Periosteal and Parosteal Osteosarcoma are two distinct subtypes of osteosarcoma, a rare and aggressive form of bone cancer. These subtypes differ in their origin, location within the bone, clinical presentation, pathological characteristics, and treatment approaches. Accurate differentiation between periosteal and parosteal osteosarcoma is crucial for determining the most effective treatment strategies and predicting patient outcomes. We will delve into the key differences between these two subtypes to enhance our understanding of their unique characteristics and management.
Periosteal Osteosarcoma
Periosteal osteosarcoma is a specific subtype of osteosarcoma, a rare and aggressive form of bone cancer. It originates in the periosteum, which is the tough membrane that covers the outer surface of bones. Unlike other types of osteosarcoma that develop within the bone itself (intramedullary), periosteal osteosarcoma arises from the outer layer of the bone. This subtype is characterized by the formation of a tumor or mass on the bone’s surface, often associated with pain, swelling, and restricted movement of the affected limb.
Diagnosis typically involves imaging studies, such as X-rays, MRI, and CT scans, followed by a biopsy to confirm the presence of cancerous cells. Treatment typically includes surgical removal of the tumor, along with adjuvant therapies like chemotherapy to reduce the risk of recurrence. Prognosis varies based on factors such as the stage of the cancer at diagnosis and the success of treatment.
Symptoms of Periosteal Osteosarcoma
Periosteal osteosarcoma is a rare form of bone cancer that develops in the periosteum, the tough membrane covering the outer surface of bones. The symptoms of periosteal osteosarcoma can vary depending on the location and size of the tumor, but common signs and symptoms may include:
- Pain: Persistent and localized pain in the affected bone or joint is one of the most common symptoms. The pain may worsen with activity or at night.
- Swelling: Swelling or a noticeable lump at the site of the tumor can occur. This swelling is often firm and adheres to the bone’s surface.
- Limited Range of Motion: Depending on the tumor’s location, there may be a restriction in the range of motion of the adjacent joint or limb.
- Weakness: Muscle weakness or atrophy in the affected area can develop over time.
- Fractures: Because periosteal osteosarcomas often occur on the bone’s surface, they can weaken the bone, making it more prone to fractures or breaks.
- Tenderness: Surrounding areas of a tumor could be sensitive when touched directly.
- Warmth and Redness: In some cases, there may be localized warmth and redness over the tumor site.
- Fatigue: Generalized fatigue or malaise can occur as the cancer progresses.
These symptoms can mimic other less serious conditions or injuries. Therefore, if you or someone you know is experiencing persistent bone pain, swelling, or any of the mentioned symptoms, it’s crucial to consult a healthcare professional for a proper evaluation, diagnosis, and appropriate management. Early diagnosis and treatment can improve outcomes for individuals with periosteal osteosarcoma.
Parosteal Osteosarcoma

Parosteal osteosarcoma is a specific subtype of osteosarcoma, a rare and malignant bone cancer. It originates from the periosteum, which is the connective tissue covering the outer surface of bones. Unlike other forms of osteosarcoma that develop within the bone itself, parosteal osteosarcoma arises from the outer layer of the bone, typically in areas where tendons or ligaments attach.
It is characterized by the slow growth of a well-defined tumor on the bone’s surface. While it is generally considered to have a lower-grade malignancy compared to other osteosarcoma subtypes, it still requires medical attention and treatment to prevent potential growth and spread.
Symptoms of Parosteal Osteosarcoma
Parosteal osteosarcoma is a rare subtype of bone cancer that primarily originates from the outer layer of bones, specifically in areas where tendons or ligaments attach. The symptoms of parosteal osteosarcoma can vary depending on the tumor’s size and location, but common signs and symptoms may include:
- Painless Mass or Lump: The most characteristic symptom of parosteal osteosarcoma is the presence of a painless, slow-growing mass or lump on the surface of a bone. This mass is often firm and adheres closely to the bone.
- Limited Range of Motion: Depending on the tumor’s location, it may restrict the range of motion of the adjacent joint or limb.
- Bone Deformity: In some cases, the tumor’s growth can cause bone deformity in the affected area.
- Weakness: Muscle weakness or atrophy in the vicinity of the tumor can occur over time.
- Tenderness: The area around the tumor may become tender to the touch, although this is less common than with some other forms of bone cancer.
