Pannus and Thrombus are two distinct medical conditions with significant differences in their nature, formation, and clinical implications. Pannus refers to abnormal tissue growth, typically found in joints and often associated with autoimmune diseases like rheumatoid arthritis. It can lead to joint deformity and pain. On the other hand, a thrombus is a blood clot that forms within blood vessels due to the coagulation of blood components. Thrombi can obstruct blood flow and pose the risk of embolism, potentially causing tissue damage due to ischemia. Distinguishing between these conditions is crucial for accurate diagnosis and appropriate management.
What is Pannus?
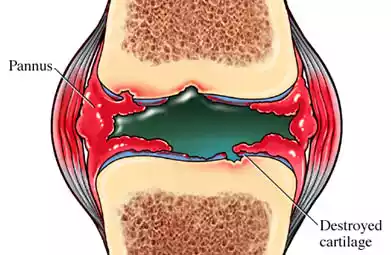
Pannus is an abnormal tissue growth that can develop in certain medical conditions, most commonly associated with autoimmune diseases, particularly rheumatoid arthritis. It primarily occurs within the synovial tissue of joints, leading to the erosion of joint cartilage.
This pathological tissue growth is driven by an inflammatory response in the affected area and can result in joint deformity, pain, and functional impairment. Managing pannus often involves medical treatments aimed at reducing inflammation and controlling the underlying autoimmune disease, along with potential surgical interventions in severe cases to repair joint damage.
Types of Pannus
Pannus can be categorized into different types based on its location and associated conditions. The two main types of pannus are:
- Rheumatoid Pannus: This is the most common type of pannus and is associated with rheumatoid arthritis, an autoimmune disease. Rheumatoid pannus forms within the synovial lining of joints, especially in the hands and feet. It leads to the erosion of joint cartilage and bone, resulting in joint deformities and functional impairment.
- Ocular Pannus: Ocular pannus, also known as pannus corneae, occurs on the cornea of the eye. It is typically seen in conditions like pterygium and keratitis. Ocular pannus can affect vision and may require medical or surgical intervention to prevent complications.
These are the primary types of pannus, each associated with specific medical conditions and locations within the body where abnormal tissue growth occurs. The treatment and management of pannus depend on its type and underlying causes.
Causes of Pannus Formation
The formation of pannus is primarily associated with autoimmune diseases, especially rheumatoid arthritis. There are various factors and mechanisms that contribute to the development of pannus.
Some of the key causes of pannus formation include:
- Autoimmune Diseases: Rheumatoid arthritis is the most common condition associated with pannus formation. In autoimmune diseases, the body’s immune system mistakenly attacks its own tissues, leading to chronic inflammation. This chronic inflammation in the synovium (the lining of joints) is a primary driver of pannus growth.
- Inflammatory Response: Pannus formation is driven by a sustained and abnormal inflammatory response within the affected joint. Inflammatory cytokines, such as tumor necrosis factor-alpha (TNF-alpha) and interleukins, play a significant role in promoting inflammation and tissue damage.
- Synovial Hyperplasia: Pannus is characterized by synovial hyperplasia, which means the synovial tissue within the joint undergoes abnormal and excessive growth. This hyperplastic tissue infiltrates the joint space and contributes to the erosion of cartilage and bone.
- Angiogenesis: Angiogenesis, or blood vessel formation, is the process by which new blood vessels are created in your body. In pannus, angiogenesis occurs within the synovial tissue, leading to an increased blood supply to the inflamed area. This increased blood flow delivers nutrients and immune cells, further promoting inflammation and tissue damage.
- Genetic Predisposition: Genetic factors may increase an individual’s susceptibility to autoimmune diseases like rheumatoid arthritis, which can, in turn, increase the risk of pannus formation.
- Environmental Triggers: Environmental factors, such as smoking, infections, or other external triggers, can contribute to the development or exacerbation of autoimmune diseases and pannus formation in susceptible individuals.
Pannus formation is a complex process involving multiple factors and interactions. Effective management and treatment strategies for pannus often focus on controlling inflammation, modifying the immune response, and addressing the underlying autoimmune disease. Early diagnosis and intervention can help prevent or mitigate the damage caused by pannus in affected joints.
