Introduction of Marfan Syndrome and Marfanoid Habitus
Marfan Syndrome: Marfan syndrome is a rare genetic disorder that affects the connective tissues of the body. It is caused by mutations in the FBN1 gene and can manifest as a wide range of physical and medical features, including long limbs, joint hypermobility, cardiovascular issues, and ocular abnormalities. Understanding Marfan syndrome is crucial for early diagnosis and management to mitigate potential health complications.
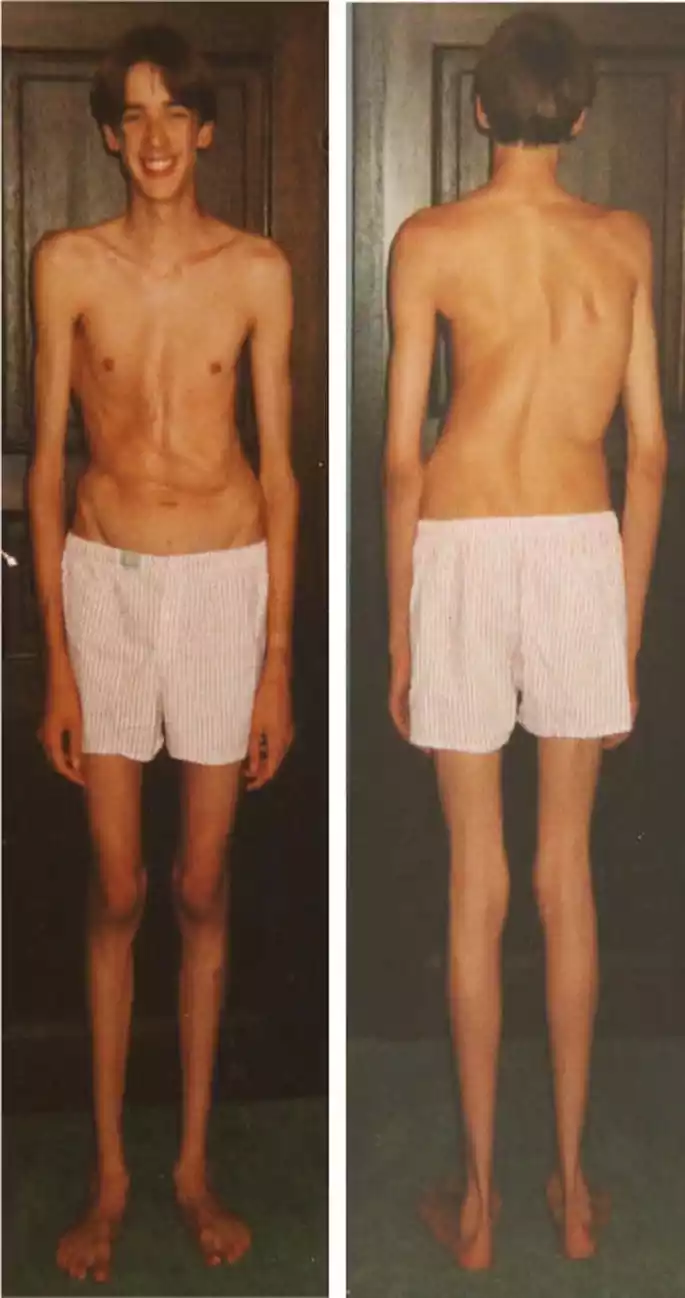
Marfanoid Habitus: Marfanoid habitus refers to a physical appearance and body structure that resembles the characteristics seen in Marfan syndrome, such as tall stature, long fingers, and a slim build. It differs from Marfan syndrome as it is not linked to FBN1 gene mutations. Marfanoid habitus can result from various genetic or environmental factors and may not necessarily lead to the same medical complications associated with Marfan syndrome. Distinguishing between the two is essential for appropriate medical evaluation and care.
What is Marfan Syndrome?
