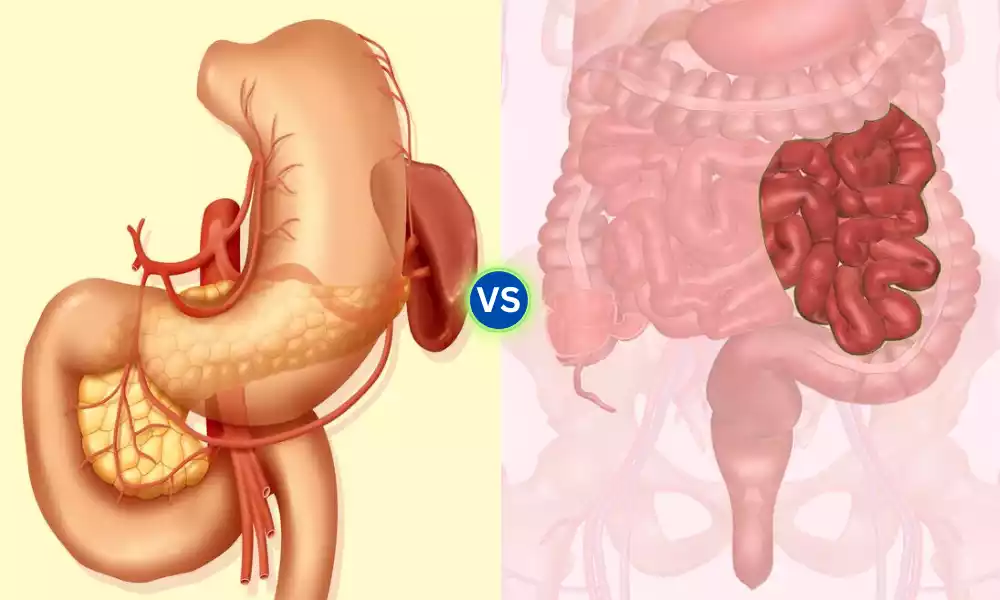
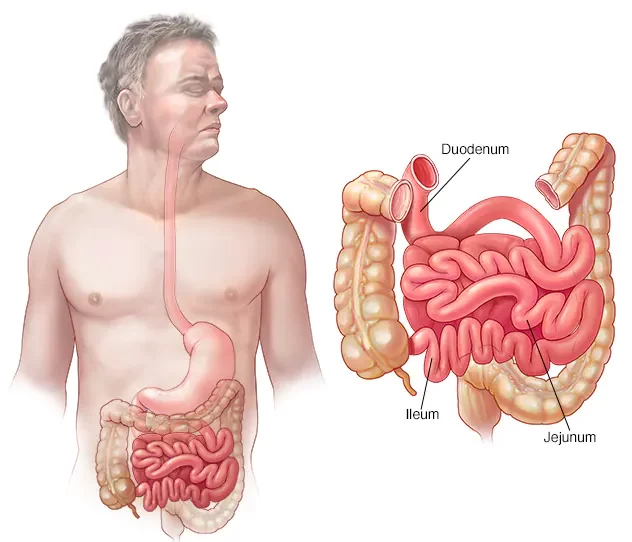
Duodenum and Jejunum are the first two sections of the small intestine, playing a pivotal role in the digestion and absorption of nutrients. The duodenum, measuring about 10-12 inches in length, follows the stomach and serves as a critical junction for the mixing of chyme (partially digested food) with bile from the liver and gallbladder, and digestive enzymes from the pancreas.
Following the duodenum, the jejunum extends for approximately two-fifths of the remaining length of the small intestine. It is primarily involved in the absorption of carbohydrates and proteins. The specialized structure of these segments, featuring villi and microvilli, provides an extensive surface area to facilitate effective digestion and nutrient uptake.
What is Duodenum?
