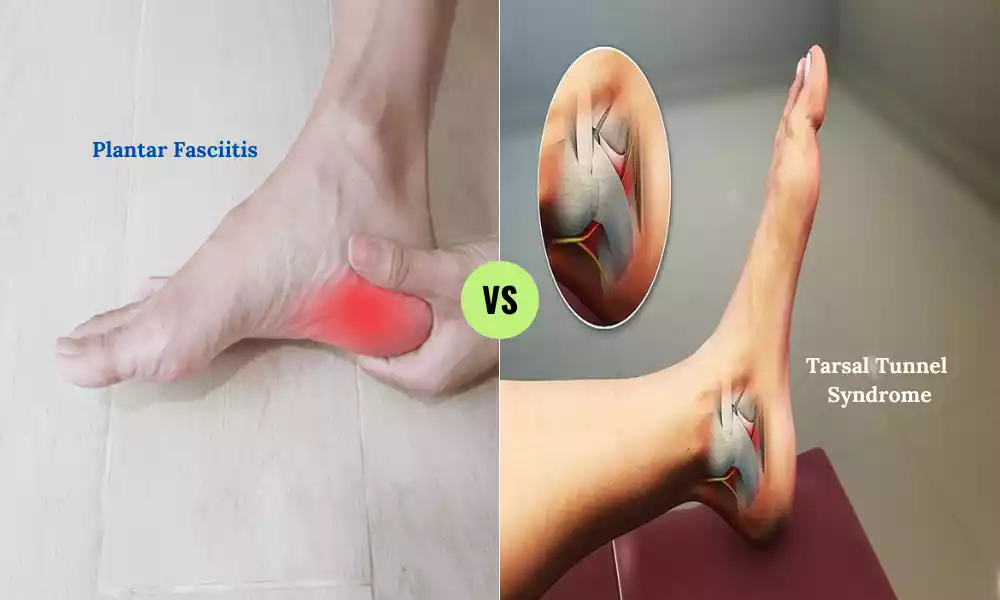
Plantar Fasciitis and Tarsal Tunnel Syndrome are both common foot conditions that can cause discomfort and affect daily activities. Plantar Fasciitis involves inflammation of the tissue connecting the heel to the toes, resulting in heel pain.
Tarsal Tunnel Syndrome is characterized by the compression of the tibial nerve along the inner ankle, leading to tingling and burning sensations. Proper understanding and management of these conditions are essential for alleviating symptoms and maintaining foot health.
What is Plantar Fasciitis?

Plantar Fasciitis is a prevalent foot condition characterized by inflammation and irritation of the plantar fascia, a thick band of tissue running along the underside of the foot from the heel to the toes. This condition commonly leads to sharp, stabbing pain in the heel, particularly during the first steps after periods of rest. Plantar Fasciitis often arises from overuse, repetitive activities, or strain on the foot’s arch-supporting structure.
Tight calf muscles, improper footwear, and certain foot anatomies can also contribute to its development. While rest, ice, stretching, and supportive footwear can aid in recovery, consulting a medical professional for accurate diagnosis and personalized treatment is essential for managing Plantar Fasciitis effectively.
Causes of Plantar Fasciitis
Plantar Fasciitis is primarily caused by the strain and irritation of the plantar fascia, the thick band of tissue that runs along the bottom of the foot. The specific causes and contributing factors to the development of Plantar Fasciitis include:
- Overuse and Repetitive Stress: Engaging in activities that involve repetitive impact on the feet, such as running, jogging, or jumping, can lead to microtears and inflammation in the plantar fascia over time.
- Poor Foot Mechanics: Having abnormal foot mechanics, such as flat feet (overpronation) or high arches (underpronation), can place uneven stress on the plantar fascia, increasing the risk of irritation.
- Obesity: Excess body weight can put additional strain on the feet, causing the plantar fascia to bear more pressure and leading to its inflammation.
