Dermatomyositis and Polymyositis are both rare, systemic autoimmune conditions characterized primarily by inflammation of the muscles, leading to muscle weakness and other related symptoms. Dermatomyositis is distinct in its presentation with unique skin manifestations, such as the heliotrope rash and Gottron’s papules, whereas Polymyositis affects only the muscles without the skin involvement. Though they share similarities in terms of muscle symptoms, their etiology, associated conditions, and treatment can differ. Accurate diagnosis and differentiation are vital as they guide treatment decisions and patient prognosis.
What is Dermatomyositis?
Dermatomyositis (DM) is a rare autoimmune disease characterized by inflammation of the muscles and distinctive skin rashes. The inflammation leads to muscle weakness, typically in the muscles closest to the trunk, such as those in the hips, thighs, shoulders, and neck. The exact cause of DM is unknown, but it involves an immune response that mistakenly targets the body’s own tissues, particularly small blood vessels within muscles and skin. In addition to muscle symptoms, unique skin manifestations set DM apart from other inflammatory myopathies.

These can include a heliotrope rash (a purplish rash on the upper eyelids), Gottron’s papules (raised, reddish patches over the knuckles), and other rashes. Dermatomyositis can affect people of all ages but is more common in adults in their 50s and 60s and children between 5 and 15 years old. The condition can also be associated with other systemic features, and in some adults, there’s an increased risk of malignancy. Treatment typically involves medications to control inflammation and manage symptoms.
Causes of Dermatomyositis
The exact cause of dermatomyositis (DM) remains unclear, but it is believed to be an autoimmune disorder where the body’s immune system mistakenly attacks its own tissues. Several factors have been proposed to contribute to the development and progression of DM:
-
- Autoimmune Reaction: DM is characterized by an immune response against the body’s own tissues. The immune system, which normally defends the body against infections, turns against the body’s muscles and skin in patients with DM.
- Viral Infections: Some researchers believe that viral infections might trigger the disease in genetically predisposed individuals. However, no specific virus has been definitively linked to DM.
- Genetic Predisposition: There is some evidence to suggest that certain genetic factors can increase one’s susceptibility to DM.
- Drug Reactions: In rare instances, DM has been linked to the use of certain medications, leading to a condition known as “drug-induced DM.” Once the medication is discontinued, symptoms may improve or resolve.
- Cancer: DM is associated with an increased risk of malignancy in adults. Some believe that the body’s immune response against a tumor might cross-react with tissues in the skin and muscles, leading to DM. This is termed paraneoplastic DM.
- Environmental Triggers: Exposure to certain environmental factors, like ultraviolet (UV) radiation, has been proposed as a potential trigger for DM in some individuals.
- Other Connective Tissue Diseases: DM can sometimes occur alongside other autoimmune diseases like systemic lupus erythematosus or rheumatoid arthritis.
While these factors might contribute to the disease, the exact cause of DM remains a topic of ongoing research. Often, a combination of genetic, environmental, and other factors may be involved in its onset and progression.
Symptoms of Dermatomyositis
Dermatomyositis (DM) presents with a combination of muscle and skin symptoms. Here are the primary manifestations associated with this condition:
Muscle Symptoms:
- Muscle Weakness: Proximal muscles (those closest to the trunk, like in the shoulders, neck, hips, and thighs) are commonly affected, making it difficult for patients to climb stairs, lift objects, or rise from a sitting position.
- Muscle Pain and Tenderness: Some people may experience muscle discomfort or pain.
Skin Symptoms:
- Heliotrope Rash: A purplish or red rash on the upper eyelids, often accompanied by swelling.
- Gottron’s Papules: Raised, reddish or violet patches over the knuckles and sometimes on the elbows and knees.
- Shawl Sign: A red or reddish-purple rash on the neck, shoulders, upper chest, and back.
- V-Neck Sign: Similar rash as the shawl sign but located on the front of the chest in the V-neck area.
- Holster Sign: A rash on the sides of the hips or outer thighs.
- Periungual Erythema: Redness around the nails.