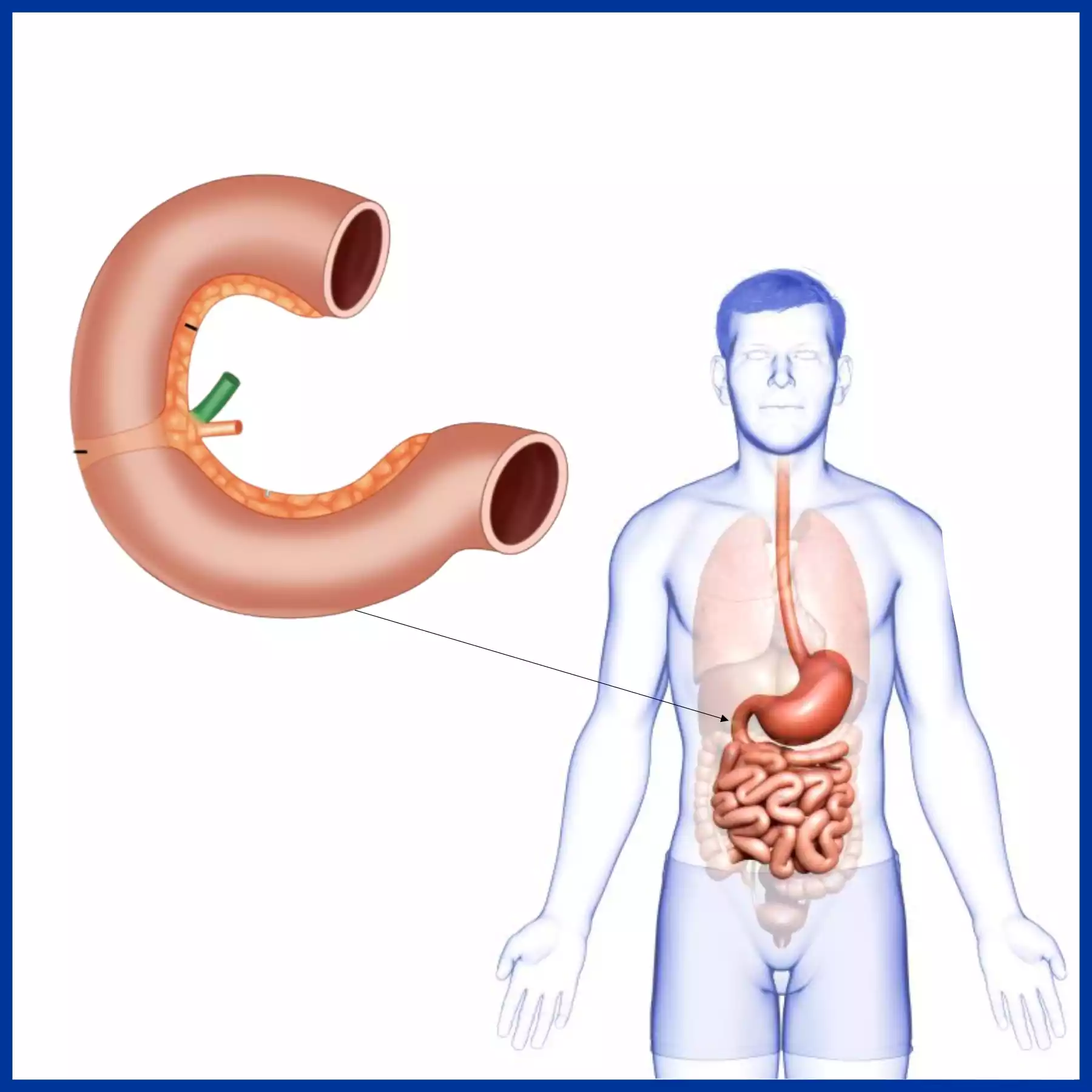
The duodenum is the first section of the small intestine in humans and most vertebrates. Located immediately beyond the stomach, it plays a crucial role in the initial stages of the digestive process.
Here are some key features and functions of the duodenum:
- Length and Location: Typically about 10-12 inches (25-30 cm) long, the duodenum begins at the pyloric sphincter of the stomach and ends at the jejunum, the next segment of the small intestine.
- Function: The duodenum is the primary site for the mixing of gastric contents (chyme) with digestive enzymes and bile. These enzymes, secreted by the pancreas, and bile, produced by the liver and stored in the gallbladder, aid in the digestion of fats, proteins, and carbohydrates.
- Sections: The duodenum can be divided into four parts:
- The superior part (first part) is located at the level of the vertebra L1.
- The descending part (second part) is where the openings for the bile and pancreatic ducts are located.
- The horizontal part (third part) passes in front of the vertebral column.
- The ascending part (fourth part) connects to the jejunum.
- Duodenal Wall: The lining of the duodenum has several folds, called plicae circulares, and tiny finger-like projections called villi. These structures increase the surface area for absorption and secretion.
- Duodenal Ulcers: The duodenum is a common site for ulcer formation, known as duodenal ulcers. These ulcers can develop due to various reasons, including an imbalance between the stomach’s acidic secretions and the ability of the duodenal lining to defend itself.
The duodenum plays a fundamental role in ensuring that the foods we eat are broken down into absorbable nutrients to be utilized by our bodies.
What is Jejunum?