Marfan syndrome is a rare genetic disorder that primarily affects the connective tissues of the body. Connective tissues are essential for providing strength and support to various organs and structures, including the skeleton, blood vessels, and the eyes. This condition is caused by mutations in the FBN1 gene, which encodes a protein called fibrillin-1. Individuals with Marfan syndrome may exhibit a wide range of physical and medical features, which can vary in severity.
Some common characteristics and symptoms of Marfan syndrome include:
- Skeletal Abnormalities: People with Marfan syndrome often have long limbs, particularly the arms and legs. They may also have joint hypermobility, scoliosis (curvature of the spine), and a narrow, tall body frame.
- Cardiovascular Issues: Marfan syndrome can pose significant threats to both heart and blood vessel health. This may lead to aortic aneurysms (weakened and enlarged aorta) and valve problems, which can be life-threatening if not monitored and managed.
- Ocular Manifestations: Eye problems associated with Marfan syndrome include nearsightedness (myopia), lens dislocation, and an increased risk of retinal detachment.
- Other Features: Individuals with Marfan syndrome may have a high, arched palate, a sunken or protruding chest (pectus excavatum or pectus carinatum), and dental abnormalities.
- Potential Complications: Left untreated or unmonitored, Marfan syndrome can lead to serious health complications, particularly those related to the cardiovascular system. Regular medical follow-up and management are crucial to reduce these risks.
Marfan syndrome varies in its presentation and severity among affected individuals. Early diagnosis and appropriate medical care, which may include medications and surgical interventions, can help improve the quality of life and prognosis for individuals with this condition. Genetic counseling is also an important component of managing Marfan syndrome, as it can help families understand the inheritance pattern and make informed decisions about family planning.
What is Marfanoid Habitus?
Marfanoid habitus refers to a physical appearance and body structure that resembles the characteristics seen in Marfan syndrome without being caused by the specific genetic mutations associated with Marfan syndrome. While individuals with Marfan syndrome have a genetic mutation primarily in the FBN1 gene, leading to abnormalities in connective tissues, those with a Marfanoid habitus typically exhibit similar physical features but lack the underlying genetic cause.

Some of the common physical characteristics associated with Marfanoid habitus include:
- Tall Stature: People with a Marfanoid habitus tend to be taller than average for their age and gender.
- Long Limbs: They may have elongated arms and legs, which can result in a slender and lanky appearance.
- Arachnodactyly: This refers to long, slender fingers and toes.
- Narrow Body Frame: Individuals with Marfanoid habitus may have a slim body build and a relatively narrow chest.
- Joint Hypermobility: Like those with Marfan syndrome, they may exhibit joint hypermobility, which means their joints can move beyond the normal range of motion.
Marfanoid habitus can result from various factors other than the FBN1 gene mutation seen in Marfan syndrome. These factors can include variations in other genes or even just natural variation in body proportions. While Marfanoid habitus may share some physical characteristics with Marfan syndrome, it does not necessarily lead to the same medical complications and health risks associated with the genetic disorder. Proper medical evaluation and assessment are essential to distinguish between Marfanoid habitus and Marfan syndrome.
Comparison Table of Marfan Syndrome and Marfanoid Habitus
Here is a comparison table outlining the key differences between Marfan Syndrome and Marfanoid Habitus:
| Characteristic | Marfan Syndrome | Marfanoid Habitus |
|---|---|---|
| Etiology | Genetic disorder caused by mutations in the FBN1 gene | Physical appearance resembling Marfan syndrome but not caused by FBN1 gene mutations or any specific genetic alteration |
| Genetic Inheritance | Typically inherited in an autosomal dominant manner | Does not follow a specific inheritance pattern and is often due to natural variation or other genetic factors |
| Connective Tissue Abnormalities | Present, leading to structural issues in multiple organ systems | May have normal connective tissues with no inherent structural problems |
| Physical Features | Long limbs, joint hypermobility, skeletal deformities, cardiovascular issues, and ocular abnormalities | Tall stature, long limbs, slender build, arachnodactyly (long fingers/toes), joint hypermobility, but typically without the associated medical complications |
| Medical Complications | Cardiovascular complications (aortic aneurysms, valve problems), ocular issues, skeletal abnormalities | Generally lacks the severe medical complications seen in Marfan syndrome |
| Diagnostic Criteria | Based on clinical evaluation, genetic testing for FBN1 mutations | Diagnosis relies on clinical assessment of physical features but without specific genetic markers |
| Management and Treatment | Requires specialized medical management, including medications and surgical interventions | Typically does not require specific medical treatment unless underlying conditions are present |
| Prognosis | Prognosis varies depending on the severity of complications and timely medical intervention | Generally has a favorable prognosis as it lacks the serious health risks associated with Marfan syndrome |
Marfanoid habitus is primarily a physical appearance and body structure, whereas Marfan syndrome is a genetic disorder with a range of associated medical complications. Distinguishing between the two is essential for appropriate medical care and genetic counseling.