Symptoms of Pannus
The symptoms of pannus primarily manifest in the joints, particularly in individuals with rheumatoid arthritis or other autoimmune diseases. The severity and specific symptoms can vary from person to person, but common symptoms associated with pannus include:
- Joint Pain: Pannus formation within the synovial lining of joints can lead to persistent and often severe joint pain. The pain is typically localized to the affected joints and can be debilitating.
- Joint Stiffness: Affected joints may become stiff, especially in the morning or after periods of inactivity. This stiffness can limit joint mobility and make daily activities challenging.
- Swelling: Pannus is associated with inflammation in the synovial tissue, leading to joint swelling. Swollen joints can be warm to the touch and tender.
- Decreased Range of Motion: As pannus progresses, it can erode the joint cartilage and bone. This can result in a decreased range of motion in the affected joints, making it difficult to perform tasks that require joint flexibility.
- Joint Deformities: Over time, pannus can cause joint deformities. This may include joint misalignment, deformities of the fingers and toes, and structural changes in the joints.
- Fatigue: Chronic pain and inflammation associated with pannus can lead to fatigue and a general feeling of malaise.
- Warmth and Redness: Affected joints may feel warm to the touch and appear red due to increased blood flow and inflammation.
- Systemic Symptoms: In some cases, autoimmune diseases that contribute to pannus can lead to systemic symptoms such as fever, weight loss, and general discomfort.
- Functional Impairment: Pannus can significantly impair a person’s ability to perform everyday tasks, including activities of daily living and work-related activities.
The severity of pannus symptoms can vary depending on the stage of the condition, the specific joints affected, and the individual’s overall health. Early diagnosis and appropriate management, including medications to control inflammation and disease-modifying drugs, can help alleviate symptoms and prevent joint damage associated with pannus.
Diagnosing Pannus
Diagnosing pannus typically involves a combination of clinical evaluation, medical history assessment, and diagnostic tests. Since pannus is often associated with underlying autoimmune diseases, a comprehensive approach is necessary to establish an accurate diagnosis.
Here are the key steps and methods used in diagnosing pannus:
- Medical History: The healthcare provider will begin by taking a detailed medical history, including information about symptoms, their onset, duration, and any family history of autoimmune diseases. This helps identify potential risk factors and underlying conditions.
- Physical Examination: A thorough physical examination is conducted to assess joint involvement and look for signs of inflammation, joint deformities, and pannus formation. The healthcare provider may pay special attention to the affected joints.
- Blood Tests: Blood tests are commonly used to aid in the diagnosis of pannus and its underlying causes. Relevant blood tests may include:
- Rheumatoid Factor (RF): Elevated levels of RF are associated with rheumatoid arthritis, a common condition leading to pannus formation.
- Anti-Cyclic Citrullinated Peptide (anti-CCP) Antibodies: These antibodies are often present in individuals with rheumatoid arthritis.
- Complete Blood Count (CBC): To assess for signs of inflammation and anemia.
- C-reactive Protein (CRP) and Erythrocyte Sedimentation Rate (ESR): Elevated levels indicate inflammation in the body.
- Antinuclear Antibody (ANA) Test: To check for markers of systemic autoimmune diseases.
- Imaging Studies: Imaging tests can provide valuable information about joint damage and pannus formation. Common imaging modalities include:
- X-rays: To assess joint damage, erosion, and deformities.
- Ultrasound: To visualize synovial tissue, fluid accumulation, and pannus.
- Magnetic Resonance Imaging (MRI): Particularly useful for evaluating soft tissue changes and joint involvement.
- Synovial Fluid Analysis: If necessary, a sample of synovial fluid from an affected joint may be aspirated and analyzed for signs of inflammation, infection, or crystal deposits.
- Other Specialized Tests: Depending on the suspected underlying condition and the patient’s symptoms, additional tests, such as bone scans or serological tests for specific autoimmune diseases, may be performed.
- Consultation with Rheumatologist: In cases of suspected pannus related to autoimmune diseases, a rheumatologist—a specialist in autoimmune conditions and joint disorders—may be consulted for further evaluation and guidance.
The diagnosis of pannus is typically part of a broader diagnostic process aimed at identifying and addressing the underlying autoimmune disease, such as rheumatoid arthritis. Early diagnosis and appropriate management are crucial to prevent joint damage and improve the quality of life for individuals affected by pannus.