- Mechanic’s Hands: Rough and cracked skin on the tips and sides of the fingers, making them appear as if they are dirty.
Other Symptoms and Complications:
- Calcinosis: Calcium deposits under the skin or in the muscles, particularly in children.
- Raynaud’s Phenomenon: Fingers or toes turn white or blue in response to cold temperatures or stress.
- Dysphagia: Difficulty swallowing due to muscle weakness affecting the throat.
- Lung Involvement: Such as interstitial lung disease, leading to coughing, shortness of breath, and other respiratory symptoms.
- Joint Pain: Arthralgia or arthritis can also occur in some patients.
- Cardiac Involvement: Arrhythmias, congestive heart failure, or inflammation of the heart muscle (myocarditis) can occur in severe cases.
It’s important to understand that the presence and severity of these symptoms can vary widely among patients. Some may primarily have skin symptoms with minimal muscle involvement, while others might experience significant muscle weakness without prominent skin findings. Early diagnosis and treatment are crucial to manage the symptoms and prevent complications effectively. If someone suspects they have dermatomyositis, they should seek medical attention promptly.
What is Polymyositis?
Polymyositis (PM) is an inflammatory autoimmune disease that results in muscle weakness, predominantly affecting the proximal muscles, such as those in the thighs, hips, shoulders, and neck. The condition is marked by the inflammation and subsequent damage of muscle fibers. This leads to symptoms such as muscle pain, tenderness, fatigue, and weakness.

The exact cause of polymyositis remains elusive, but it involves an aberrant immune response in which the body’s immune system mistakenly attacks healthy muscle tissue. Unlike dermatomyositis, which is a related condition, polymyositis does not manifest with skin rashes. Polymyositis can affect people of various ages but typically appears in adults between the ages of 30 and 50.
Early diagnosis and treatment are essential, as the disease, if left untreated, can lead to significant muscle weakness and functional disability. Management typically involves medications that suppress the immune system and reduce inflammation.
Causes of Polymyositis
Polymyositis (PM) is an autoimmune disorder, but its exact cause remains unclear. In individuals with polymyositis, the immune system—which is supposed to protect the body from infections and diseases—mistakenly attacks healthy muscle tissue, leading to inflammation and muscle damage.
Several factors are believed to contribute to the onset and progression of PM:
-
- Autoimmune Mechanism: Polymyositis is considered to be an autoimmune disease where the body’s own immune cells target and damage muscle fibers.
- Viral Infections: There’s some speculation that viral infections might initiate the disease in genetically predisposed individuals. However, a specific virus as a direct cause of PM has not been conclusively identified.
- Genetic Predisposition: Certain genetic factors or patterns may make some individuals more susceptible to developing PM.
- Environmental Triggers: Just as with dermatomyositis, exposure to certain environmental factors has been proposed as a potential trigger for PM in some individuals. However, the evidence is not robust, and more research is needed.
- Drug Reactions: There are a few reports of drug-induced polymyositis, although this is less common than drug-induced dermatomyositis. Discontinuing the causative drug often leads to symptom improvement.
- Association with Other Autoimmune Disorders: PM can sometimes coexist with other autoimmune diseases, suggesting shared or overlapping pathogenic mechanisms.
Despite these factors, the precise cause of PM remains elusive. It’s likely that a combination of genetic, environmental, and other unknown factors play a role in its development. As research continues, more clarity about the exact causes or triggers for polymyositis may emerge.
Symptoms of Polymyositis
Polymyositis (PM) primarily affects the muscles, leading to a range of muscle-related symptoms. Here are the most common manifestations associated with this condition:
- Muscle Weakness: This is the hallmark symptom of polymyositis. The weakness typically affects the proximal muscles, which are the muscles closest to the trunk of the body, such as those in the hips, thighs, shoulders, and neck. As a result, individuals with PM may have difficulty climbing stairs, lifting objects, standing up from a seated position, or reaching overhead.
- Muscle Pain and Tenderness: While muscle weakness is more common, some people with PM may also experience muscle pain (myalgia) or tenderness, although this is less frequent than in other inflammatory myopathies.