The jejunum is the second section of the small intestine in humans and many vertebrates, situated between the duodenum and the ileum. It is central to the digestive process, particularly in the absorption of nutrients.
Here are some key features and functions of the jejunum:
- Location and Length: The jejunum starts where the duodenum ends and comprises approximately the upper two-fifths of the remaining part of the small intestine. Its exact length can vary, but it typically ranges between 6 to 8 feet (1.8 to 2.4 meters).
- Structure: Like other parts of the small intestine, the jejunum’s lining has numerous plicae circulares (circular folds), villi, and microvilli. These structures significantly increase its surface area, enhancing absorption of digested nutrients.
- Function: The jejunum is chiefly responsible for the absorption of carbohydrates and proteins. As chyme (semi-liquid food) moves through the jejunum, nutrients are absorbed through the mucosal lining and into the bloodstream.
- Distinctive Characteristics: Compared to the duodenum and the ileum, the jejunum has a thicker wall, is typically more vascular (having more blood vessels), and has a deeper red color. Its circular folds are also more pronounced, reflecting its primary role in absorption.
- Relation to the Mesentery: The jejunum is attached to the posterior wall of the abdomen by a fold of peritoneum called the mesentery. This structure provides the jejunum with mobility and contains the blood vessels, nerves, and lymphatics that supply the intestine.
The jejunum is a vital component of the digestive system, ensuring that the body effectively absorbs the essential nutrients from the food we consume.
Comparison table of Duodenum and Jejunum
Here’s a comparison table highlighting the differences and similarities between the duodenum and jejunum:
| Feature/Aspect | Duodenum | Jejunum |
|---|---|---|
| Location | First section of the small intestine | Second section of the small intestine |
| Length | Approximately 10-12 inches (25-30 cm) | Approximately 6-8 feet (1.8-2.4 meters) |
| Function | Receives chyme from stomach and mixes it with bile and pancreatic enzymes | Primarily involved in the absorption of carbohydrates and proteins |
| Appearance | Relatively shorter and wider | Longer with a thicker wall and more vascular, giving it a deeper red color |
| Structural Features | Has four distinct sections (superior, descending, horizontal, ascending) | Prominent plicae circulares and villi for increased absorption |
| Connections | Connected to the stomach at the pyloric sphincter | Begins where the duodenum ends and leads to the ileum |
| Notable Structures | Has the major and minor duodenal papillae, which are openings for bile and pancreatic ducts | No specific openings; more uniform in structure |
| Associated Conditions | Common site for duodenal ulcers due to stomach acid | Less common for ulcers; issues usually arise from malabsorption |
| Position in Mesentery | Mostly retroperitoneal (only the first part is intraperitoneal) | Entirely intraperitoneal, suspended by the mesentery |
This table provides a concise comparison between the two, although it’s essential to understand that both are continuous parts of the same organ (small intestine) and function collaboratively in the digestive process.
Importance of the difference between Duodenum and Jejunum
The distinction between the duodenum and jejunum is pivotal for various reasons, both anatomically and functionally:
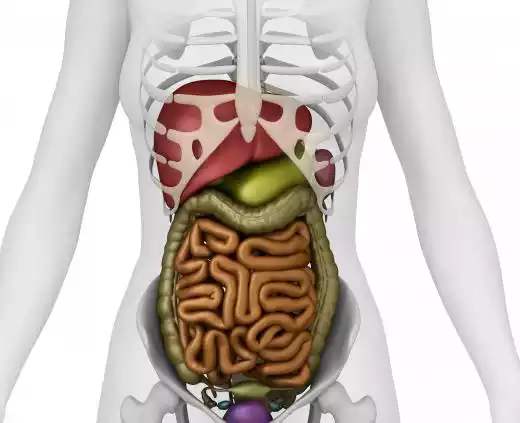
- Position and Structure: Anatomically, the duodenum is positioned immediately after the stomach, forming a C-shaped curve around the head of the pancreas, while the jejunum follows the duodenum and occupies the central part of the abdominal cavity. Recognizing this arrangement is crucial for surgical interventions and diagnostic imaging.
- Digestive Role: The duodenum is the site where acidic chyme from the stomach mixes with bile from the liver and digestive enzymes from the pancreas. This mixing and neutralization process sets the stage for further digestion and absorption in the jejunum and beyond.
- Absorptive Capacity: The jejunum, with its longer villi and extensive surface area, is the primary site for nutrient absorption. While the duodenum absorbs certain minerals and vitamins, the jejunum is primarily responsible for the absorption of digested carbohydrates, proteins, and fats.