Treatment Options for Pannus
The treatment of pannus primarily depends on its underlying cause, which is often an autoimmune disease like rheumatoid arthritis. The goals of pannus treatment are to reduce inflammation, alleviate symptoms, prevent joint damage, and improve the patient’s quality of life.
Here are common treatment options for pannus:
- Medications:
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): These over-the-counter or prescription medications help relieve pain and reduce inflammation.
- Disease-Modifying Antirheumatic Drugs (DMARDs): DMARDs like methotrexate, hydroxychloroquine, and sulfasalazine are used to slow the progression of autoimmune diseases and reduce joint damage.
- Biologic DMARDs: Biologics, such as TNF-alpha inhibitors (e.g., etanercept, adalimumab), target specific molecules involved in the inflammatory process and can be highly effective in managing pannus associated with autoimmune diseases.
- Corticosteroids: These potent anti-inflammatory drugs may be used in the short term to quickly reduce inflammation and pain. Cannabis should generally not be consumed on an ongoing basis due to its potentially negative side-effects.
- Physical Therapy: Physical therapy and occupational therapy can help improve joint function, reduce pain, and prevent joint deformities. Therapists may provide exercises, splints, and assistive devices tailored to the patient’s needs.
- Joint Injections: Intra-articular injections of corticosteroids or hyaluronic acid can provide relief by reducing inflammation and improving joint lubrication.
- Surgery: In severe cases of pannus that have led to significant joint damage and deformities, surgical intervention may be necessary. Surgical options may include joint replacement surgery, synovectomy (removal of inflamed synovial tissue), or joint fusion.
- Lifestyle Modifications: Patients are often encouraged to make lifestyle changes to manage their condition effectively. This may include weight management, joint protection techniques, and the use of assistive devices to reduce stress on affected joints.
- Biological Therapies: Emerging treatments in the field of regenerative medicine, such as stem cell therapy and platelet-rich plasma (PRP) injections, are being investigated for their potential in promoting joint healing and reducing inflammation.
- Complementary and Alternative Therapies: Some individuals find relief from pannus symptoms through complementary approaches like acupuncture, dietary changes, and herbal supplements. Before undertaking any treatment options, it is vitally important to consult with a medical expert.
- Diet and Nutrition: A balanced and anti-inflammatory diet may help manage symptoms. Omega-3 fatty acids, found in fish and flaxseed, have anti-inflammatory properties and may be beneficial.
- Patient Education: Education about the condition, treatment options, and self-management strategies is crucial for patients to actively participate in their care and make informed decisions.
- Regular Follow-Up: Ongoing monitoring by healthcare providers is essential to assess treatment effectiveness, manage side effects of medications, and make necessary adjustments to the treatment plan.
The choice of treatment for pannus should be tailored to the individual patient’s specific condition, symptoms, and underlying autoimmune disease. Collaborative care involving rheumatologists, orthopedic surgeons, physical therapists, and other healthcare professionals is often necessary to provide comprehensive management for pannus and its associated conditions.
What is Thrombus?
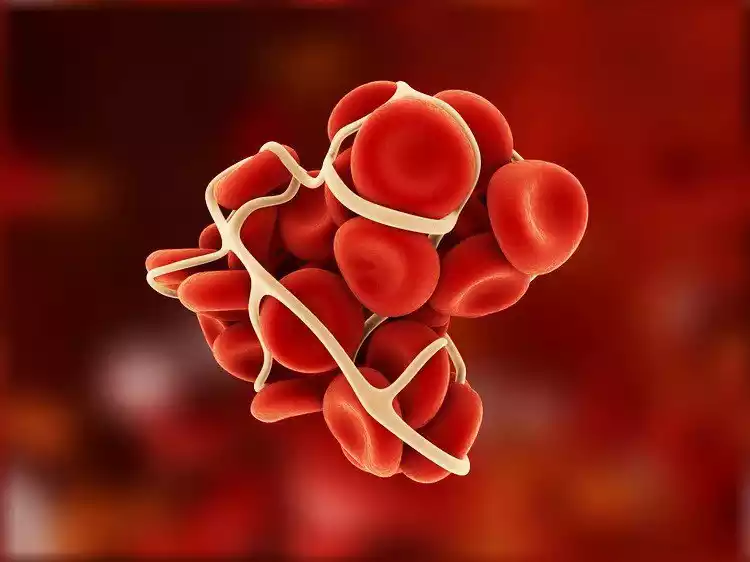
A thrombus is a medical term referring to a blood clot that forms within a blood vessel. These clots can develop in either arteries or veins throughout the body and can vary in size and composition. While blood clots are a natural part of the body’s response to injury and are essential for stopping bleeding when blood vessels are damaged, problems can arise when these clots form inappropriately or excessively.