- Difficulty Swallowing (Dysphagia): In some individuals with PM, the muscles involved in swallowing can become weakened, leading to difficulty swallowing or choking.
- Respiratory Problems: If the muscles that support breathing become affected, individuals might experience shortness of breath or respiratory failure in severe cases.
- Fatigue: Many individuals with PM report feeling unusually tired or fatigued.
- Joint Pain: Arthralgia or arthritis can occur in some patients with PM, leading to joint pain or swelling.
- General Malaise: A feeling of overall discomfort or uneasiness can sometimes accompany PM.
- Raynaud’s Phenomenon: In some cases, individuals with PM might also experience Raynaud’s phenomenon, where the fingers or toes turn white or blue in response to cold temperatures or stress.
- Cardiac Symptoms: Although less common, PM can also affect the heart, leading to irregular heart rhythms or other cardiac issues.
It’s important to understand that the presentation and severity of symptoms can vary among individuals with polymyositis. The condition can be progressive, with muscle weakness increasing over time. Early diagnosis and intervention are crucial to manage the disease effectively and to prevent complications. If someone suspects they have polymyositis, they should consult a healthcare professional.
Comparison Table of Dermatomyositis and Polymyositis
The Comparison Table of Dermatomyositis and Polymyositis:
| Feature/Aspect | Dermatomyositis (DM) | Polymyositis (PM) |
|---|---|---|
| Basic Definition | Autoimmune disease with muscle inflammation and distinctive skin rashes. | Autoimmune disease causing muscle inflammation without skin involvement. |
| Primary Affected Area | Muscles and skin | Muscles only |
| Typical Onset Age | Adults in 50s-60s; Children 5-15 years old | Adults between 30-50 years old |
| Skin Symptoms | Heliotrope rash, Gottron’s papules, shawl and V-neck signs, among others. | No specific skin symptoms |
| Muscle Symptoms | Proximal muscle weakness, often symmetric | Proximal muscle weakness, often symmetric |
| Associated Conditions | Increased risk of malignancy in some adults, interstitial lung disease, other connective tissue diseases. | Less common association with malignancies, may have overlap with other autoimmune conditions. |
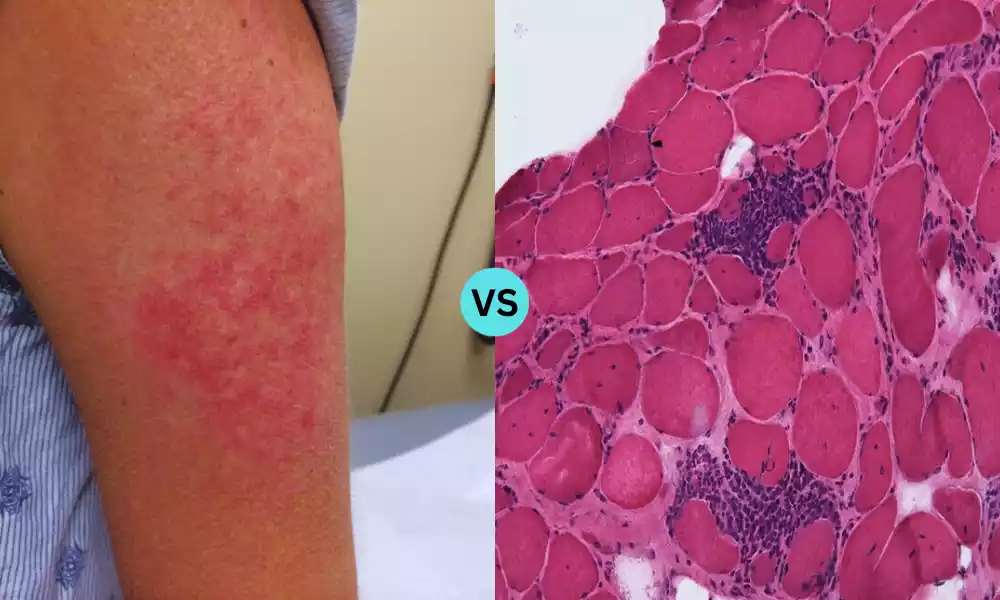
| Muscle Biopsy Findings | Perifascicular atrophy and inflammation | Endomysial inflammation with muscle fiber invasion |
| Common Treatments | Corticosteroids, immunosuppressive agents, IVIG, physical therapy | Corticosteroids, immunosuppressive agents, physical and occupational therapy |
| Immune Response | Targets small blood vessels in muscles and skin | Directly targets muscle fibers |
This table provides a general overview, but it’s important to understand that individual presentations might vary, and the diseases can sometimes overlap. Always consult a medical expert for precise diagnosis and treatment.