- Improper Footwear: Shoes without adequate cushioning or arch support may lead to Plantar Fasciitis. Shoes with inadequate support fail to absorb shock and distribute pressure effectively.
- Tight Calf Muscles and Achilles Tendons: Reduced flexibility in the calf muscles and Achilles tendons can increase tension on the plantar fascia, making it more susceptible to inflammation.
- Sudden Increase in Physical Activity: Rapidly intensifying physical activities, especially those involving the feet, can strain the plantar fascia and cause irritation.
- Age: Plantar Fasciitis is more common in individuals between the ages of 40 and 60, as the plantar fascia may become less flexible and more prone to inflammation with age.
- Occupational Factors: Jobs that require prolonged standing or walking on hard surfaces can contribute to the development of Plantar Fasciitis.
- Muscle Imbalances: Weakness or imbalances in the muscles of the feet and lower legs can alter the way pressure is distributed on the plantar fascia.
- Inadequate Warm-up: Engaging in physical activities without proper warm-up exercises can increase the risk of straining the plantar fascia.
- Underlying Medical Conditions: Certain medical conditions, such as rheumatoid arthritis and ankylosing spondylitis, can increase the likelihood of developing Plantar Fasciitis.
It’s important to note that while these factors can contribute to the development of Plantar Fasciitis, individual cases may vary. If you’re experiencing persistent heel pain or suspect you have Plantar Fasciitis, seeking medical evaluation and guidance from a healthcare professional is recommended for an accurate diagnosis and appropriate treatment plan.
Symptoms of Plantar Fasciitis
Plantar Fasciitis is characterized by specific symptoms, primarily centered around pain and discomfort in the heel and arch of the foot. Common symptoms of Plantar Fasciitis include:
- Heel Pain: The hallmark symptom of Plantar Fasciitis is sharp or stabbing pain in the heel, particularly at the front and bottom of the heel bone. This pain is often most intense in the morning, especially when taking the first steps after waking up.
- Pain After Rest: Pain and discomfort may also occur after periods of rest, such as sitting or lying down for an extended time, and then standing up or resuming activity. This is due to the tightening of the plantar fascia during rest, which leads to increased tension when weight is placed on the foot again.
- Pain During Activity: Activities that involve prolonged standing, walking, running, or jumping can trigger or exacerbate the pain. The pain tends to lessen as the foot “warms up” and the plantar fascia becomes more flexible during movement.
- Stiffness: Some individuals with Plantar Fasciitis may experience stiffness and reduced flexibility in the foot, particularly in the morning or after periods of inactivity.
- Tenderness: The bottom of the heel may feel tender to the touch, and pressure applied to the affected area can elicit pain.
- Radiating Pain: In some cases, the pain from Plantar Fasciitis can radiate along the sole of the foot, extending toward the arch.
- Worsening Pain: If left untreated or if the underlying factors persist, the pain from Plantar Fasciitis can worsen over time and become chronic. It’s important to seek appropriate treatment to prevent long-term discomfort.
It’s worth noting that while the symptoms of Plantar Fasciitis are characteristic, they can sometimes be mistaken for other conditions that cause heel pain. If you’re experiencing persistent foot pain or are unsure about the cause of your symptoms, it’s advisable to consult a healthcare professional for an accurate diagnosis and tailored treatment recommendations. Early intervention and proper management can lead to better outcomes and relief from discomfort.
What is Tarsal Tunnel Syndrome?

Tarsal Tunnel Syndrome is a condition characterized by compression or irritation of the tibial nerve as it passes through the tarsal tunnel, a narrow space located on the inside of the ankle. This tunnel is formed by the bones and soft tissues of the ankle, and it serves as a pathway for several nerves, arteries, and tendons.
Similar to the carpal tunnel in the wrist, the tarsal tunnel can become narrowed or constricted, leading to pressure on the tibial nerve. This compression can result in a range of symptoms, including pain, tingling, numbness, and weakness in the foot and ankle.