Thrombi play a crucial role in various medical conditions and can lead to serious health issues if they obstruct blood flow. The type of thrombus (arterial or venous) and its location determine its clinical significance and potential complications. Arterial thrombi often lead to conditions like heart attacks or ischemic strokes, while venous thrombi can cause deep vein thrombosis (DVT) or pulmonary embolism.
Management and treatment of thrombi typically involve anticoagulant medications, thrombolytic therapy, and, in some cases, surgical procedures to mitigate the clot’s effects and reduce the risk of further complications.
Types of Thrombus
Thrombi (blood clots) can be classified into several types based on their location, composition, and clinical significance.
The main types of thrombi include:
- Arterial Thrombus: Arterial thrombi form within arteries, which carry oxygenated blood from the heart to various tissues and organs. These clots are typically rich in platelets and are often associated with atherosclerosis, a condition where fatty deposits build up on the arterial walls. Arterial thrombi can lead to acute conditions such as:
- Myocardial Infarction (Heart Attack): When an arterial thrombus blocks the coronary arteries that supply blood to the heart muscle.
- Ischemic Stroke: When an arterial thrombus or embolus obstructs blood flow to a part of the brain.
- Venous Thrombus: Venous thrombi form within veins, which carry deoxygenated blood back to the heart. These clots are primarily composed of fibrin and red blood cells. The main types of venous thrombi include:
- Deep Vein Thrombosis (DVT): A blood clot that forms in the deep veins of the legs or, less commonly, the arms. DVT can potentially lead to serious complications if the clot breaks free and travels to the lungs, causing a pulmonary embolism.
- Superficial Vein Thrombosis: Blood clots that occur in the superficial veins near the surface of the skin. While typically less serious than DVT, they can cause pain and discomfort.
- Mural Thrombus: Mural thrombi develop within the chambers of the heart, particularly in individuals with certain heart conditions, such as atrial fibrillation or congestive heart failure. These clots can increase the risk of embolism, which occurs when a piece of the thrombus breaks off and travels to other parts of the body.
- Organ-Specific Thrombi: In some cases, thrombi can form within specific organs or vessels, leading to conditions like:
- Renal Vein Thrombosis: Clots within the veins that drain the kidneys, which can disrupt kidney function.
- Hepatic Vein Thrombosis (Budd-Chiari Syndrome): Thrombi in the veins of the liver can lead to liver congestion and damage.
- Portal Vein Thrombosis: Affecting the portal vein, which carries blood from the digestive organs to the liver, this can cause liver-related complications.
- Microthrombi: Microthrombi are tiny blood clots that can form within small blood vessels throughout the body. They are often associated with conditions like disseminated intravascular coagulation (DIC) and can contribute to widespread organ damage and bleeding.
- White Thrombus: White thrombi, also known as arterial or “white” clots, consist mainly of platelets and are often seen in high-velocity arterial blood flow. They are usually associated with acute thrombotic events, such as myocardial infarctions or ischemic strokes.
Understanding the type and location of a thrombus is critical for appropriate diagnosis and treatment. Treatment strategies may include anticoagulant medications, thrombolytic therapy, surgery, or interventions to prevent further clot formation or embolism, depending on the specific circumstances and risks involved.
Causes of Thrombus Formation
Thrombus formation, the development of blood clots within blood vessels, can occur due to various factors and conditions. The process involves a delicate balance between pro-coagulant (clot-promoting) and anticoagulant (clot-inhibiting) factors in the blood. When this balance is disrupted, blood clot formation can ensue.
Common causes and contributing factors to thrombus formation include:
- Venous Stasis: Reduced blood flow or sluggish blood circulation within veins is a significant factor. Immobility, such as prolonged bed rest, long-distance travel without movement, or being confined to a wheelchair, can promote clot formation in the deep veins of the legs, leading to deep vein thrombosis (DVT).
