeling of a foreign object in the eye.
Corneal ulcers can result from various causes, including bacterial, viral, or fungal infections, physical trauma or injury to the eye, or underlying conditions that affect the health of the cornea. They are considered a serious eye condition and require prompt medical attention to prevent complications, such as corneal scarring or vision loss. Treatment typically involves the use of topical medications, such as antibiotics, antifungals, or antivirals, depending on the underlying cause of the ulcer, as well as pain management and close monitoring by an eye specialist. Severe cases may require surgical intervention, such as a corneal transplant.
Causes of Corneal Ulcer
Corneal ulcers can develop as a result of various causes, including infections, injuries, and underlying medical conditions. Here are some common causes of corneal ulcers:
-
- Bacterial Infections: Bacterial infections are a frequent cause of corneal ulcers. Pathogenic bacteria, such as Staphylococcus aureus or Pseudomonas aeruginosa, can invade the cornea through breaks in the epithelial layer. These infections can occur due to contact lens-related issues, eye injuries, or poor hygiene.
- Viral Infections: Viruses, particularly herpes simplex virus (HSV) or varicella-zoster virus (VZV), can lead to viral keratitis, which can cause corneal ulcers. Herpes keratitis is a recurrent condition that may result in painful ulcers on the cornea.
- Fungal Infections: Fungal keratitis is less common but can lead to corneal ulcers, especially in individuals who use contaminated contact lenses or live in regions with high humidity. Fungal infections are often difficult to treat and can be sight-threatening.
- Corneal Abrasions: Trauma to the eye, such as scratches, foreign body penetration, or other forms of injury, can disrupt the corneal epithelium and create an opening for infection, potentially leading to a corneal ulcer.
- Contact Lens Wear: Improper use or care of contact lenses, including extended wear, sleeping with lenses in, or using contaminated solutions, can increase the risk of bacterial or fungal infections, which may result in corneal ulcers.
- Dry Eye Syndrome: Chronic dryness of the eye’s surface can lead to corneal epithelial damage and make the cornea more susceptible to infections that can result in ulcers.
- Underlying Medical Conditions: Certain systemic conditions, such as autoimmune diseases like rheumatoid arthritis or Sjögren’s syndrome, can increase the risk of corneal ulcers due to associated dry eye and compromised corneal health.
- Exposure to Irritants: Chemical or environmental irritants, including harsh chemicals, foreign substances, or environmental pollutants, can damage the cornea and potentially lead to ulcers.
- Use of Steroids: Prolonged use of corticosteroid eye drops without proper medical supervision can weaken the cornea’s immune response, making it more susceptible to infections that may cause ulcers.
- Neurotrophic Cornea: Conditions that affect the corneal nerves, such as diabetes mellitus or herpes zoster infection, can result in decreased corneal sensitivity, making the cornea more prone to injury and ulceration.
Corneal ulcers are a serious eye condition that requires prompt diagnosis and appropriate treatment. Early intervention is crucial to prevent complications, such as corneal scarring or vision loss. If you suspect you have a corneal ulcer or experience symptoms like eye pain, redness, photophobia, or blurred vision, it is essential to seek immediate medical attention from an eye care specialist.
Symptoms of Corneal Ulcer
Corneal ulcers are characterized by a range of symptoms that can vary in severity depending on the cause and stage of the ulcer. Common symptoms of a corneal ulcer include:
-
- Eye Pain: Corneal ulcers are typically associated with moderate to severe eye pain, which may feel like a sharp, stabbing sensation. The pain can be constant or intermittent.
- Redness: The affected eye often appears red or bloodshot due to the inflammation and irritation caused by the ulcer.
- Tearing: Excessive tearing, or epiphora, is a common response to the irritation of the corneal ulcer. The tearing may be accompanied by a watery discharge.
- Photophobia: People with corneal ulcers are often sensitive to light, a condition known as photophobia. Bright lights can exacerbate discomfort and pain.