How to diagnosis of Marfan Syndrome and Marfanoid Habitus
Diagnosing Marfan Syndrome and Marfanoid Habitus involves a combination of clinical evaluation, medical history assessment, and, in the case of Marfan Syndrome, genetic testing. Here are the steps for diagnosing each condition:
Diagnosis of Marfan Syndrome
- Clinical Evaluation: The diagnosis of Marfan Syndrome typically begins with a thorough clinical assessment by a healthcare professional, such as a geneticist, cardiologist, or other specialists. The evaluation includes:
- Physical examination to assess characteristic features like tall stature, long limbs, joint hypermobility, chest deformities (pectus excavatum or pectus carinatum), and eye abnormalities.
- Cardiovascular assessment, which may involve imaging studies like echocardiography or MRI to detect aortic root dilation and valvular problems.
- Ocular examination to look for lens dislocation, myopia, and other eye-related issues.
- Skeletal evaluation for features such as scoliosis or abnormal bone development.
- Ghent Criteria: Clinicians use the Ghent criteria, a set of diagnostic criteria, to determine if an individual meets the clinical and genetic criteria for Marfan Syndrome. The criteria take into account various signs and symptoms, family history, and genetic testing results.
- Genetic Testing: Genetic testing may be recommended to identify mutations in the FBN1 gene or other genes associated with Marfan Syndrome. While not all individuals with Marfan Syndrome have an identifiable mutation, genetic testing can be helpful in confirming the diagnosis in some cases.
Diagnosis of Marfanoid Habitus
Diagnosing Marfanoid Habitus is primarily a clinical assessment because it is not linked to specific genetic mutations. Here’s how it’s typically done:
- Clinical Evaluation: A healthcare professional will perform a comprehensive physical examination to assess the patient’s physical features. The focus will be on:
- Tall stature
- Long limbs
- Arachnodactyly (long, slender fingers and toes)
- Joint hypermobility
- Medical History: A detailed medical history is essential to rule out any underlying medical conditions that might cause these physical features. Family history of similar physical traits or genetic conditions should also be considered.
- Differential Diagnosis: The healthcare provider will consider other conditions that might present with similar physical features, such as Marfan Syndrome, homocystinuria, and other connective tissue disorders.
- Imaging and Testing: In some cases, imaging studies or additional tests may be ordered to assess the cardiovascular system, skeletal structure, or other potential issues. These tests are typically performed when there are specific concerns or symptoms beyond the physical appearance.
- Genetic Testing (if warranted): If there are concerns about an underlying genetic cause, genetic testing may be considered to rule out or identify other genetic syndromes or disorders.
Marfanoid Habitus is a descriptive term for a certain body type and appearance, and it may not always be associated with an underlying medical condition. Proper diagnosis relies on a comprehensive evaluation by a healthcare professional to determine if there are any specific medical concerns or genetic factors contributing to the physical characteristics.
Treatment Options for Marfan Syndrome and Marfanoid Habitus
Treatment options for Marfan Syndrome and Marfanoid Habitus differ significantly due to the distinct nature of these conditions. Marfan Syndrome is a genetic disorder with potential medical complications, while Marfanoid Habitus primarily refers to a physical appearance without the same associated health risks.