What are the similarities between Dermatomyositis and Polymyositis?
Dermatomyositis (DM) and polymyositis (PM) are both classified as inflammatory myopathies, and they share several similarities in terms of their clinical presentation, pathology, and potential etiologies. Here are the primary similarities between the two:
-
- Muscle Weakness: Both conditions predominantly cause symmetric, proximal muscle weakness (affecting muscles close to the trunk, like those of the shoulders and hips).
- Autoimmune Nature: DM and PM are believed to be autoimmune disorders where the body’s immune system mistakenly attacks healthy tissue, particularly muscle fibers.
- Elevated Muscle Enzymes: Blood tests in patients with either condition often show elevated levels of muscle enzymes, indicating muscle inflammation or damage. Commonly tested enzymes include creatine kinase (CK), aldolase, lactate dehydrogenase (LDH), and aspartate aminotransferase (AST).
- EMG Findings: Electromyography (EMG), a test used to assess the health of muscles and the nerve cells that control them, often shows characteristic patterns of muscle irritation and damage in both conditions.
- Histological Features: Muscle biopsy, a diagnostic tool where a small sample of muscle tissue is removed and examined under a microscope, often reveals inflammatory changes in both DM and PM.
- Treatment Approach: The initial treatment strategies for both conditions are quite similar, typically involving corticosteroids like prednisone. Immunosuppressive medications may also be used in both to control the disease and reduce corticosteroid doses.
- Association with Other Diseases: Both DM and PM can be associated with other systemic autoimmune diseases, and both can occasionally be paraneoplastic, meaning they might be associated with an underlying malignancy.
- Potential Causes: While the exact causes of both conditions are not fully understood, they are believed to involve a mix of genetic predisposition, environmental triggers, and possibly viral infections.
- Complications: Both DM and PM can lead to complications beyond muscle weakness, including respiratory issues, cardiac problems, and difficulty swallowing, among others.
While these similarities exist, it’s essential to recognize that DM and PM are distinct conditions with unique clinical features, especially the characteristic skin manifestations of DM. Proper diagnosis and differentiation between the two are crucial for effective management and treatment.
Treatment and Management of Dermatomyositis and Polymyositis
The treatment and management of dermatomyositis (DM) and polymyositis (PM) are somewhat similar because both are inflammatory myopathies. The primary goal of treatment is to reduce inflammation, improve muscle strength and function, and manage any associated complications or other systemic features.
Here’s an overview of the treatment and management strategies for both conditions:
- Corticosteroids:
- Prednisone is usually the first-line treatment for DM and PM. It’s an anti-inflammatory medication that can help reduce muscle inflammation and improve muscle strength.
- Long-term use of corticosteroids can have side effects, so doctors aim to taper the dosage once the patient starts to improve, and may introduce other medications to help reduce the required steroid dose.
- Immunosuppressive Agents:
- These are used either in combination with corticosteroids or when patients don’t respond well to steroids.
- Commonly used agents include methotrexate, azathioprine (Imuran), mycophenolate mofetil, and cyclosporine. They work by suppressing the immune system’s abnormal response.
- Immunoglobulin Therapy:
- Intravenous immunoglobulin (IVIG) is a treatment where purified human antibodies are given through a vein. It can be effective for those who don’t respond to other treatments.
- Biologic Therapies:
- Drugs like rituximab (which targets specific immune cells) have been used in refractory cases or severe disease manifestations.
