Atopic and Seborrheic Dermatitis are two distinct but common skin conditions that can cause discomfort and affect one’s quality of life. Atopic dermatitis, often starting in childhood, involves chronic inflammation, itching, and dry, scaly skin. It is influenced by genetic and environmental factors. On the other hand, seborrheic dermatitis primarily affects oil-rich areas like the scalp and face, leading to greasy, red skin with yellow or white scales. Yeast overgrowth and hormonal factors play a significant role in its development. Understanding the differences between these dermatitis types is crucial for accurate diagnosis and effective management.
What is Atopic Dermatitis?

Atopic dermatitis, commonly known as eczema, is a chronic inflammatory skin condition that typically begins in childhood but can persist into adulthood. Acne is characterized by itchy, dry and irritated skin which often features redness or scaling. The exact cause of atopic dermatitis is complex and involves a combination of genetic predisposition and environmental triggers. People with a family history of allergies or asthma are more prone to developing atopic dermatitis.
The condition is linked to an overactive immune response to various allergens and irritants, leading to skin barrier dysfunction and increased susceptibility to inflammation. Common areas affected include the flexural folds of the body (like the elbows and knees), as well as the face and neck. Management involves the use of moisturizers, avoiding triggers, and using topical corticosteroids or immunomodulators during flare-ups.
Symptoms and Presentation
Atopic dermatitis, also known as eczema, is characterized by a range of symptoms and presentations that can vary in intensity and appearance. Common symptoms and presentations of atopic dermatitis include:
- Intense Itching (Pruritus): One of the most prominent features of atopic dermatitis is severe itching, which can be extremely uncomfortable and lead to scratching. Scratching can further worsen the condition and potentially cause skin infections.
- Dry and Flaky Skin: The affected skin tends to be dry, rough, and scaly. It may feel “rough like sandpaper.” This dryness is a result of the skin’s impaired ability to retain moisture.
- Redness (Erythema): The skin appears red or inflamed due to the underlying inflammatory response. In some cases, the redness can be widespread.
- Inflammation: Inflamed areas of the skin may be swollen, warm to the touch, and tender. The immune response contributes to this inflammation.
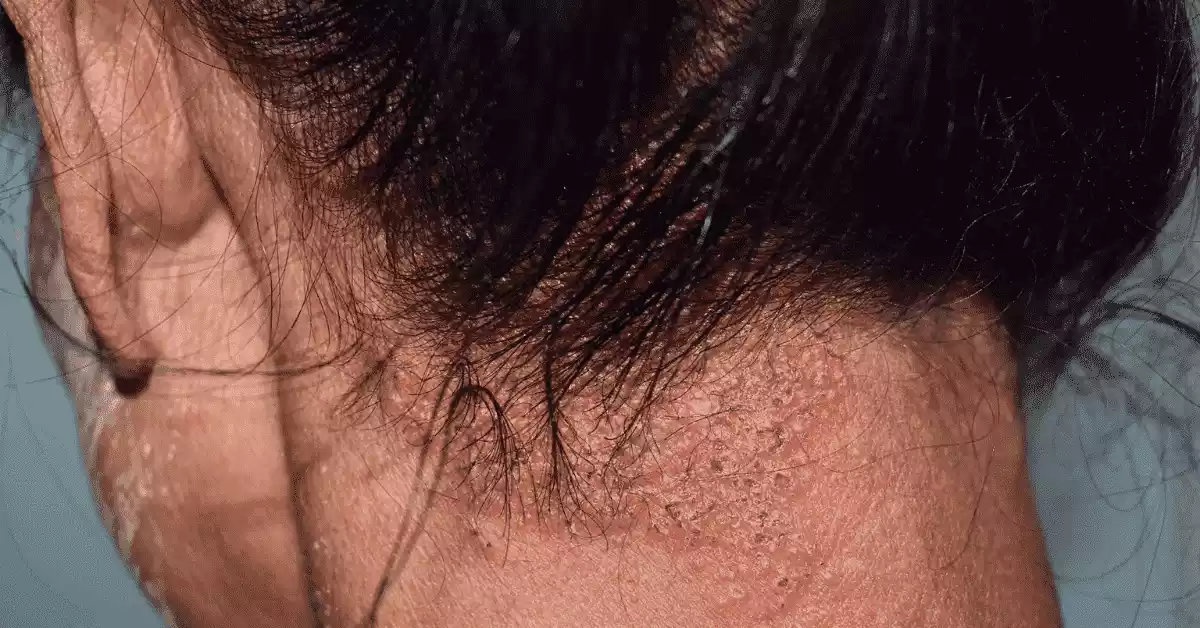
- Raised Bumps or Papules: Small, raised bumps known as papules can develop on the skin’s surface, often surrounding hair follicles. Scratching can lead to these papules becoming more prominent.