Here are the treatment options for each:
Treatment Options for Marfan Syndrome
- Medical Management: Individuals with Marfan Syndrome require ongoing medical management to address potential complications. This may include the following:
- Medications: Beta-blockers or other medications may be prescribed to reduce the risk of aortic dissection and manage blood pressure.
- Regular Monitoring: Routine check-ups with specialists (cardiologists, ophthalmologists, orthopedic surgeons, etc.) to monitor cardiovascular health, eye health, and skeletal issues.
- Orthopedic Interventions: Orthopedic surgery may be needed to address scoliosis or chest deformities.
- Ocular Care: Treatment for eye-related issues, such as prescription eyeglasses or surgery to correct lens dislocation or retinal detachment.
- Dental Care: Management of dental issues, including a high, arched palate.
- Lifestyle Modifications: Lifestyle changes can help reduce the risk of complications:
- Regular Exercise: Engaging in low-impact exercises can help maintain cardiovascular health.
- Avoiding High-Impact Activities: Activities that put stress on the aorta, such as heavy lifting or contact sports, should be avoided.
- Aortic Root Surgery: Surgical intervention may be necessary for individuals with aortic dilation or aneurysms.
- Genetic Counseling: Genetic counseling is essential for individuals with Marfan Syndrome and their families to understand the genetic inheritance pattern and make informed decisions about family planning.
Treatment Options for Marfanoid Habitus
Marfanoid Habitus does not require specific medical treatment unless there are underlying health issues or concerns. Treatment primarily focuses on addressing any related medical conditions or symptoms.
Here are some considerations:
- Medical Evaluation: If an individual with Marfanoid Habitus experiences symptoms or has concerns about underlying health conditions, they should seek a medical evaluation.
- Addressing Underlying Conditions: If any associated health issues are identified during evaluation (e.g., cardiovascular problems, joint pain), appropriate treatments or interventions will be recommended based on the specific diagnosis.
- Regular Health Check-Ups: Routine health check-ups and screenings can help detect and address any potential health concerns early, even if they are not directly related to Marfanoid Habitus.
It’s important to emphasize that Marfanoid Habitus is primarily a physical appearance and body structure, and it does not inherently lead to the same medical complications seen in Marfan Syndrome. Therefore, treatment for Marfanoid Habitus is tailored to the individual’s specific health needs and concerns, if present. In contrast, Marfan Syndrome requires ongoing medical management to prevent or mitigate the associated health risks.
Similarities between Marfan Syndrome and Marfanoid Habitus
Marfan Syndrome and Marfanoid Habitus share certain physical similarities, which can sometimes make it challenging to differentiate between the two without a thorough medical evaluation. Here are the key similarities:
- Tall Stature: Both individuals with Marfan Syndrome and those with Marfanoid Habitus tend to be taller than average for their age and gender.
- Long Limbs: In both cases, individuals often have elongated arms and legs, contributing to a slender and lanky appearance.
- Arachnodactyly: Both groups may exhibit arachnodactyly, characterized by long, slender fingers and toes.
- Joint Hypermobility: Both conditions can involve joint hypermobility, where the joints can move beyond the normal range of motion.
These physical similarities can lead to confusion, but it’s essential to recognize that Marfanoid Habitus is primarily a descriptive term for a specific body type and appearance, while Marfan Syndrome is a distinct genetic disorder with associated medical complications affecting various organ systems, including the cardiovascular, skeletal, and ocular systems. Proper medical evaluation and assessment are necessary to differentiate between the two and determine if any underlying genetic conditions or health risks are present.
Conclusion
Marfan Syndrome is a rare genetic disorder caused by mutations in the FBN1 gene, leading to a range of medical complications primarily affecting the cardiovascular, skeletal, and ocular systems. Accurate diagnosis and lifelong medical management are crucial to mitigate risks and improve quality of life. On the other hand, Marfanoid Habitus refers to a physical appearance resembling Marfan Syndrome but not caused by the same genetic mutations.
It typically lacks the associated medical complications, with treatment focused on addressing any underlying health concerns, if present. Distinguishing between the two is essential for appropriate medical care and genetic counseling.