- Fractures: Parosteal osteosarcoma can weaken the bone, making it more susceptible to fractures or breaks, though this is relatively rare.
- Numbness or Tingling: In cases where the tumor compresses nerves, numbness or tingling sensations in the affected area may be present.
Parosteal osteosarcoma is often less aggressive and tends to grow slowly compared to other osteosarcoma subtypes. Timely diagnosis and appropriate treatment are still crucial to prevent the tumor from advancing and causing complications. If you or someone you know has a painless lump or experiences any of these symptoms, consulting a healthcare professional for a proper evaluation and diagnosis is essential for effective management and potential treatment options.
Diagnosis of Periosteal Osteosarcoma and Parosteal Osteosarcoma
Diagnosing both periosteal osteosarcoma and parosteal osteosarcoma, two distinct subtypes of bone cancer, involves a combination of clinical evaluation, imaging studies, and confirmatory tests.
Here’s an overview of the diagnostic process for each of these subtypes:
Diagnosis of Periosteal Osteosarcoma:
- Clinical Evaluation: The diagnostic process often begins with a thorough clinical evaluation by a healthcare professional. This includes taking a detailed medical history and conducting a physical examination. Patients may present with localized pain, swelling, or a palpable mass near the affected bone.
- Imaging Studies:
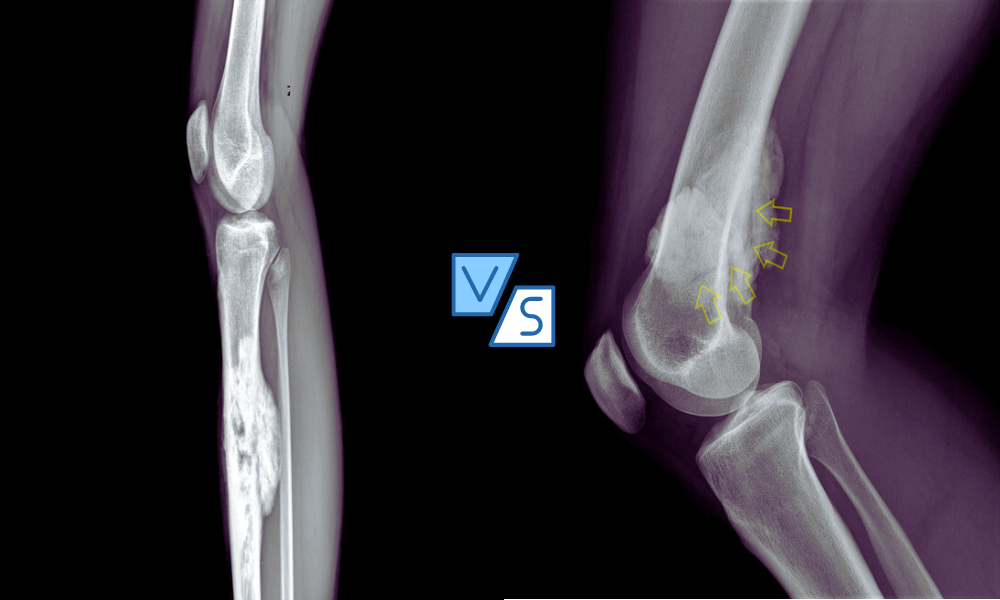
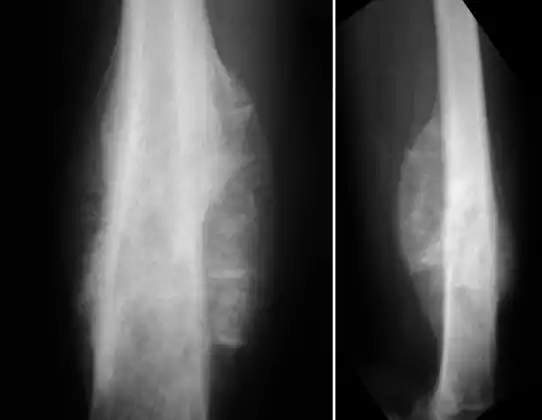
- X-rays: X-ray imaging is usually the initial step in assessing bone abnormalities. Periosteal osteosarcoma may appear as an irregular mass or bone elevation near the bone’s surface.