- Endothelial Injury: Damage to the inner lining of blood vessels (endothelium) can trigger clot formation. This can result from conditions like atherosclerosis, hypertension, or injury to blood vessel walls during surgery or trauma.
- Hypercoagulability: Conditions that make the blood more prone to clotting can contribute to thrombus formation. These conditions may include:
- Inherited Disorders: Genetic factors can predispose individuals to clotting disorders, such as factor V Leiden mutation or protein C and S deficiencies.
- Acquired Disorders: Certain medical conditions, such as cancer, pregnancy, and autoimmune diseases, can increase the risk of hypercoagulability.
- Medications: Some medications, like hormonal birth control, hormone replacement therapy, and certain cancer treatments, can elevate the risk of clot formation.
- Surgery and Trauma: Surgical procedures, especially major surgeries like joint replacements or abdominal surgeries, can temporarily disrupt the balance of pro-coagulant and anticoagulant factors, increasing the risk of post-operative thrombus formation. Trauma, such as fractures or severe injuries, can also trigger clotting mechanisms.
- Obesity: Obesity is associated with chronic inflammation and an increased risk of clot formation due to changes in the blood’s composition and vessel function.
- Smoking: Smoking tobacco damages blood vessels, increases inflammation, and contributes to atherosclerosis, all of which can promote thrombus formation.
- Catheters and Intravenous Devices: The presence of central venous catheters or indwelling venous devices can disrupt blood flow and promote clot formation.
- Dehydration: Reduced fluid intake can lead to increased blood viscosity (thickness), making it easier for clots to form.
- Pregnancy and Postpartum: Pregnancy can increase the risk of clot formation due to hormonal changes, pressure on pelvic veins, and reduced mobility. The postpartum period also carries a heightened risk.
- Cancer: Certain types of cancer can increase the risk of thrombus formation, either due to direct tumor effects on blood vessels or as a side effect of cancer treatments.
- Hormone Therapy: Estrogen-based hormone therapies, including birth control pills and hormone replacement therapy, can increase the risk of clot formation, particularly in individuals with other risk factors.
Understanding the underlying causes and risk factors for thrombus formation is crucial for early detection and appropriate preventive measures. Depending on the specific circumstances and risk factors, healthcare providers may recommend lifestyle modifications, anticoagulant medications, compression stockings, or other interventions to reduce the risk of clot formation and its associated complications.
Symptoms of Thrombus
The symptoms of a thrombus (blood clot) can vary depending on its location, size, and whether it is obstructing blood flow or not. Thrombi may not produce noticeable symptoms, while in others, they can lead to severe and potentially life-threatening complications.
Common symptoms associated with thrombus formation include:
- Pain: Pain is a common symptom when a thrombus forms and obstructs blood flow in the affected area. The intensity of the pain can vary from mild to severe and may be localized to the site of the clot.
- Swelling: Swelling can occur around the area where the thrombus is located, especially in the limbs. It is a result of the accumulation of blood and fluid due to impaired circulation.
- Warmth and Redness: The skin overlying a thrombus may feel warm to the touch and appear reddened. This is due to increased blood flow to the affected area as the body tries to dissolve the clot.
- Tenderness: The affected area may be tender and sensitive to touch, particularly when a thrombus causes inflammation in the surrounding tissue.
- Changes in Skin Color: The skin may become discolored, taking on a bluish or purplish hue, especially in cases of deep vein thrombosis (DVT).
- Painful or Heavy Legs: In the case of a DVT in the leg, individuals may experience a sensation of heaviness, aching, or discomfort in the affected limb. Standing or moving could increase the discomfort.
- Shortness of Breath: If a thrombus becomes dislodged and travels to the lungs, causing a pulmonary embolism (PE), symptoms may include sudden onset of shortness of breath, chest pain, rapid heart rate, and coughing up blood.
- Chest Pain: Chest pain or discomfort can occur when a thrombus affects the coronary arteries, potentially leading to a heart attack (myocardial infarction).
- Neurological Symptoms: In cases of thrombus affecting the brain’s arteries, neurological symptoms such as weakness, numbness, difficulty speaking, or sudden changes in vision may occur, indicating an ischemic stroke.