- Antimalarial Medications:
- Drugs like hydroxychloroquine are sometimes used, particularly for skin symptoms in DM.
- Physical and Occupational Therapy:
- Essential for maintaining muscle strength and preventing muscle atrophy.
- Therapists can provide exercises and strategies to improve mobility, muscle strength, and daily functioning.
- Sun Protection:
- For those with DM, sun protection is essential since sunlight can exacerbate skin symptoms. This includes using sunscreens, wearing protective clothing, and avoiding peak sunlight hours.
- Regular Monitoring:
- Both conditions may have associated complications, including heart, lung, and joint involvement, so regular medical evaluations are crucial.
- Periodic muscle strength testing, lung function tests, and blood tests can help monitor disease activity and the effectiveness of treatments.
- Management of Associated Conditions:
- For those with associated conditions (like interstitial lung disease or malignancies with DM), additional treatments or interventions may be necessary.
- Lifestyle Measures:
- Eating a balanced diet, getting regular exercise (as recommended by a healthcare professional), and avoiding triggers (like sun exposure for DM) can be beneficial.
The choice of treatments often depends on the severity of symptoms, the patient’s overall health, and the presence of any associated conditions or complications. It’s essential for patients to work closely with their rheumatologists or other specialists to develop an individualized treatment plan.
How to Prevention of Dermatomyositis and Polymyositis
The exact causes of dermatomyositis (DM) and polymyositis (PM) are not entirely understood, but they are believed to result from a combination of genetic, environmental, and possibly infectious factors leading to an autoimmune response. Due to the multifactorial nature of their onset, specific prevention strategies for DM and PM have not been established.
There are general measures that can be considered:
- Awareness: Be aware of the symptoms, especially if there’s a family history of autoimmune diseases. Early detection and intervention can lead to better outcomes.
- Avoid Potential Triggers: While not proven, some individuals report the onset of symptoms after certain events like infections, medication use, or exposure to environmental toxins. It’s wise to be cautious and aware, although it’s not always possible to avoid such triggers.
- Sun Protection (especially for DM): For those with dermatomyositis or a predisposition to it, sun protection is crucial. Using sunscreens, wearing protective clothing, and avoiding excessive sun exposure can help prevent skin symptoms from worsening or flaring.
- Regular Health Check-ups: Maintaining routine health examinations can help detect early signs of autoimmune disorders and initiate timely interventions.
- Healthy Lifestyle: Maintaining a healthy lifestyle with a balanced diet, regular exercise, and stress reduction techniques can potentially help in boosting overall immunity and reducing the risk of various diseases.
- Vaccinations: Keeping up-to-date with vaccinations might help prevent infections that could potentially trigger or exacerbate autoimmune responses.
- Avoid Smoking: Smoking is known to have various negative impacts on health and might be involved in the exacerbation of some autoimmune conditions.
- Medication Review: If on medication, especially new ones, monitor for any new or unusual symptoms and report them to a healthcare provider. There have been instances where drug reactions have induced symptoms similar to DM or PM.
- Stay Informed: As research continues, new information regarding the prevention and management of DM and PM may emerge. It’s beneficial for at-risk individuals to stay informed.
It’s essential to understand that while these measures can support overall health and might reduce the risk of various conditions, there’s no definitive way to prevent DM or PM due to the complexity of their causes. If someone suspects they have or are developing symptoms of these conditions, they should seek medical attention promptly.
Conclusion
Dermatomyositis (DM) and polymyositis (PM) are complex autoimmune inflammatory myopathies characterized by muscle weakness and inflammation. While they share several clinical and pathological features, DM is distinguished by its unique skin manifestations. The exact causes remain elusive, stemming from a combination of genetic, environmental, and possibly infectious factors.
Treatment primarily aims to reduce inflammation and improve muscle function, employing corticosteroids, immunosuppressive agents, and other modalities. Continued research seeks to better understand these conditions, aiming for improved treatments and potential prevention strategies. Early diagnosis and intervention are crucial for managing these conditions effectively and ensuring the best possible patient outcomes.