- Blurred Vision: The presence of an ulcer on the cornea can cause visual disturbances, leading to blurred or hazy vision.
- Foreign Body Sensation: Some individuals with corneal ulcers report a feeling of having a foreign object, such as sand or grit, in their eye. This sensation can be quite uncomfortable.
- Decreased Vision: As the ulcer progresses and affects the corneal tissue, it can lead to a noticeable decrease in vision. The extent of vision loss depends on the size and location of the ulcer.
- Eye Discharge: Depending on the underlying cause of the corneal ulcer, there may be discharge from the affected eye. The discharge may be clear or purulent (containing pus) in cases of infection.
- Excessive Blinking and Squinting: To protect the eye from further irritation and discomfort, individuals with corneal ulcers may frequently blink or squint.
The severity of these symptoms can vary, and some individuals may experience only a subset of these symptoms. Additionally, the progression of symptoms may differ depending on the underlying cause of the corneal ulcer.
Corneal ulcers are a serious eye condition that requires prompt medical attention from an eye care specialist or ophthalmologist. Delayed treatment can lead to complications, including corneal scarring, vision loss, or even perforation of the cornea. If you experience any of the above symptoms or suspect you have a corneal ulcer, seek immediate evaluation and treatment to protect your eye health and preserve your vision.
Corneal Opacity
Corneal opacity refers to an abnormal condition of the cornea, which is the clear, transparent front surface of the eye. In corneal opacity, the cornea becomes cloudy, hazy, or partially opaque, which impairs its normal transparency. This loss of clarity can disrupt the passage of light through the cornea and affect vision.

Corneal opacity can result from various causes, including scarring, inflammation, injury, or underlying medical conditions. The degree of opacity can vary, ranging from mild haziness that only slightly affects vision to complete cloudiness that significantly impairs vision. The appearance and severity of corneal opacity depend on the underlying cause and the extent of damage to the corneal tissue.
Treatment of corneal opacity depends on its cause and severity. It may involve managing underlying conditions, using corrective lenses (such as glasses or contact lenses) to improve vision, or, in more severe cases, surgical intervention such as a corneal transplant to replace the damaged corneal tissue with healthy donor tissue.
Causes of Corneal Opacity
Corneal opacity can result from various underlying causes that affect the clarity of the cornea, leading to a loss of transparency. These causes can vary in nature and include:
-
- Corneal Scarring: Scar tissue formation on the cornea is one of the most common causes of corneal opacity. Scarring can occur due to various factors, such as previous corneal injuries, infections (including corneal ulcers), or surgical procedures.
- Inflammatory Conditions: Chronic inflammation of the cornea, known as keratitis, can lead to corneal opacity. Inflammatory conditions may result from autoimmune disorders, infections, or other underlying issues.
- Corneal Dystrophies: Genetic or hereditary disorders like Fuchs’ dystrophy or lattice dystrophy can cause abnormal deposits or changes in the corneal tissue, leading to opacity.
- Keratoconus: This progressive eye condition causes the cornea to become thin and bulge forward in a cone shape. Over time, the distorted shape can lead to corneal opacity.
- Infections: Severe and untreated corneal infections, such as fungal keratitis, can result in scarring and opacity.
- Chemical or Thermal Burns: Exposure to caustic chemicals or extreme heat can damage the cornea and cause opacity.
- Trauma: Direct injury to the eye, including corneal abrasions, foreign body penetration, or blunt trauma, can disrupt the cornea and lead to scarring and opacity.
- Metabolic Disorders: Certain metabolic conditions, such as hereditary tyrosinemia or mucopolysaccharidoses, can affect the cornea and lead to opacity.
- Neurotrophic Cornea: Conditions that affect the corneal nerves, like diabetes mellitus or herpes zoster infection (shingles), can lead to decreased corneal sensitivity and potential injury, which may result in corneal opacity.