- Weeping or Oozing Blisters: In severe cases, blisters may form, and these can rupture, leading to oozing of fluid. Liquid then dries to form a crust over your face.
- Lichenification: Prolonged scratching and rubbing can cause the skin to thicken and develop a leathery texture, a condition known as lichenification.
- Flexural Involvement: Atopic dermatitis often affects the flexural areas of the body, such as the insides of the elbows and knees. These areas may be particularly prone to irritation and flare-ups.
- Face and Neck: In infants and young children, atopic dermatitis often appears on the face, especially on the cheeks and chin. In older children and adults, it can affect the neck, as well.
- Sleep Disturbances: Itching and discomfort from atopic dermatitis can disrupt sleep, leading to irritability and daytime fatigue.
- Secondary Infections: Due to the compromised skin barrier, there’s a higher risk of secondary bacterial or viral skin infections.
It’s important to note that atopic dermatitis symptoms can vary widely among individuals and across age groups. Infants and children may have different presentation patterns compared to adults. Proper diagnosis and management, often involving a dermatologist’s expertise, can help alleviate symptoms and improve quality of life for those affected by atopic dermatitis.
Causes of Atopic Dermatitis
Causes of atopic dermatitis are:
- Genetics: Family history of allergies and atopic conditions increases susceptibility.
- Immune Dysfunction: Dysregulated immune responses lead to inflammation and skin barrier disruption.
- Skin Barrier Dysfunction: Impaired skin barrier function allows moisture loss and irritants to penetrate.
- Environmental Triggers: Allergens, irritants, temperature changes, and humidity affect flare-ups.
- Allergies: Reactions to certain allergens can exacerbate or trigger symptoms.
- Microbial Factors: Skin microbiota imbalances may contribute to inflammation.
- Early-Life Exposures: Factors like early antibiotic use and exposure to allergens can influence risk.
- Stress: Psychological stress can exacerbate symptoms.
- Climate: Dry and cold weather can worsen skin dryness and irritation.
What is Seborrheic Dermatitis?
Seborrheic dermatitis is a common skin condition characterized by red, inflamed skin covered with greasy or oily scales. It primarily affects areas of the body that have a high density of oil glands, such as the scalp, face (particularly the nasolabial folds and eyebrows), and chest. The condition is often linked to an overgrowth of a type of yeast called Malassezia on the skin. Hormonal factors, stress, and certain medical conditions can also contribute to its development.
Seborrheic dermatitis can range from mild dandruff to more severe cases with significant redness and itching. While it is not fully understood, the condition involves an inflammatory response to the presence of yeast and its metabolic byproducts on the skin. Treatment options include medicated shampoos containing antifungal agents, topical antifungal creams or gels, and occasionally topical corticosteroids for managing acute flare-ups.
Symptoms and Presentation of Seborrheic Dermatitis
Seborrheic dermatitis is characterized by specific symptoms and presentations that primarily affect areas of the body rich in oil glands. The severity and appearance of these symptoms can vary, but common features of seborrheic dermatitis include:
- Greasy Scales: Affected areas of the skin, particularly the scalp and face, develop greasy or oily scales. These scales may appear yellowish or white and can range in size from small flakes to larger, more prominent patches.
- Itching: Seborrheic dermatitis is often associated with mild to moderate itching. While the itching is generally not as intense as in other forms of dermatitis, it can still cause discomfort.
- Redness and Inflammation: The skin underneath the scales can appear red and inflamed, particularly in areas where scales are more pronounced.
- Scalp Involvement (Dandruff): Seborrheic dermatitis commonly affects the scalp, resulting in dandruff. This involves the shedding of skin flakes from the scalp that may be visible on hair, clothing, and shoulders.
- Face Involvement: The condition can also affect facial areas, such as the nasolabial folds (the sides of the nose), eyebrows, and the skin between the eyebrows. The scales on the face can resemble those on the scalp.
- Cradle Cap (Infants): In infants, seborrheic dermatitis is referred to as “cradle cap.” It appears as thick, yellowish or brownish scales on the scalp and may extend to the forehead and eyebrows.
