Introduction
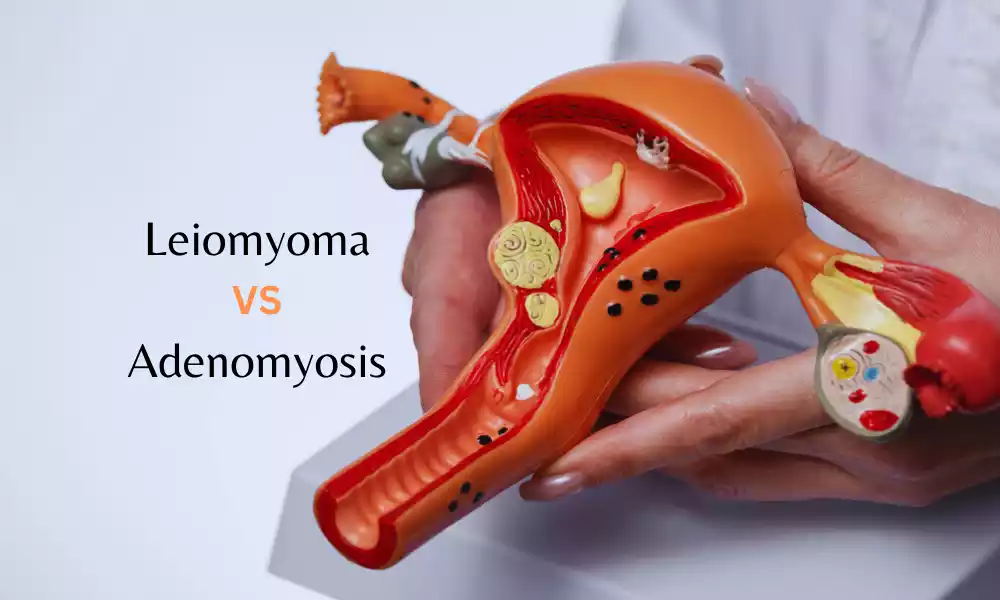
Gynecological conditions have long posed challenges in both diagnosis and treatment. Among the myriad conditions, leiomyoma and adenomyosis are often subjects of discussion due to their prevalence among women of reproductive age and their potential to cause significant symptoms. While they share some overlapping features, they are distinct entities, and understanding the differences between the two is paramount for clinicians and patients alike.
Definition of Leiomyoma
Leiomyoma, commonly known as uterine fibroids, is a benign (non-cancerous) tumor that originates from the smooth muscle layer (myometrium) of the uterus. These tumors can vary in size, from tiny, undetectable masses to large masses that can distort and enlarge the uterus. They can be single or multiple and can be located in different parts of the uterus (submucosal, intramural, or subserosal). The exact cause of leiomyoma is unknown, but its growth is often associated with estrogen and progesterone, two hormones that support the menstrual cycle.

Definition of Adenomyosis
Adenomyosis is a condition in which the inner lining of the uterus (the endometrium) breaks through the muscle wall of the uterus (the myometrium). This invasive endometrial tissue can lead to an enlarged uterus and can cause heavy or prolonged menstrual bleeding, pain, and cramping. Unlike endometriosis, where endometrial tissue grows outside the uterus, in adenomyosis, the tissue growth is confined within the uterine muscle. The exact cause of adenomyosis remains unclear, but the condition is commonly associated with middle-aged women and those who have had children.
Causes of Leiomyoma and Adenomyosis
Leiomyoma
The exact cause of leiomyoma is not entirely understood. Several factors contribute to their development:
- Hormonal Factors: Estrogen and progesterone, female hormones produced by the ovaries, promote the growth of leiomyomas. Fibroids contain more estrogen and progesterone receptors than normal uterine muscle cells.
- Genetic Factors: Fibroids have been linked to genetic changes. They may also run in families, implying a potential genetic component.
- Growth Factors: Insulin-like growth factor may also influence the growth of fibroids.
- Other Factors: Early onset of menstruation, obesity, and nulliparity (never giving birth) have been associated with an increased risk of developing fibroids.
Adenomyosis
The exact cause remains elusive, but several theories have been postulated:
- Invasive Tissue Growth: Direct invasion of the endometrial cells into the myometrium.
- Developmental Origins: Adenomyosis might originate within the uterine muscle from endometrial tissue deposited during fetal development.
- Uterine Inflammation: Following childbirth, inflammation of the uterine lining might cause a break in the normal boundary of cells.
- Stem Cell Origins: Bone marrow stem cells might invade the uterus, causing adenomyosis.
- Hormonal Factors: Like leiomyomas, estrogen plays a role in the disease’s pathogenesis.
Symptoms of Leiomyoma and Adenomyosis
Leiomyoma
Symptoms vary based on size, location, and number of tumors. They may include:
- Heavy menstrual bleeding: Resulting in anemia in some cases.
- Prolonged menstrual periods.
- Pelvic pain or pressure.
- Frequent urination.
- Difficulty emptying the bladder.
- Constipation.
- Back or leg pain.