- Hormonal Regulation: The duodenum releases hormones like cholecystokinin (CCK) and secretin in response to its contents. These hormones play a role in regulating digestive enzyme secretion, bile release, and stomach emptying. Understanding this regulation is vital for certain clinical conditions.
- Clinical Implications: Certain disorders may preferentially affect one part over the other. For instance, duodenal ulcers are more common than jejunal ones, while celiac disease tends to affect the proximal parts of the small intestine, including the duodenum and upper jejunum.
- Surgical Considerations: In bariatric surgeries or trauma cases, understanding the difference between the two sections becomes crucial to determine the site of intervention or to assess the extent of injury.
The differentiation between the duodenum and jejunum is crucial for a comprehensive understanding of gastrointestinal physiology, pathology, and clinical medicine. Their individual roles in digestion and absorption underscore the importance of their distinction in both health and disease.
Clinical Significance
The duodenum and jejunum, given their essential roles in digestion and absorption, are involved in various clinical conditions and disorders. Understanding their clinical significance aids healthcare professionals in diagnosing, treating, and managing diseases and conditions related to these segments of the small intestine.
Here are some of the clinical aspects related to the duodenum and jejunum:
- Duodenal Ulcers: A common clinical condition where erosions occur in the mucosal lining of the duodenum. It’s typically caused by Helicobacter pylori infection or prolonged use of nonsteroidal anti-inflammatory drugs (NSAIDs). Symptoms might include burning stomach pain, bloating, and nausea.
- Celiac Disease: An autoimmune condition where ingestion of gluten (a protein found in wheat, barley, and rye) leads to damage in the small intestine, primarily affecting the duodenum and jejunum. This can result in malabsorption of nutrients, leading to symptoms like diarrhea, weight loss, and anemia.
- Duodenal Atresia: A congenital disorder where a part of the duodenum is not developed, causing a blockage. It’s often diagnosed shortly after birth due to symptoms like vomiting and abdominal distension.
- Jejunal and Duodenal Polyps: These are growths that can form on the mucosal lining. While most are benign, some can be precancerous. They might be associated with certain syndromes like Familial Adenomatous Polyposis.
- Crohn’s Disease: A type of inflammatory bowel disease that can affect any part of the gastrointestinal tract, including the jejunum. Symptoms might include abdominal pain, diarrhea, weight loss, and fatigue.
- Gastrointestinal Bleeding: Both the duodenum and jejunum can be sites of bleeding, often detected when a patient presents with melena (dark, tarry stools) or anemia.
- Bile and Pancreatic Duct Issues: The duodenum is where the common bile duct and the pancreatic duct empty. Issues like gallstones or tumors can block these ducts, leading to jaundice, pancreatitis, or other complications.
- Short Bowel Syndrome: This condition arises when a significant portion of the small intestine (including parts of the jejunum) is removed or nonfunctional, leading to malabsorption and nutrient deficiencies.
- Intestinal Obstructions: Any blockages in the duodenum or jejunum can prevent the normal flow of chyme, leading to symptoms like vomiting, abdominal pain, and constipation.
- Intussusception: A condition where one segment of the intestine “telescopes” into an adjacent segment, leading to an obstruction. It can sometimes involve the jejunum.
Understanding these clinical conditions and their presentation is pivotal for early diagnosis and effective treatment. Modern medical imaging techniques like endoscopy, MRI, and CT scans, along with various laboratory tests, play a significant role in diagnosing and managing these conditions related to the duodenum and jejunum.
Disorders related to Duodenum and Jejunum
The duodenum and jejunum are integral parts of the digestive process, and various disorders can affect their function. Here’s a list of some disorders specifically related to these segments of the small intestine:
- Duodenal Ulcers: Erosions in the mucosal lining of the duodenum often caused by Helicobacter pylori infection or chronic NSAID use.
- Duodenal Atresia: A congenital condition where a part of the duodenum fails to develop, causing obstruction.
- Duodenal Stenosis: A narrowing of the duodenal lumen which can be congenital or acquired due to ulcers or tumors.
- Celiac Disease: An autoimmune condition that affects the proximal small intestine, including the duodenum and jejunum. Ingestion of gluten leads to inflammation and villous atrophy, impairing nutrient absorption.
- Crohn’s Disease: A type of inflammatory bowel disease, it can affect any part of the GI tract but when it involves the jejunum, it’s sometimes referred to as jejunoileitis.
- Jejunal and Duodenal Polyps: Benign growths in the lining which can be sporadic or associated with genetic syndromes like Familial Adenomatous Polyposis or Peutz-Jeghers syndrome.