The causes of Tarsal Tunnel Syndrome can vary and often include factors that increase pressure on the tibial nerve within the tunnel. These factors may include flat feet, ankle injuries, inflammation of the surrounding tendons, and certain medical conditions like diabetes or arthritis.
The symptoms of Tarsal Tunnel Syndrome can mimic those of other conditions, such as Plantar Fasciitis or nerve entrapment in the lower leg, making accurate diagnosis important. Treatment options for Tarsal Tunnel Syndrome may include rest, immobilization, physical therapy, orthotic devices, anti-inflammatory medications, and in severe cases, surgical decompression to relieve pressure on the tibial nerve and restore normal nerve function.
Causes of Tarsal Tunnel Syndrome
Tarsal Tunnel Syndrome can occur due to the compression or irritation of the tibial nerve as it passes through the tarsal tunnel, a narrow space located on the inside of the ankle. The causes of Tarsal Tunnel Syndrome often involve factors that contribute to increased pressure on the tibial nerve within this tunnel.
Some common causes and contributing factors include:
- Anatomical Factors: Certain anatomical variations can predispose individuals to Tarsal Tunnel Syndrome. These include having a flat foot, which can lead to increased strain on the tibial nerve, or having an enlarged or prominent structure within the tarsal tunnel.
- Injury or Trauma: Ankle injuries such as sprains, fractures, or direct trauma to the inside of the ankle can result in swelling and inflammation, potentially causing compression of the tibial nerve within the tarsal tunnel.
- Overpronation: Individuals with overpronation, where the foot excessively rolls inward during walking or running, may experience increased pressure on the tibial nerve due to the altered biomechanics.
- Repetitive Strain: Engaging in activities that involve repetitive ankle movement, such as running or walking long distances, can contribute to irritation and inflammation of the tendons and structures within the tarsal tunnel, leading to nerve compression.
- Tendon Inflammation: Conditions like tendinitis or tenosynovitis involving the tendons that pass through the tarsal tunnel can lead to swelling and compression of the tibial nerve.
- Systemic Conditions: Certain medical conditions like diabetes, arthritis, and peripheral neuropathy can increase the risk of nerve compression and Tarsal Tunnel Syndrome.
- Space-Occupying Lesions: Growth of benign or malignant masses within or near the tarsal tunnel can exert pressure on the tibial nerve, leading to symptoms.
- Pregnancy: Hormonal changes and weight gain during pregnancy can contribute to fluid retention and swelling, potentially causing nerve compression within the tarsal tunnel.
- Footwear: Ill-fitting shoes or footwear that lacks proper support can affect foot mechanics and contribute to nerve compression.
- Inflammatory Conditions: Inflammatory diseases such as rheumatoid arthritis or lupus can cause swelling and inflammation around the tarsal tunnel, leading to nerve compression.
- Scar Tissue: Scar tissue formation due to previous surgery or trauma can affect the space within the tarsal tunnel, potentially compressing the tibial nerve.
Understanding the underlying causes of Tarsal Tunnel Syndrome is crucial for accurate diagnosis and effective treatment. If you’re experiencing symptoms suggestive of this condition, consulting a healthcare professional for evaluation and appropriate management is recommended.
Symptoms of Tarsal Tunnel Syndrome
Tarsal Tunnel Syndrome is characterized by a range of symptoms that result from the compression or irritation of the tibial nerve within the tarsal tunnel, a confined space on the inside of the ankle.
The symptoms of Tarsal Tunnel Syndrome can vary in severity and presentation, but commonly include:
- Pain: Persistent or intermittent pain along the inside of the ankle or the bottom of the foot is a hallmark symptom. The pain may be sharp, burning, tingling, or shooting in nature.
- Numbness and Tingling: Sensations of numbness, tingling, or a “pins and needles” feeling often radiate along the path of the tibial nerve, which can extend to the sole of the foot and sometimes even to the toes.
- Electric Shock Sensation: Some individuals may experience sudden and intense electric shock-like sensations in the foot or ankle, which can be triggered by movement or pressure on the nerve.