Adenomyosis
The symptoms can be subtle or quite severe, including:
- Heavy or prolonged menstrual bleeding.
- Severe menstrual cramps.
- Pain during intercourse.
- Chronic pelvic pain.
- An enlarged uterus, often mimicking pregnancy.
Importance of Distinguishing Between Leiomyoma and Adenomyosis
- Diagnosis & Imaging: While both conditions can be identified using ultrasound and MRI, the distinguishing features can aid in precise diagnosis. Leiomyomas appear as well-defined, round masses, whereas adenomyosis presents as an asymmetrical thickening of the uterus with small cystic spaces.
- Treatment Approaches: Leiomyomas might be managed with medications, non-invasive radiological procedures, or surgical interventions such as myomectomy. Adenomyosis, on the other hand, has limited treatment options, including hormonal therapies and hysterectomy.
- Prognosis & Fertility Impact: While both conditions can affect fertility, the approach to managing fertility differs. For instance, submucosal fibroids directly impact the uterine cavity and often need removal to improve fertility outcomes. Adenomyosis can compromise implantation but the extent of its impact on fertility remains a subject of ongoing research.
- Symptom Overlap: Distinguishing the conditions is essential because their symptoms often overlap. Precise diagnosis ensures the appropriate management of symptoms, optimizing patient outcomes.
- Patient Education: Understanding the differences aids in informed decision-making. Patients can make choices about treatments, including surgical options, based on their condition and desired outcomes, such as retaining fertility.
Comparison table of Leiomyoma and Adenomyosis
Here’s a detailed comparison table:
| Feature | Leiomyoma (Uterine Fibroids) | Adenomyosis |
|---|---|---|
| Nature/Type | Benign smooth muscle tumor | Endometrial tissue within the myometrium |
| Origin | Myometrium (uterine muscle layer) | Endometrial glands and stroma migrating into the myometrium |
| Location in the Uterus | Can be submucosal (underneath the inner lining), intramural (within the muscle wall), or subserosal (outside the muscle wall) | Embedded within the myometrium |
| Appearance | Distinct masses or tumors that can vary in size and number | Diffuse or localized thickening of the uterine wall |
| Symptoms | May be asymptomatic, but can cause heavy menstrual bleeding, pelvic pain, pressure on nearby organs, frequent urination | Heavy and prolonged menstrual bleeding, severe menstrual cramps, chronic pelvic pain |
| Age of Onset | Often discovered during the 30s and 40s | Typically affects women aged 40-50 and those who’ve had children |
| Associated Factors | Possible links with hormonal levels, genetics, and other growth factors | Often linked with previous uterine surgeries or childbirth |
| Diagnosis | Ultrasound, MRI, Hysteroscopy | Transvaginal ultrasound, MRI |
| Treatment | Medications, myomectomy, hysterectomy, uterine artery embolization | Pain management, hormonal therapy, endometrial ablation, hysterectomy |
| Long-term Health Implications | Generally benign, but large fibroids can cause complications | Can lead to chronic pain and severe menstrual symptoms, but is benign |
While both leiomyoma and adenomyosis can have similar symptoms, their treatments and implications for fertility and health vary. Consulting with a gynecologist for proper diagnosis and treatment options is crucial.
Similarities between Leiomyoma and Adenomyosis
- Origin: Both conditions are related to the uterus and its tissues.
- Benign Nature: Both are benign conditions, meaning they are not cancerous and do not metastasize to other parts of the body.
- Symptoms: Both can lead to heavy menstrual bleeding (menorrhagia), pelvic pain, and a feeling of fullness in the lower abdomen.
- Age of Prevalence: They most commonly affect women in their reproductive years, especially those in their 30s and 40s.
- Hormonal Influence: Both conditions can be influenced by hormonal changes and can respond to hormonal therapies.
- Impact on Fertility: Both can potentially affect fertility and impact a woman’s ability to conceive, though this varies from person to person.
Diagnosis of Leiomyoma and Adenomyosis

Leiomyoma (Uterine Fibroids):
- Ultrasound: This imaging technique is often the first step, providing a visualization of fibroids.
- MRI: Offers detailed images of the uterus and is especially useful in mapping fibroids before surgical procedures.
- Hysteroscopy: Allows for a direct visual examination of the interior of the uterus.
- Lab Tests: On occasion, to rule out other potential causes of heavy menstrual bleeding.
Adenomyosis:
- Pelvic Examination: Initial assessment which may reveal an enlarged, tender uterus.
- Ultrasound: Especially transvaginal ultrasound, helps in visualizing the uterus, but findings can sometimes be non-specific.
- MRI: Considered a very accurate method for diagnosing adenomyosis.
- Endometrial Biopsy: While this cannot confirm adenomyosis, it’s useful for ruling out other conditions.
Treatment Approaches for Leiomyoma and Adenomyosis
Leiomyoma (Uterine Fibroids):
- Medications: These can regulate hormones, reduce symptoms, or shrink fibroids. Examples include GnRH analogs or birth control pills.