- Duodenal Switch Surgery: A type of bariatric surgery that involves rerouting a significant portion of the small intestine, affecting the function of the duodenum and jejunum.
- Duodenal and Jejunal Diverticula: Pouch-like outpouchings of the mucosa and submucosa. While most are asymptomatic, they can sometimes become inflamed or infected.
- Superior Mesenteric Artery Syndrome (SMAS): A rare vascular disorder where the third part of the duodenum is compressed between the superior mesenteric artery and the aorta, leading to obstruction.
- Parasitic Infections: Certain parasites like Giardia lamblia primarily affect the duodenum and jejunum leading to malabsorption and diarrhea.
- Tumors: Both benign and malignant tumors can occur in the duodenum and jejunum. Examples include adenocarcinomas, carcinoids, and gastrointestinal stromal tumors (GISTs).
- Nonsteroidal Anti-Inflammatory Drug (NSAID) Enteropathy: Chronic use of NSAIDs can cause damage to the mucosa of the small intestine, including the jejunum, leading to ulcers and bleeding.
- Zollinger-Ellison Syndrome: A rare condition where one or more tumors form in the pancreas or duodenum, leading to the excessive production of stomach acid. This can result in severe, recurring peptic ulcers in the duodenum.
It’s essential to understand that while some of these disorders may primarily affect the duodenum or jejunum, the entire gastrointestinal system is interconnected. Therefore, disorders in one section can influence the function of other sections. Proper diagnosis, often involving endoscopy, imaging, and laboratory tests, is crucial for effective management and treatment.
Treatment Approaches
Treatment approaches for disorders of the duodenum and jejunum vary based on the specific condition, its severity, and the overall health of the patient. Here’s a general overview of treatment modalities for some of the disorders mentioned:
- Duodenal Ulcers:
- Medications: Proton pump inhibitors (PPIs) like omeprazole, H2 blockers like ranitidine, and antacids to reduce stomach acid.
- Antibiotics: To treat Helicobacter pylori infections.
- Lifestyle changes: Avoiding spicy foods, alcohol, and smoking; managing stress.
- Surgery: Rarely needed, but may be done in cases of bleeding, perforation, or obstruction.
- Duodenal Atresia:
- Surgery: To correct the atresia and establish intestinal continuity.
- Celiac Disease:
- Gluten-free diet: The mainstay of treatment, avoiding wheat, barley, and rye.
- Vitamin and mineral supplements: To address any deficiencies.
- Crohn’s Disease:
- Anti-inflammatory drugs: Such as corticosteroids and aminosalicylates.
- Immune system suppressors: Like azathioprine, methotrexate, and biologics (e.g., infliximab).
- Antibiotics: To treat or prevent infections.
- Surgery: To remove damaged sections in severe cases.
- Jejunal and Duodenal Polyps:
- Endoscopic removal: Polyps can often be removed during an endoscopy.
- Surgical resection: In cases of larger or malignant polyps.
- Superior Mesenteric Artery Syndrome (SMAS):
- Nutritional support: Including nasogastric decompression.
- Surgical intervention: Duodenojejunostomy may be done in severe cases.
- Parasitic Infections (e.g., Giardia):
- Antiparasitic medications: Such as metronidazole or tinidazole.
- Tumors:
- Surgery: To remove the tumor.
- Chemotherapy or radiation: Depending on the tumor type and stage.
- Targeted therapies: For specific types of tumors like GISTs.
- NSAID Enteropathy:
- Discontinuation of NSAIDs: If possible.
- Proton pump inhibitors (PPIs): To reduce acid production.
- Misoprostol: To protect the stomach lining.
- Zollinger-Ellison Syndrome:
- Surgery: To remove the tumor.
- Medications: High-dose proton pump inhibitors to suppress acid production.
In many conditions affecting the duodenum and jejunum, dietary and lifestyle modifications play a significant role in management. Additionally, patient education, regular follow-up, and monitoring are crucial for optimal outcomes.
Conclusion
The Duodenum and Jejunum are integral segments of the small intestine, playing pivotal roles in the digestive process. The duodenum, as the first section post-stomach, receives chyme and is vital for the initial breakdown and neutralization of food, aided by bile and pancreatic secretions. The jejunum, following the duodenum, is the primary site for nutrient absorption, with its extensive surface area ensuring efficient uptake of digested components.
Both segments are susceptible to various disorders, from ulcers to congenital issues, and their proper function is crucial for overall nutritional health. Understanding their anatomy, function, and related disorders is essential for comprehensive healthcare and patient well-being.