- Computed Tomography (CT) Scan: CT scans provide detailed cross-sectional images of the bone, helping to assess the tumor’s extent and characteristics.
- Magnetic Resonance Imaging (MRI): MRI scans are crucial for evaluating soft tissues and the tumor’s relationship with nearby structures, which can be particularly important for periosteal osteosarcoma diagnosis.
- Biopsy: When imaging studies suggest the presence of a tumor, a biopsy is typically performed to confirm the diagnosis. During a biopsy, a small sample of tissue is collected from the suspected tumor site. A pathologist then examines the tissue under a microscope to determine if it contains cancerous cells.
- Histological Examination: The pathologist examines the biopsy specimen’s histological characteristics to confirm the diagnosis of periosteal osteosarcoma. Specific features of this type of osteosarcoma may be observed under the microscope.
- Immunohistochemistry and Molecular Testing: In some cases, immunohistochemistry and molecular testing may be conducted to further characterize the tumor and identify specific markers that can guide treatment decisions.
- Staging: Once the diagnosis of periosteal osteosarcoma is confirmed, the extent of the disease is evaluated through staging. Staging helps determine if the cancer has spread to other parts of the body, such as the lungs or other bones, and guides treatment planning.
Diagnosis of Parosteal Osteosarcoma:
The diagnostic process for parosteal osteosarcoma is quite similar to that of periosteal osteosarcoma due to their shared origin in the bone’s outer layer:
- Clinical Evaluation: Healthcare professionals conduct a comprehensive clinical evaluation, taking a detailed medical history and performing a physical examination. Symptoms may include painless masses or lumps, limited range of motion, and bone deformity.
- Imaging Studies:
- X-rays: X-rays are often the initial imaging modality used to detect bone abnormalities. Parosteal osteosarcoma may appear as a well-defined, bony mass on the surface of the affected bone.
- CT Scan: CT scans provide detailed images that help assess the tumor’s characteristics and relationship with the bone.
- Biopsy: To confirm the diagnosis, a biopsy is performed. This involves collecting a small tissue sample from the suspected tumor site, which is then examined by a pathologist under a microscope.
- Histological Examination: The pathologist examines the biopsy specimen’s histological features to confirm the presence of parosteal osteosarcoma.
- Immunohistochemistry and Molecular Testing: In some cases, additional testing may be conducted to further characterize the tumor and identify specific markers.
- Staging: Staging helps determine the extent of the disease and whether it has metastasized to other parts of the body, guiding treatment planning.
Both periosteal and parosteal osteosarcoma require a multidisciplinary approach involving orthopedic surgeons, radiologists, pathologists, and oncologists for accurate diagnosis and effective treatment planning. Early diagnosis and appropriate treatment are crucial for optimizing outcomes in these rare bone cancer subtypes.
Treatment Approach for Periosteal Osteosarcoma and Parosteal Osteosarcoma
The treatment approach for periosteal osteosarcoma and parosteal osteosarcoma, two distinct subtypes of bone cancer, typically involves a combination of surgical resection and, in some cases, adjuvant therapies. The specific treatment plan may vary depending on the tumor’s size, location, stage, and individual patient factors.
Here is an overview of the treatment approach for each of these subtypes:
Treatment Approach for Periosteal Osteosarcoma:
- Surgical Resection: The primary treatment for periosteal osteosarcoma is surgical removal (resection) of the tumor. The goal is to achieve complete resection while preserving as much healthy bone and adjacent tissues as possible. Limb-salvage surgery is often pursued when feasible, meaning the affected bone and nearby tissues are preserved, and reconstructive procedures may be necessary.
- Chemotherapy: Adjuvant chemotherapy is commonly recommended after surgery to reduce the risk of local recurrence and distant metastasis. Multi-agent chemotherapy regimens are typically employed and are based on the specific characteristics of the tumor. Common chemotherapy drugs include doxorubicin, cisplatin, methotrexate, and ifosfamide.
- Radiation Therapy: Radiation therapy is generally not the primary treatment for periosteal osteosarcoma, but it may be considered in cases where complete surgical resection is not possible or in cases of recurrence.
- Follow-Up: After treatment, regular follow-up appointments are essential to monitor for any signs of recurrence and to assess the patient’s overall health and function.