- Weakness: Weakness in the affected foot or ankle muscles may occur, leading to difficulties in activities like walking, climbing stairs, or maintaining balance.
- Pain Aggravation: Symptoms may worsen with activities that involve prolonged standing, walking, or physical exertion. Pain and discomfort might also intensify during the night.
- Symptoms Spread: Over time, if left untreated, the symptoms of Tarsal Tunnel Syndrome may spread or progress to involve a larger portion of the foot or even the calf.
- Symptoms Triggered by Movement: Certain movements, such as flexing the ankle or pressing on the tarsal tunnel area, can trigger or worsen the symptoms.
- Relief with Rest: Similar to other nerve-related conditions, symptoms might temporarily improve with rest or elevation of the affected limb.
- Swelling: Swelling around the tarsal tunnel area might be present due to inflammation caused by nerve compression.
- Changes in Sensation: Changes in the way the skin feels, such as hypersensitivity or decreased sensitivity, can occur in the affected area.
It’s important to note that the symptoms of Tarsal Tunnel Syndrome can overlap with those of other conditions, such as peripheral neuropathy or nerve entrapment in the lower leg. If you suspect you have Tarsal Tunnel Syndrome or are experiencing persistent foot or ankle discomfort, seeking medical evaluation from a healthcare professional is recommended for proper diagnosis and tailored treatment. Early intervention can help alleviate symptoms and prevent potential complications.
Comparative Table of Plantar Fasciitis and Tarsal Tunnel Syndrome
Here’s a comparative table outlining key differences between Plantar Fasciitis and Tarsal Tunnel Syndrome:
| Aspect | Plantar Fasciitis | Tarsal Tunnel Syndrome |
|---|---|---|
| Affected Area | Plantar fascia (heel) | Tibial nerve in tarsal tunnel |
| Main Symptom | Heel pain, especially mornings | Pain, numbness, tingling |
| Pain Pattern | Bottom and front of heel | Along inner ankle/foot |
| Pain Triggers | Initial steps, activity | Movement, pressure on nerve |
| Associated Conditions | Overuse, poor footwear | Foot misalignment, injuries |
| Risk Factors | High-impact activities, obesity | Flat feet, diabetes, injury |
| Diagnostic Tests | Clinical assessment, imaging | Clinical assessment, tests |
| Treatment Approach | Rest, stretching, footwear | Orthotics, exercises, rest |
| Nerve Involvement | No direct nerve involvement | Compression of tibial nerve |
| Location of Symptoms | Primarily in heel | Radiating along ankle/foot |
| Nighttime Symptoms | Pain often reduces | Pain/tingling may worsen |
| Relation to Rest | Pain after rest | Rest may alleviate symptoms |
| Potential for Surgery | Rarely required | Considered in severe cases |
| Prognosis and Recovery | Generally favorable | Varied, depending on cause |
Remember, while this table provides a simplified comparison, individual experiences may vary. Speak to a healthcare professional in order to obtain an accurate diagnosis and personalized treatment suggestions.
Plantar Fasciitis and Tarsal Tunnel Syndrome Are Diagnosed

Diagnosing Plantar Fasciitis and Tarsal Tunnel Syndrome involves a combination of medical history assessment, physical examination, and potentially imaging studies. Here’s how each condition is typically diagnosed:
Diagnosis of Plantar Fasciitis:
- Medical History: Your healthcare provider will ask about your symptoms, when they started, and any factors that may have contributed, such as recent changes in activity or footwear.
- Physical Examination: The provider will perform a physical examination of your foot, checking for tenderness, swelling, and any specific pain points along the plantar fascia.
- Pain Response: The presence of sharp pain in the heel, particularly upon the first steps in the morning or after rest, is a key indicator.
- Range of Motion: Limited ankle dorsiflexion (the ability to point your toes upward) may suggest tight calf muscles, which can contribute to Plantar Fasciitis.