- Contact Lens-Related Issues: Prolonged and improper use of contact lenses, including extended wear or using lenses that do not fit properly, can lead to corneal damage and opacity.
- Age-Related Changes: As people age, changes in the cornea’s structure and function can lead to reduced transparency and mild opacity.
The treatment of corneal opacity depends on the underlying cause and the extent of the opacity. It may involve managing the underlying condition, using corrective lenses (such as glasses or contact lenses) to improve vision, or surgical intervention, such as a corneal transplant, to replace the damaged corneal tissue with healthy donor tissue. The specific treatment plan is determined by an eye care specialist after a thorough evaluation.
Symptoms of Corneal Opacity
Corneal opacity itself is not a standalone condition but rather a result of an underlying issue that affects the transparency of the cornea. Therefore, the symptoms of corneal opacity are often associated with the underlying cause and the extent of the opacity. Common symptoms that individuals with corneal opacity may experience include:
-
- Blurred Vision: Corneal opacity can lead to blurred or hazy vision, making it difficult to see clearly. The degree of vision impairment can vary depending on the extent of opacity.
- Reduced Visual Acuity: Individuals may experience a decrease in visual sharpness, resulting in difficulty reading, recognizing faces, or performing tasks that require clear vision.
- Glare or Halos: Some people with corneal opacity may perceive glare or halos around lights, especially when driving at night or in bright lighting conditions.
- Distorted Vision: The presence of opacity in the cornea can cause light to scatter irregularly, leading to distorted or wavy vision.
- Photophobia: Sensitivity to light (photophobia) may develop, making it uncomfortable to be in brightly lit environments.
- Eye Irritation: Depending on the underlying cause, individuals with corneal opacity may experience eye discomfort, itching, or a foreign body sensation.
- Excessive Tearing: Irritation caused by corneal opacity can trigger excessive tearing or watery eyes.
- Pain or Discomfort: In some cases, especially if the opacity is associated with inflammation or injury, individuals may experience mild to moderate eye pain or discomfort.
The specific symptoms can vary based on the underlying condition causing the corneal opacity. For instance, corneal opacity resulting from corneal scarring may have different symptoms than opacity due to an inflammatory condition.
If you experience any of these symptoms or suspect you have corneal opacity, it is crucial to seek evaluation and treatment by an eye care specialist, such as an ophthalmologist. Identifying and addressing the underlying cause is essential for managing corneal opacity and improving visual function. Treatment options will depend on the underlying condition and may include medications, corrective lenses, or surgical intervention like a corneal transplant.
Comparison Table of Corneal Ulcer and Corneal Opacity
Here is a comparison table highlighting the key differences between corneal ulcers and corneal opacity:
| Characteristic | Corneal Ulcer | Corneal Opacity |
|---|---|---|
| Definition | Open sore or lesion on the cornea resulting from infection, injury, or underlying conditions leading to tissue loss. | Loss of transparency or clarity in the cornea due to various causes, often from scarring or inflammation. |
| Symptoms | – Eye pain
– Redness – Tearing – Photophobia (light sensitivity) – Blurred vision – Sensation of foreign body in the eye – Discharge (if due to infection) |
– Blurred vision
– Reduced visual acuity – Glare or halos – Distorted vision – Photophobia – Eye irritation – Excessive tearing – Possible pain or discomfort |
| Causes | – Bacterial, viral, fungal infections
– Trauma or injury – Contact lens-related issues – Underlying medical conditions – Use of steroids |
– Scarring (from previous injury, infections, or surgery)
– Inflammatory conditions – Corneal dystrophies – Keratoconus – Infections (leading to scarring or inflammation) |
| Diagnosis | – Clinical examination by an eye specialist
– Corneal staining (to visualize the ulcer) |
– Clinical examination by an eye specialist
– Corneal imaging (pachymetry, topography) |
| Treatment | – Antibiotics, antifungals, or antivirals (based on cause)
– Steroids (for inflammation) – Pain management – In severe cases, corneal transplant |
– Management of underlying cause (if applicable)
– Corrective lenses (glasses or contact lenses) – Surgical intervention (e.g., corneal transplant) |
| Prognosis | Varies depending on the cause, severity, and promptness of treatment. Severe ulcers can lead to scarring, vision loss, or corneal perforation. | Depends on the cause and extent of the opacity; some cases maybe managed with good vision, while others may requiresurgical intervention. |
While corneal ulcers and corneal opacity are distinct conditions, they can sometimes be related. For example, a corneal ulcer that has healed may leave behind scarring, which can contribute to corneal opacity. Additionally, both conditions warrant prompt attention from an eye care specialist to prevent complications and preserve vision.