- Worse in Certain Conditions: Symptoms of seborrheic dermatitis may worsen in response to various factors, including stress, hormonal changes, cold and dry weather, and use of certain hair care products or cosmetics.
- Flare-Ups and Remissions: The condition often follows a pattern of flare-ups and remissions, with periods of heightened symptoms followed by periods of relative calm.
- Other Areas: While most common on the scalp and face, seborrheic dermatitis can occasionally affect other areas rich in oil glands, such as the chest, back, and skin folds.
- Thicker Scales (In Severe Cases): In severe cases, the scales can become thicker and more adherent, requiring more intensive treatment.
It’s important to differentiate seborrheic dermatitis from other skin conditions, especially psoriasis, as the two can have overlapping symptoms. Proper diagnosis by a dermatologist is essential for effective treatment. Mild cases of seborrheic dermatitis may respond well to over-the-counter treatments, while more severe or persistent cases may require prescription medications or medical guidance for management.
Causes of Seborrheic Dermatitis
Causes of seborrheic dermatitis include:
- Yeast Overgrowth (Malassezia): Excessive growth of the Malassezia yeast on the skin’s surface triggers an inflammatory response.
- Sebum Production: Elevated skin oil (sebum) production provides an environment for yeast proliferation.
- Hormonal Factors: Hormonal changes influence sebum production and may contribute, particularly during puberty.
- Genetic Predisposition: Family history and specific genes play a role in susceptibility.
- Immune System Response: Malassezia presence activates the immune system, leading to inflammation.
- Stress and Lifestyle: Stress, exhaustion, and certain lifestyle factors can worsen symptoms.
- Weather and Environment: Cold, dry weather and changes in humidity can trigger or exacerbate the condition.
- Immunosuppression: Conditions or medications weakening the immune system can increase risk.
Comparison Table of Atopic and Seborrheic Dermatitis
Here’s a comparison table outlining the key differences between atopic dermatitis and seborrheic dermatitis:
| Aspect | Atopic Dermatitis | Seborrheic Dermatitis |
|---|---|---|
| Definition | Chronic inflammatory skin condition | Common skin condition with greasy scales |
| Onset | Typically starts in childhood | Can occur at any age, including infancy |
| Genetic Link | Strong family history and genetic predisposition | Family history may increase risk |
| Affected Areas | Flexural areas, face, neck, hands | Scalp, face (nasolabial folds, eyebrows), chest |
| Appearance | Dry, scaly, red, inflamed skin | Greasy scales, redness, sometimes inflammation |
| Itching | Intense itching, often severe | Mild to moderate itching |
| Triggers | Allergens, irritants, environmental factors | Yeast overgrowth (Malassezia), stress, hormones |
| Skin Barrier | Impaired, leading to dryness and inflammation | Barrier dysfunction, greasy scales |
| Age Groups | Primarily affects children and infants | Affects various age groups, including adults |
| Stress Impact | Stress can worsen symptoms and flare-ups | Stress can exacerbate symptoms |
| Location | Commonly found in flexural areas (elbows, knees) | Often localized to oil-rich areas (scalp, face) |
| Secondary Infections | Risk due to scratching and compromised skin | Risk due to compromised skin barrier |
| Treatments | Emollients, topical corticosteroids, immunomodulators | Medicated shampoos, topical antifungals, corticosteroids |
| Management | Avoiding triggers, moisturizing, lifestyle changes | Managing yeast overgrowth, reducing inflammation |
| Medical Guidance | Often requires medical attention and treatment | May require medical guidance for effective management |
How to Diagnosis of Atopic and Seborrheic Dermatitis

Diagnosis of Atopic Dermatitis
Diagnosing atopic dermatitis usually involves a combination of medical history, physical examination, and exclusion of other conditions. A dermatologist or healthcare provider typically follows these steps:
-
- Medical History: The doctor will ask about your symptoms, when they started, family history of skin conditions, allergies, and any triggers that worsen your symptoms.
- Physical Examination: The doctor will examine your skin to assess the appearance, distribution of rashes, and any signs of itching, redness, scaling, or inflammation.
- Diagnostic Criteria: Atopic dermatitis is often diagnosed based on established diagnostic criteria, such as the Hanifin and Rajka criteria or the U.K. Working Party’s diagnostic criteria.
- Exclusion of Other Conditions: The doctor may rule out other skin conditions that may mimic atopic dermatitis, such as contact dermatitis, psoriasis, or fungal infections.