Treatment Approach for Parosteal Osteosarcoma:
- Surgical Resection: The mainstay of treatment for parosteal osteosarcoma is surgical removal of the tumor. Given the relatively low-grade nature of parosteal osteosarcoma, efforts are made to preserve as much of the surrounding bone and tissues as possible. Surgeons aim for complete tumor removal with clear margins.
- Radiation Therapy: In some cases, radiation therapy may be considered as an adjuvant treatment, particularly if there are concerns about microscopic residual disease or if complete surgical resection is challenging due to the tumor’s location.
- Chemotherapy: Unlike other forms of osteosarcoma, parosteal osteosarcoma is often less responsive to chemotherapy. Therefore, chemotherapy is typically not a first-line treatment for parosteal osteosarcoma. It may be considered in specific cases, particularly if there are concerns about the risk of recurrence or metastasis.
- Follow-Up: Regular follow-up appointments are necessary to monitor for any signs of recurrence and to assess the patient’s overall health and function.
It’s important to emphasize that the treatment approach for each patient should be individualized, and decisions should be made in consultation with a multidisciplinary team of healthcare professionals, including orthopedic surgeons, medical oncologists, and radiation oncologists.
The choice of treatment depends on factors such as the tumor’s characteristics, stage, and the patient’s overall health and preferences. Early diagnosis and timely intervention are crucial for achieving the best possible outcomes in both periosteal and parosteal osteosarcoma.
Comparison Table of Periosteal and Parosteal Osteosarcoma
Here is a comparison table highlighting the key differences between periosteal and parosteal osteosarcoma:
| Characteristic | Periosteal Osteosarcoma | Parosteal Osteosarcoma |
|---|---|---|
| Origin | Develops in the periosteum (outer bone membrane) | Develops on the bone’s surface, often near tendons or ligaments |
| Tumor Characteristics | Typically forms a well-defined mass on the bone’s surface | Usually presents as a painless, slow-growing lump adhering to the bone |
| Pain and Symptoms | Often associated with localized pain, swelling, and discomfort | Typically painless but may cause limited range of motion or muscle weakness |
| Aggressiveness | Considered more aggressive compared to parosteal osteosarcoma | Generally less aggressive, tends to grow slowly |
| Response to Chemotherapy | Usually responsive to chemotherapy, which is often used as adjuvant therapy | Less responsive to chemotherapy; chemotherapy is not typically the first-line treatment |
| Surgical Resection | Surgery to remove the tumor while preserving bone structure is common | Surgical resection with efforts to preserve adjacent tissues and bone is the primary treatment |
| Radiation Therapy | Not the primary treatment, but may be considered in some cases | Considered as adjuvant therapy in specific cases, particularly if complete surgical resection is challenging |
| Metastasis | Has the potential to metastasize (spread) to other parts of the body | Rarely metastasizes, but local recurrence can occur |
| Prognosis | Prognosis varies depending on tumor stage and response to treatment | Generally more favorable prognosis compared to periosteal osteosarcoma |
This table highlights the primary differences between periosteal and parosteal osteosarcoma, individual cases can vary, and treatment decisions should be made in consultation with a medical team based on the patient’s specific condition and characteristics of the tumor.
Similarities- Periosteal and Parosteal Osteosarcoma
Here are the similarities between periosteal and parosteal osteosarcoma:
- Both are rare subtypes of osteosarcoma.
- They primarily originate in the bone and are associated with the outer surface of bones.
- Commonly occur in long bones, such as the femur and tibia.
- Surgical resection is the primary treatment approach for both, aiming to remove the tumor while preserving healthy bone and tissue.
- Adjuvant therapies like chemotherapy and radiation may be considered in some cases to reduce the risk of recurrence.
- Diagnosis involves histological examination of biopsy specimens to confirm cancerous cells.
Summary
Periosteal and Parosteal Osteosarcoma, though rare and sharing some commonalities in their location and treatment approaches, are distinct subtypes of bone cancer. Understanding their differences is crucial for accurate diagnosis and tailored treatment planning, as periosteal osteosarcoma tends to be more aggressive and responsive to chemotherapy, while parosteal osteosarcoma is generally less aggressive and less responsive to chemotherapy. Timely diagnosis and a multidisciplinary medical approach remain essential for optimizing outcomes for patients with these unique bone cancers.