How to diagnosis of Corneal Ulcer and Corneal Opacity
The diagnosis of corneal ulcers and corneal opacity involves a thorough eye examination performed by an eye care specialist, typically an ophthalmologist. Specialized tests and imaging may also be used to assess the condition and determine the underlying cause.

Here is an overview of the diagnostic process for both conditions:
Diagnosis of Corneal Ulcer:
- Patient History: The ophthalmologist will start by taking a detailed patient history, including information about symptoms, the duration of symptoms, any recent eye injuries or infections, contact lens use, and relevant medical history.
- Visual Acuity Test: A visual acuity test is performed to measure the patient’s visual sharpness and determine if the ulcer has affected vision.
- Slit-Lamp Examination: The ophthalmologist uses a slit-lamp microscope to examine the cornea closely. This instrument provides a magnified view of the cornea, allowing the doctor to assess the size, depth, and location of the ulcer.
- Fluorescein Staining: Fluorescein dye is applied to the eye’s surface, and a blue light is used to illuminate the eye. The dye highlights the area of the corneal ulcer, making it more visible for examination.
- Measurement of Corneal Thickness: Pachymetry is a test that measures the thickness of the cornea. It can help determine if the ulcer has caused corneal thinning, which is a concern for potential perforation.
- Cultures and Scraping: If an infectious corneal ulcer is suspected, a sample of the ulcer may be collected for laboratory analysis to identify the specific causative organism (bacteria, virus, or fungus).
- Corneal Imaging: In some cases, imaging techniques like anterior segment optical coherence tomography (AS-OCT) or confocal microscopy may be used to obtain more detailed images of the cornea and the extent of the ulcer.
Diagnosis of Corneal Opacity:
- Patient History: Similar to corneal ulcers, the ophthalmologist will begin by taking a detailed patient history, including information about symptoms, any prior eye injuries or surgeries, and any underlying medical conditions.
- Visual Acuity Test: A visual acuity test is performed to measure the patient’s visual sharpness and determine the extent of vision impairment caused by corneal opacity.
- Slit-Lamp Examination: A slit-lamp examination is used to evaluate the cornea’s appearance and the degree of opacity. The doctor can assess the location, size, and characteristics of the opacity.
- Corneal Imaging: Advanced imaging techniques, such as corneal topography or pachymetry, may be used to assess the extent of corneal opacity and determine if corneal thickness is affected.
- Underlying Condition Evaluation: If the cause of corneal opacity is unclear, further testing or evaluation of underlying medical conditions may be necessary. This can include blood tests or additional imaging studies.
The specific diagnostic approach may vary based on the patient’s symptoms, medical history, and the ophthalmologist’s clinical judgment. Once the diagnosis is established, the underlying cause of the corneal ulcer or corneal opacity can be determined, and an appropriate treatment plan can be developed to address the condition effectively. Early diagnosis is essential to prevent complications and preserve vision in both cases.
Treatment approaches for Corneal Ulcer and Corneal Opacity
Treatment approaches for corneal ulcers and corneal opacity differ based on the underlying condition and the extent of damage to the cornea. Here are the typical treatment approaches for each condition:
Treatment for Corneal Ulcer:
- Identification of Underlying Cause: The first step is to determine the cause of the corneal ulcer, whether it’s bacterial, viral, fungal, or due to injury.