- Patch Testing: If allergies are suspected, patch testing might be conducted to identify specific allergens triggering your symptoms.
Diagnosis of Seborrheic Dermatitis
Diagnosing seborrheic dermatitis also involves a combination of medical history, physical examination, and sometimes additional tests:
-
- Medical History: The doctor will ask about your symptoms, when they started, any associated factors (like stress), and any treatments you’ve tried.
- Physical Examination: The doctor will closely examine the affected areas, such as the scalp, face, or other regions, looking for greasy scales, redness, and signs of inflammation.
- Clinical Appearance: Seborrheic dermatitis often has a characteristic appearance, with greasy scales in areas rich in oil glands.
- Differential Diagnosis: The doctor may differentiate seborrheic dermatitis from other skin conditions that might look similar, such as psoriasis or contact dermatitis.
- Skin Scraping: In some cases, the doctor might perform a skin scraping to examine under a microscope and confirm the presence of yeast (Malassezia).
Both conditions require accurate diagnosis by a healthcare professional or dermatologist. Self-diagnosis is not recommended, as other skin conditions can mimic their symptoms. Once diagnosed, appropriate treatment and management strategies can be tailored to your specific condition.
Treatment for Atopic Dermatitis
Treatment for atopic dermatitis includes:
- Emollients: Regular use of moisturizers to keep skin hydrated.
- Topical Corticosteroids: Anti-inflammatory creams for flare-ups.
- Topical Calcineurin Inhibitors: Non-steroidal creams to manage inflammation.
- Antihistamines: Relieve itching and improve sleep quality.
- Avoiding Triggers: Identifying and avoiding irritants and allergens.
- Bathing Practices: Short, lukewarm baths using mild cleansers.
- Prescription Medications: Oral medications or light therapy for severe cases.
- Stress Management: Techniques to reduce stress-related flare-ups.
- Allergen Management: Testing and avoidance if allergies play a role.
- Education and Lifestyle: Learning about triggers and skincare.
Work with a healthcare provider for personalized care.
Treatment for Seborrheic Dermatitis
Treatment for seborrheic dermatitis includes:
- Medicated Shampoos: Using shampoos containing antifungal agents like ketoconazole or selenium sulfide for scalp involvement.
- Topical Antifungals: Applying antifungal creams or lotions to affected skin areas.
- Topical Corticosteroids: Low-strength corticosteroid creams for inflammation.
- Topical Calcineurin Inhibitors: Non-steroidal creams to reduce inflammation.
- Regular Shampooing: Frequent and gentle shampooing to manage scalp symptoms.
- Cradle Cap (Infants): Gentle washing and brushing to remove scales.
- Stress Management: Reducing stress to prevent flare-ups.
- Lifestyle Adjustments: Avoiding triggers like harsh skincare products.
Consult a healthcare provider or dermatologist for personalized treatment recommendations based on the severity and location of your seborrheic dermatitis.
Preventive Measures
Preventive measures play a significant role in managing both atopic dermatitis and seborrheic dermatitis. While complete prevention may not always be possible, these steps can help reduce the frequency and severity of flare-ups:
For Atopic Dermatitis:
-
- Moisturize Regularly: Keep your skin well-hydrated with fragrance-free moisturizers to maintain the skin barrier.
- Avoid Irritants: Use mild, fragrance-free cleansers and detergents. Avoid harsh soaps and products with potential allergens.
- Identify Triggers: Determine your specific triggers (allergens, stress) and take steps to avoid or minimize exposure.
- Manage Stress: Stress can exacerbate symptoms, so practice stress management techniques like mindfulness and relaxation.
- Proper Bathing: Take short, lukewarm baths, and pat your skin dry gently after bathing.
- Comfortable Clothing: Wear soft, breathable fabrics that minimize irritation.
- Allergen Management: If allergies contribute, follow allergist-recommended strategies for avoidance.
- Avoid Scratching: Trim your nails and use strategies to minimize scratching to prevent skin damage and infections.
For Seborrheic Dermatitis:
-
- Regular Shampooing: Maintain good scalp hygiene with regular use of medicated shampoos containing antifungal agents.
- Topical Treatments: Apply antifungal creams or lotions to affected areas as directed by your healthcare provider.
- Gentle Skin Care: Use mild cleansers and avoid excessive scrubbing, which can exacerbate symptoms.
- Stress Management: Stress reduction techniques can help prevent flare-ups.