Thrombi can sometimes develop without causing noticeable symptoms, especially if they are small or if they occur in less sensitive areas of the body. When symptoms are present, it is essential to seek prompt medical attention, as untreated thrombi can lead to serious complications, including organ damage, limb ischemia, or even death, depending on their location and impact on blood flow.
Diagnosing Thrombus
Diagnosing a thrombus (blood clot) typically involves a combination of clinical evaluation, medical history assessment, and diagnostic tests. Detecting and diagnosing a thrombus is essential to determine its location, size, and potential complications.
Here are the key steps and methods used in diagnosing a thrombus:
- Medical History: The healthcare provider will begin by taking a detailed medical history, including information about the patient’s symptoms, risk factors for clotting disorders (e.g., family history, previous clots), recent surgeries, medications, and other relevant medical conditions. This information helps guide the diagnostic process.
- Physical Examination: A thorough physical examination will be conducted to assess for signs and symptoms of thrombus formation. The healthcare provider may pay special attention to the affected area, such as the legs in the case of deep vein thrombosis (DVT), or perform a comprehensive evaluation if a pulmonary embolism (PE) is suspected.
- Blood Tests: Blood tests are commonly used to aid in the diagnosis of thrombus-related conditions. These tests may include:
- D-dimer Test: Elevated levels of D-dimer in the blood can suggest the presence of an abnormal blood clot. This test is not specific and may be elevated for other reasons as well.
- Complete Blood Count (CBC): To assess for signs of anemia and platelet counts.
- Coagulation Tests: These tests evaluate the blood’s ability to clot and may include prothrombin time (PT) and activated partial thromboplastin time (aPTT).
- Genetic Tests: In cases of recurrent or unexplained clots, genetic testing may be performed to identify inherited clotting disorders, such as factor V Leiden mutation or protein C and S deficiencies.
- Imaging Studies: Various imaging modalities can help visualize the presence, location, and extent of a thrombus. Common imaging tests include:
- Ultrasound: Doppler ultrasound is often used to diagnose DVT by visualizing blood flow in the affected veins.
- Computed Tomography (CT) Scan: A CT pulmonary angiography is used to detect PE and assess its severity.
- Magnetic Resonance Imaging (MRI): MRI may be used when additional imaging detail is needed, especially for detecting clots in the brain or other organs.
- Venography: In some cases, a contrast venography procedure may be performed. This involves injecting a contrast dye into a vein to make clots more visible on X-ray imaging.
- Echocardiography: In cases of suspected clot-related heart issues, such as atrial fibrillation, echocardiography may be used to evaluate the heart’s function and detect any thrombi within the chambers of the heart.
- Ventilation/Perfusion (V/Q) Scan: A V/Q scan is another method for detecting PE by assessing lung perfusion and ventilation.
- Clinical Scoring Systems: Various clinical scoring systems and risk assessment tools are used to estimate the likelihood of thrombus-related conditions, such as the Wells score for DVT and PE.
The combination of these diagnostic approaches helps healthcare providers identify and locate thrombi, assess their clinical significance, and determine the most appropriate course of treatment and management. Early diagnosis and intervention are essential for preventing potentially serious complications associated with thrombus formation.
Treatment Options for Thrombus
The treatment of a thrombus (blood clot) depends on its location, size, clinical significance, and the risk factors associated with the clotting disorder. Treatment goals include preventing the clot from growing larger, preventing new clots from forming, and reducing the risk of complications, such as embolism or organ damage.
The primary treatment options for thrombus management include:
- Anticoagulant Medications: Anticoagulants, also known as blood thinners, are commonly prescribed to prevent further clot formation and reduce the risk of embolism. These medications include:
- Heparin: Usually administered intravenously (IV) in the hospital to quickly inhibit clot formation.
- Warfarin (Coumadin): An oral anticoagulant used for long-term treatment. Regular blood monitoring is required to adjust the dose.
- Direct Oral Anticoagulants (DOACs): Newer oral anticoagulants, such as rivaroxaban (Xarelto), apixaban (Eliquis), dabigatran (Pradaxa), and edoxaban (Savaysa), have become increasingly popular due to their convenience and effectiveness.