- Surgical:
- Myomectomy: Removal of fibroids while preserving the uterus.
- Hysterectomy: Removal of the uterus; it’s a definitive treatment.
- Uterine Artery Embolization: A procedure that blocks blood flow to fibroids, causing them to shrink.
Adenomyosis:
- Pain Management: NSAIDs or other pain-relief medications.
- Hormonal Treatments: Birth control pills, progestin therapy, or GnRH analogs to reduce heavy bleeding and pain.
- Focused Ultrasound Surgery: A non-invasive procedure that destroys the inner lining of the uterus using sound waves.
- Endometrial Ablation: Destroys the lining of the uterus to reduce or stop heavy bleeding.
- Hysterectomy: The removal of the uterus; considered the most definitive treatment for adenomyosis.
Prevention of Leiomyoma and Adenomyosis
Here’s a concise list of points to consider for the prevention and management of Leiomyoma (uterine fibroids) and Adenomyosis:
Prevention and Management of Leiomyoma:
- Regular Check-ups: Routine gynecological exams help detect fibroids early.
- Healthy Lifestyle: Maintain a balanced diet and regular exercise.
- Hormonal Monitoring: Be aware of any hormonal imbalances or unusual menstrual patterns.
- Avoid Environmental Toxins: Some studies suggest a link between fibroids and exposure to certain chemicals.
- Manage Blood Pressure: There’s evidence suggesting a correlation between high blood pressure and fibroids.
Prevention and Management of Adenomyosis:
- Routine Gynecological Exams: Helps in early detection and management.
- Hormonal Balance: Awareness of hormonal fluctuations can help manage symptoms.
- Pain Management: Use of NSAIDs during menstruation can reduce pain and inflammation.
- Consider Birth Control: Hormonal birth control might reduce symptoms.
- Seek Early Treatment: Addressing symptoms early can slow progression and improve quality of life.
While these points can aid in management, they don’t guarantee prevention. Regular consultations with healthcare professionals are essential.
Advancement in medical science for Leiomyoma and Adenomyosis
Medical science has continuously evolved, and over the past several decades, advancements in the understanding, diagnosis, and treatment of both leiomyoma and adenomyosis have emerged. These advancements offer patients better quality of life and more diverse treatment options.
Advancements in Leiomyoma (Uterine Fibroids):
- MRI-guided Focused Ultrasound Surgery (MRgFUS): A non-invasive procedure that uses ultrasound waves to heat and destroy fibroid tissue. This procedure is guided by magnetic resonance imaging (MRI) to accurately target fibroids.
- Laparoscopic Radiofrequency Ablation: Also known as Lap-RFA, this procedure uses a needle-like probe to transmit radiofrequency energy, heating and shrinking the fibroids.
- Genetic Research: Investigations into the genetic component of fibroids can lead to understanding their growth mechanisms, potentially leading to targeted therapies.
- Uterine Artery Embolization: While not entirely new, refinements in the procedure and materials used have made it more effective and safe. It involves blocking the blood supply to the fibroid, causing it to shrink.
- Advanced Imaging Techniques: Improved MRI and ultrasound capabilities offer more detailed visualization of fibroids, aiding in better diagnosis and treatment planning.
Advancements in Adenomyosis:
- High-intensity Focused Ultrasound (HIFU): Similar to its use in fibroids, HIFU can be used to target and destroy adenomyotic tissue non-invasively.
- Advanced Hormonal Therapies: Besides traditional hormone therapies, GnRH antagonists have been researched for adenomyosis treatment, offering potential advantages in symptom control.
- Endometrial Ablation Techniques: Newer technologies and techniques, like radiofrequency ablation, have been introduced, offering more efficient and less invasive ways to treat heavy menstrual bleeding associated with adenomyosis.
- Improved Diagnostic Capabilities: Advancements in imaging, especially MRI, have led to better differentiation between adenomyosis and other gynecological conditions.
- Research on Pathophysiology: Understanding the molecular and cellular mechanisms underlying adenomyosis can potentially open doors to innovative treatments. Recent studies focus on the role of stem cells and hormonal and inflammatory pathways.
- Ulipristal Acetate: A medication that affects progesterone receptor modulators, Ulipristal acetate has shown effectiveness in controlling symptoms of both adenomyosis and fibroids. Its long-term safety profile is still under study.
Future Prospects:
The increasing convergence of biotechnology, genetics, and clinical medicine promises even more advanced treatments in the near future. Personalized medicine, based on an individual’s genetic makeup, may offer targeted treatments for conditions like leiomyoma and adenomyosis.
As our understanding of these conditions deepens, especially at the molecular and cellular levels, more innovative therapies are anticipated.
Patients are advised to discuss with their healthcare providers to understand which advanced treatments are available and suitable for their specific conditions.
Conclusion
Leiomyoma and adenomyosis are distinct gynecological conditions with overlapping symptoms. Proper diagnosis is crucial as treatment approaches differ. While both conditions can significantly impact a woman’s life, understanding their differences and seeking appropriate medical intervention can lead to effective management and improved quality of life.