- Avoid Oil-Based Products: In cases of facial seborrheic dermatitis, avoid heavy oil-based cosmetics or skincare products.
- Sun Protection: Protect your skin from excessive sun exposure, as sunburn can worsen symptoms.
- Healthy Lifestyle: Eat a balanced diet, exercise regularly, and get adequate sleep to support overall skin health.
- Consult a Professional: If over-the-counter treatments are not effective, consult a healthcare provider or dermatologist for personalized recommendations.
Remember that consistency in following these preventive measures is essential for long-term management. Since triggers and sensitivities can vary from person to person, it’s important to identify what works best for you through trial and observation. If your symptoms persist or worsen, seeking medical advice is recommended for proper management.
Overlapping Challenges
Overlapping challenges in atopic dermatitis and seborrheic dermatitis include:
- Itching: Both conditions often cause itching, leading to discomfort and potential skin damage.
- Inflammation: Inflammation is a shared feature, contributing to redness and discomfort.
- Impact on Appearance: Both conditions can affect appearance and self-esteem due to visible symptoms.
- Chronic Nature: They are chronic conditions, with symptoms that can persist over time.
- Triggers: Environmental factors, stress, and allergens can trigger or worsen both conditions.
- Management: Effective management requires personalized approaches, often involving skincare, lifestyle changes, and medical treatments.
- Quality of Life: Flare-ups impact daily life, potentially causing sleep disturbances and emotional distress.
Navigating these shared challenges involves understanding individual triggers, seeking professional guidance, and adopting strategies that address both physical symptoms and emotional well-being.
Lifestyle Management
Lifestyle management is crucial for individuals with atopic dermatitis and seborrheic dermatitis to help prevent flare-ups, reduce symptoms, and improve overall skin health. Here are lifestyle management tips for both conditions:
For Atopic Dermatitis:
-
- Hydration: Be sure to drink enough water throughout the day in order to hydrate your skin from within.
- Diet: Maintain a balanced diet rich in nutrients that support skin health, such as omega-3 fatty acids found in fish and antioxidants from fruits and vegetables.
- Avoid Allergens: Identify and avoid allergens that trigger your symptoms, such as certain foods, pollen, pet dander, or dust mites.
- Stress Reduction: Practice stress management techniques like deep breathing, meditation, yoga, or engaging in hobbies.
- Hygiene: Use mild, fragrance-free soaps and detergents to prevent skin irritation. Avoid hot water and harsh scrubbing.
- Avoid Overheating: Excessive heat and sweating can worsen itching, so dress in layers and avoid overheated environments.
- Moisturize: Apply a fragrance-free moisturizer regularly to maintain skin hydration and barrier function.
- Clothing: Choose loose-fitting, breathable clothing to reduce discomfort and friction.
For Seborrheic Dermatitis:
-
- Diet: Similar to atopic dermatitis, a balanced diet rich in nutrients supports overall skin health.
- Regular Cleansing: Maintain proper scalp hygiene by regularly shampooing with medicated shampoos containing antifungal agents.
- Stress Management: Manage stress through relaxation techniques, hobbies, and activities you enjoy.
- Gentle Skincare: Use gentle cleansers and avoid harsh scrubbing, especially on affected areas.
- Sun Protection: Protect your skin from excessive sun exposure by using sunscreen and wearing protective clothing.
- Avoid Oil-Based Products: Choose non-comedogenic (non-oil-based) cosmetics and skincare products.
- Regular Checkups: Schedule regular visits with your healthcare provider or dermatologist to monitor your condition.
- Healthy Lifestyle: Prioritize regular exercise, adequate sleep, and a balanced diet for overall well-being.
Remember that maintaining a healthy lifestyle can contribute not only to managing your skin condition but also to your overall quality of life. While lifestyle adjustments can be beneficial, they should be combined with appropriate medical treatments and guidance from healthcare professionals for the best outcomes.
Summary
Atopic Dermatitis and Seborrheic Dermatitis are common skin conditions that can significantly impact quality of life. While their causes and presentations differ, both conditions benefit from a combination of proper skincare, stress management, identifying triggers, and, when needed, medical treatments.
Personalized approaches, guided by healthcare professionals, can help individuals effectively manage symptoms, reduce flare-ups, and improve overall skin health. It’s important to stay proactive, attentive to triggers, and consistent in adopting preventive measures and lifestyle adjustments to enjoy a better quality of life despite these dermatological challenges.