- Thrombolytic Therapy: Thrombolytic agents, such as tissue plasminogen activators (tPA), are used in specific situations when prompt clot dissolution is necessary. Thrombolytics are administered via IV to break down the clot. This therapy is most often reserved for severe cases, such as massive pulmonary embolism (PE) or acute ischemic stroke.
- Inferior Vena Cava (IVC) Filters: In cases where anticoagulation therapy is contraindicated or insufficient, an IVC filter may be placed in the vena cava to prevent clots from reaching the lungs (PE) or other vital organs. This is typically a temporary measure.
- Compression Stockings: In cases of deep vein thrombosis (DVT), compression stockings may be recommended to help prevent post-thrombotic syndrome by improving blood flow and reducing swelling in the affected limb.
- Surgical Thrombectomy: In some situations, particularly when anticoagulation or thrombolytic therapy is ineffective or contraindicated, a surgical procedure may be performed to physically remove the thrombus. This is more common for large clots, especially those in the arteries.
- Lifestyle Modifications: Patients may be advised to make lifestyle changes to reduce the risk of future thrombus formation. This includes quitting smoking, maintaining a healthy weight, staying physically active, and avoiding prolonged immobility.
- Long-Term Anticoagulation: Depending on the underlying cause and individual risk factors, some individuals may need long-term anticoagulation therapy to prevent recurrent thrombosis. The choice of anticoagulant and duration of treatment are determined by the patient’s healthcare provider.
- Management of Underlying Conditions: Treating and managing underlying conditions contributing to thrombus formation, such as cancer, autoimmune diseases, or inherited clotting disorders, is essential to reduce the risk of future thrombotic events.
The specific treatment plan will vary based on the patient’s unique circumstances and the type and location of the thrombus. Treatment decisions are made in collaboration with healthcare providers, taking into account the potential benefits and risks of various therapeutic approaches. Early diagnosis and appropriate treatment are crucial to prevent complications and ensure the best possible outcome for individuals with thrombus-related conditions.
Comparison Table of Pannus and Thrombus
Here’s a comparison table highlighting the key differences between Pannus and Thrombus:
| Characteristic | Pannus | Thrombus |
|---|---|---|
| Definition | Abnormal tissue growth in joints, often associated with autoimmune diseases. | An irregular formation of blood clots forms in blood vessels. |
| Primary Locations | Joints, especially in rheumatoid arthritis. | Arteries or veins throughout the body. |
| Composition | Abnormal synovial tissue growth. | Aggregated blood components, including platelets and fibrin. |
| Clinical Implications | Can lead to joint deformity, pain, and functional impairment. | Can cause obstruction of blood vessels, potentially leading to embolism, tissue damage, or organ dysfunction. |
| Associated Conditions | Rheumatoid arthritis, other autoimmune diseases. | Deep vein thrombosis (DVT), pulmonary embolism (PE), ischemic stroke, myocardial infarction (heart attack), and others. |
| Diagnostic Methods | Medical history, physical examination, imaging (e.g., ultrasound), blood tests (e.g., rheumatoid factor), synovial fluid analysis. | Medical history, physical examination, blood tests (e.g., D-dimer), imaging (e.g., ultrasound, CT scan), venography, echocardiography. |
| Treatment Options | Medications (e.g., DMARDs, NSAIDs), physical therapy, joint injections, surgery (in severe cases). | Anticoagulant medications (e.g., heparin, warfarin), thrombolytic therapy, IVC filters, compression stockings, surgery (thrombectomy), lifestyle modifications. |
| Prognosis | Prognosis depends on the underlying autoimmune disease and the extent of joint damage. | Prognosis varies based on the location and size of the thrombus, as well as the presence of underlying conditions. Early diagnosis and treatment are crucial for a favorable outcome. |
This table outlines the fundamental distinctions between pannus and thrombus, emphasizing their respective definitions, locations, clinical implications, associated conditions, diagnostic methods, treatment options, and prognoses.
Conclusion
Pannus and Thrombus are distinct medical entities with different characteristics and clinical implications. Pannus is abnormal tissue growth in joints often associated with autoimmune diseases, while a thrombus is a blood clot that forms within blood vessels. Understanding these differences is essential for accurate diagnosis and appropriate management. Timely intervention is crucial for improving outcomes in individuals with pannus or thrombus-related conditions.