- Palpation: Applying pressure to specific points on the foot can help identify areas of tenderness and pain.
- Gait Analysis: Observing your walking pattern and identifying any abnormalities in foot mechanics can aid in diagnosis.
Diagnosis of Tarsal Tunnel Syndrome:
- Medical History: Your medical history will be evaluated to understand your symptoms, their duration, and any potential contributing factors like recent injuries or medical conditions.
- Physical Examination: The healthcare provider will perform a physical examination to check for areas of tenderness along the tarsal tunnel, assess reflexes, and evaluate muscle strength and sensation.
- Tinel’s Sign: Tapping or pressing on the tarsal tunnel area may elicit tingling or electric shock-like sensations, known as Tinel’s sign, which can be indicative of nerve compression.
- Nerve Testing: Nerve conduction studies and electromyography (EMG) may be conducted to assess the function of the tibial nerve and surrounding nerves.
- Imaging: Imaging tests such as ultrasound or magnetic resonance imaging (MRI) might be ordered to visualize the tarsal tunnel and surrounding structures. These tests can help rule out other potential causes of symptoms.
The diagnosis is often clinical, relying on the combination of medical history, physical examination findings, and sometimes additional tests. It’s important to consult a healthcare professional if you’re experiencing symptoms consistent with either Plantar Fasciitis or Tarsal Tunnel Syndrome. Accurate diagnosis is crucial for appropriate treatment planning and management.
Treatment Options for Plantar Fasciitis
Here are your treatment options to manage Plantar Fasciitis:
- Rest and activity modification.
- Ice therapy to reduce inflammation.
- Gentle stretching exercises for calf muscles and Achilles tendon.
- Arch-supporting orthotic inserts and proper footwear.
- Over-the-counter pain relievers like NSAIDs.
- Physical therapy for exercises and techniques.
- Night splints to prevent tightness.
- Corticosteroid injections for severe cases.
- Extracorporeal Shock Wave Therapy (ESWT) may be appropriate in certain instances.
- Undergoing surgery should only be considered as an alternative approach if other forms of therapy do not suffice.
Consulting a healthcare professional is essential for personalized treatment recommendations and effective management.
Managing Tarsal Tunnel Syndrome
Here’s a concise overview of managing Tarsal Tunnel Syndrome:
- Rest and avoid aggravating activities.
- Use orthotic inserts and supportive footwear.
- Physical therapy for exercises and nerve gliding.
- Consider medications for pain and inflammation.
- Use splints to maintain foot position.
- Manage underlying conditions if present.
- Surgical intervention rarely considered.
Collaborating with a healthcare professional is vital for effective management tailored to your situation.
Prevention and Lifestyle Adjustments
Here are the prevention tips and lifestyle adjustments for both Plantar Fasciitis and Tarsal Tunnel Syndrome:
For Plantar Fasciitis:
- Wear supportive footwear.
- Gradually increase activity intensity.
- Incorporate regular foot stretches.
- Maintain a healthy weight.
- Practice good foot hygiene.
- Consider orthotic inserts.
- Warm up before exercise.
- Listen to your body and address discomfort.
For Tarsal Tunnel Syndrome:
- Choose supportive shoes.
- Maintain proper foot alignment.
- Stretch calf muscles and nerves.
- Manage weight.
- Adopt a healthy lifestyle.
- Focus on ergonomics.
- Avoid high heels.
- Stay active with low-impact exercises.
- Keep feet clean and dry.
- Regularly check foot health.
Following these tips can help reduce the risk of these conditions and promote overall foot health. If symptoms continue, speak to a healthcare provider immediately.
Final Thoughts
Plantar Fasciitis and Tarsal Tunnel Syndrome are two distinct foot conditions that can cause considerable discomfort. Timing of diagnosis and intervention are of critical importance for efficient management. By adopting preventive measures and making lifestyle adjustments, individuals can reduce the risk of developing these conditions and enjoy improved foot health.