- Topical Medications:
- Antibiotics: Bacterial ulcers are often treated with broad-spectrum antibiotic eye drops or ointments.
- Antifungals: Fungal ulcers require antifungal medications.
- Antivirals: Viral ulcers caused by herpes simplex or varicella-zoster virus may be treated with antiviral medications.
- Pain Management: To alleviate eye pain associated with corneal ulcers, pain-relieving eye drops or oral pain medications may be prescribed.
- Corticosteroids: In some cases, especially if there is significant inflammation, corticosteroid eye drops may be used. However, these are typically avoided if there is an active infection.
- Frequent Monitoring: Close follow-up with an eye care specialist is essential to assess the ulcer’s progress and response to treatment.
- Protection and Hygiene: It’s important to protect the affected eye from further injury and maintain good eye hygiene during treatment.
- Surgery (in severe cases): If the ulcer is unresponsive to medical treatment, or if it has caused extensive corneal damage, a corneal transplant (keratoplasty) may be necessary to replace the damaged corneal tissue with healthy donor tissue.
Treatment for Corneal Opacity:
The treatment of corneal opacity primarily depends on its underlying cause and the extent of vision impairment:
- Management of Underlying Condition: If corneal opacity is secondary to an underlying medical condition or inflammation, treating the underlying condition is the first priority. This may involve medications, lifestyle changes, or other medical interventions.
- Corrective Lenses: In mild cases where vision is only slightly impaired, the use of glasses or contact lenses may be sufficient to improve visual acuity and clarity.
- Surgical Intervention (e.g., Corneal Transplant): In cases of severe or extensive corneal opacity that significantly impairs vision and does not respond to other treatments, a corneal transplant (keratoplasty) may be recommended. During a transplant, the damaged corneal tissue is replaced with healthy donor tissue to restore transparency.
- Rehabilitative Services: Vision rehabilitation services, including low vision aids and training, may be recommended to help individuals maximize their remaining vision and adapt to visual impairment if vision cannot be fully restored.
- Management of Symptoms: Depending on the specific symptoms associated with corneal opacity (e.g., photophobia or glare), additional measures such as sunglasses or anti-glare coatings on glasses may be helpful.
The choice of treatment for both corneal ulcers and corneal opacity is determined by an eye care specialist (ophthalmologist) after a thorough evaluation. Early intervention and proper management are crucial to prevent complications and preserve vision in individuals with these conditions.
Prevention of Corneal Ulcer and Corneal Opacity
Preventing corneal ulcers and corneal opacity involves taking measures to protect the health and integrity of the cornea, as well as addressing underlying risk factors and conditions that can lead to these eye conditions. Here are some prevention strategies for corneal ulcers and corneal opacity:
Prevention of Corneal Ulcer:
- Proper Contact Lens Care:
- Follow strict hygiene practices when handling contact lenses.
- Wash hands thoroughly before touching lenses.
- Clean and disinfect lenses as recommended by an eye care specialist.
- Avoid sleeping in contact lenses unless prescribed by an eye doctor.
- Replace contact lenses as directed, and never wear expired lenses.
- Avoid Eye Trauma:
- Protect your eyes from injury during sports and activities by wearing appropriate protective gear, such as goggles or safety glasses.
- Be cautious when handling sharp objects or chemicals that could potentially harm the eyes.
- Good Eye Hygiene:
- Avoid rubbing your eyes with dirty hands.
- Do not share eye makeup, contact lenses, or eye drops with others.
- Keep your face and eyes clean.
- Regular Eye Examinations:
- Schedule regular eye check-ups with an eye care specialist to monitor the health of your eyes and address any potential issues promptly.
- Proper Use of Eye Medications:
- Use prescribed eye medications, such as steroids or antibiotics, strictly as directed by your eye doctor.
- Do not use medications meant for one eye in the other eye.
- Hydration and Lubrication: Keep the eyes adequately lubricated with artificial tears or lubricating eye drops if you have dry eyes or other conditions that increase the risk of corneal dryness and irritation.
Prevention of Corneal Opacity:
- Manage Underlying Medical Conditions: If you have an underlying medical condition, such as autoimmune disorders or metabolic diseases, work closely with your healthcare provider to manage the condition effectively.
- Eye Protection: Use eye protection when engaging in activities that pose a risk of eye injury, such as wearing safety goggles when working with tools or participating in sports with potential eye hazards.
- Avoid Eye Irritants: Be cautious around chemicals, smoke, and other irritants that could harm the eyes. Use protective eyewear when necessary.
- Proper Contact Lens Use: Follow the same guidelines for proper contact lens use and hygiene as outlined in the prevention of corneal ulcers.
- Early Treatment: If you experience any symptoms of eye discomfort, pain, redness, or vision changes, seek immediate medical attention. Early diagnosis and treatment can help prevent complications that may lead to corneal opacity.
- Regular Eye Examinations: Regular eye check-ups with an eye care specialist can help identify and address any eye conditions or risk factors for corneal opacity.
It’s essential to maintain good eye hygiene and take precautions to protect your eyes from injury and infection. Regular eye exams are crucial for early detection and timely intervention, which can be instrumental in preventing the development of corneal ulcers and corneal opacity.
What are similarities between Corneal Ulcer and Corneal Opacity?
Corneal ulcers and corneal opacity are both eye conditions that involve the cornea, the clear, front surface of the eye. While they are distinct conditions with different causes and characteristics, there are some similarities between them:
- Corneal Involvement: Both corneal ulcers and corneal opacity primarily affect the cornea, which is responsible for the eye’s clarity and focusing of light onto the retina.
- Vision Impairment: Both conditions can lead to vision impairment. Corneal ulcers can cause blurred vision, and corneal opacity, by definition, results in a loss of corneal transparency, leading to decreased visual clarity.
- Symptoms: While the specific symptoms may differ, both conditions can result in eye redness, discomfort, and sensitivity to light (photophobia).
- Diagnosis: Both conditions are typically diagnosed through clinical examination by an eye care specialist, which may include the use of specialized tests and imaging to assess the extent of the condition.
- Treatment by an Eye Specialist: Both corneal ulcers and corneal opacity require evaluation and treatment by an ophthalmologist or eye care specialist with expertise in managing corneal conditions.
- Potential Complications: If left untreated or not managed appropriately, both conditions can lead to complications that may affect vision. Corneal ulcers can result in corneal scarring, and corneal opacity can cause significant vision loss.
- Importance of Early Intervention: Early diagnosis and prompt treatment are crucial for both conditions to prevent complications and preserve vision.
- Need for Preventive Measures: Preventive measures, such as proper contact lens care, eye protection, and good eye hygiene, can help reduce the risk of both corneal ulcers and corneal opacity.
While these similarities exist, it’s important to note that the underlying causes, treatments, and long-term outcomes for corneal ulcers and corneal opacity can vary significantly. Therefore, a proper diagnosis and tailored treatment plan are essential for each condition.
Conclusion
Corneal Ulcers and Corneal Opacity are significant eye conditions that can impact vision and eye health. Corneal ulcers involve open sores on the cornea, often caused by infections or injuries, and require prompt diagnosis and treatment to prevent complications. On the other hand, corneal opacity refers to the loss of corneal transparency due to various factors, including scarring and inflammation, and may result in blurred vision.
Early intervention, tailored to the underlying cause, is essential in both cases to safeguard vision and minimize potential long-term consequences. Regular eye care and preventive measures play a crucial role in maintaining the health of the cornea and overall eye well-being.