Sensory and Cerebellar Ataxia are both neurological conditions that manifest as problems with coordination, balance, and movement. They arise from different sources within the nervous system and require distinct diagnostic approaches and treatments. Sensory ataxia primarily stems from issues with sensory nerve pathways, such as those responsible for proprioception and vibration sense, often due to conditions like neuropathy or vitamin deficiencies. In contrast, cerebellar ataxia arises from dysfunction or damage to the cerebellum, a region in the brain responsible for coordinating motor skills and balance.
Understanding the unique characteristics and treatment strategies for each type of ataxia is crucial for effectively managing these conditions and improving the quality of life for those affected.
Sensory Ataxia
Sensory ataxia is a neurological disorder characterized by a lack of coordination and balance that results from a dysfunction in the sensory pathways of the nervous system, specifically in the perception of proprioception (the sense of the body’s position in space), joint position, and vibration sense.

This type of ataxia typically arises when the sensory nerves responsible for transmitting information about these sensations become impaired or damaged. Proprioception and joint position sense help individuals maintain their body’s position and posture, while vibration sense provides information about the body’s contact with the environment.
Common causes of sensory ataxia include:
- Peripheral Neuropathy: Damage or dysfunction of peripheral nerves, often due to conditions like diabetes, vitamin deficiencies, or toxic exposures.
- Posterior Column Disease: This refers to disorders that affect the posterior columns of the spinal cord, where sensory information such as vibration, proprioception, and fine touch is processed. Conditions like tabes dorsalis, a late manifestation of syphilis, can lead to posterior column degeneration.
- Vitamin Deficiencies: Inadequate intake of certain vitamins, particularly vitamin B12, can lead to sensory neuropathy and subsequent sensory ataxia.
- Chronic Alcoholism: Long-term alcohol abuse can result in neuropathy and sensory ataxia due to the toxic effects of alcohol on nerves.
The primary symptom of sensory ataxia is difficulty in maintaining balance and coordinating movements, especially when the individual’s eyes are closed or when they are in poorly lit environments. This is because sensory input from proprioceptive and vibratory senses is crucial for the brain to accurately interpret the body’s position and make adjustments to maintain balance.
Treatment of sensory ataxia typically involves addressing the underlying cause, such as treating vitamin deficiencies or managing neuropathic conditions. Physical therapy and assistive devices like canes or braces may be recommended to help individuals manage their symptoms and improve their mobility and balance.
Cerebellar Ataxia
Cerebellar ataxia is a neurological disorder characterized by a lack of coordination, unsteady movements, and difficulties with balance and posture due to dysfunction or damage to the cerebellum, a part of the brain responsible for coordinating voluntary muscle movements, maintaining balance, and fine-tuning motor skills.

Common causes of cerebellar ataxia include:
- Degenerative Disorders: These are progressive conditions that lead to the gradual degeneration of the cerebellum. Examples include spinocerebellar ataxias and Friedreich’s ataxia.
- Stroke: A stroke that affects the cerebellum can lead to ataxia.
- Trauma: Head injuries or trauma to the back of the head can damage the cerebellum and result in ataxia.
- Infections: Certain infections, such as viral or bacterial infections, can damage the cerebellum and lead to ataxia.
- Tumors: Tumors in or near the cerebellum can interfere with its function and cause ataxia.
- Autoimmune Disorders: Some autoimmune diseases can target the cerebellum and disrupt its function.
- Toxic Exposure: Exposure to certain toxins, such as alcohol or certain medications, can lead to ataxia.
The hallmark symptoms of cerebellar ataxia include:
- Poor coordination: Difficulty with tasks that require precise movements, such as writing or buttoning a shirt.
- Unsteady gait: Difficulty walking in a straight line and maintaining balance.
- Slurred speech: Difficulty articulating words clearly due to impaired control of the vocal muscles.
- Tremors: Shaking or trembling movements, particularly when attempting fine motor tasks.
- Difficulty with eye movements: Jerky or uncoordinated eye movements, which can affect vision and balance.
The specific symptoms and severity of cerebellar ataxia can vary depending on the underlying cause and the extent of cerebellar damage. Treatment options may include addressing the underlying cause (if possible), physical therapy to improve coordination and balance, and sometimes medications to manage symptoms or slow the progression of degenerative forms of ataxia.
Comparison Table of Sensory and Cerebellar Ataxia
Here’s a comparison table of sensory ataxia and cerebellar ataxia, highlighting key differences between these two types of ataxia:
| Characteristic | Sensory Ataxia | Cerebellar Ataxia |
|---|---|---|
| Location of Dysfunction | Sensory pathways of the nervous system | Cerebellum (part of the brain) |
| Primary Sensory Impairment | Impaired proprioception, joint position sense, and vibration sense | No primary sensory impairment; affects coordination and balance control mediated by the cerebellum |
| Common Causes | Peripheral neuropathy, posterior column disease, vitamin deficiencies, chronic alcoholism | Degenerative disorders (e.g., spinocerebellar ataxias), stroke, trauma, infections, tumors, autoimmune disorders, toxic exposure |
| Coordination and Balance | Difficulty maintaining balance and coordinating movements, especially with eyes closed or in dimly lit environments | Difficulty with coordination, balance, and fine motor control; may also affect speech and eye movements |
| Gait Abnormalities | Unsteady gait with difficulty walking straight and maintaining balance | Unsteady, wide-based gait often described as “drunken” or “wobbly” |
| Speech Impairment | Less likely to affect speech directly | Commonly leads to slurred speech and difficulty articulating words |
| Tremors and Shaking | Typically not associated with tremors or shaking | May exhibit tremors, especially during fine motor tasks |
| Underlying Pathology | Primarily involves sensory nerve damage or dysfunction | Primarily involves dysfunction or damage to the cerebellum |
| Treatment Options | Address underlying cause (e.g., treat neuropathy, manage vitamin deficiencies), physical therapy, assistive devices | Manage underlying cause (if possible), physical therapy, medications for symptom management (e.g., for tremors), and lifestyle adjustments |
These are general characteristics, and individual cases of both sensory and cerebellar ataxia can vary in terms of symptoms and severity depending on the underlying cause and the extent of nerve or brain damage. Proper diagnosis by a healthcare professional is essential to determine the specific type and treatment approach for ataxia in each individual case.
Diagnosis of Sensory and Cerebellar Ataxia
The diagnosis of sensory and cerebellar ataxia involves a comprehensive medical evaluation, including clinical assessments, medical history, neurological examinations, and often a combination of specialized tests.
Here are the key steps and diagnostic methods for each type of ataxia:
Diagnosis of Sensory Ataxia:
- Medical History and Physical Examination:
- The healthcare provider will begin by taking a detailed medical history, including information about symptoms, their onset, and any relevant medical conditions or exposures.
- A physical examination will be conducted to assess balance, coordination, muscle strength, and reflexes.
- Neurological Examination:
- The physician will perform a neurological examination to assess sensory function, including proprioception, joint position sense, and vibration sense. Abnormalities in these sensory functions may indicate sensory ataxia.
- Nerve Conduction Studies and Electromyography (EMG):
- Nerve conduction studies and EMG tests may be performed to evaluate the function of peripheral nerves and muscles. Abnormal results can point to peripheral neuropathy, a common cause of sensory ataxia.
- Blood Tests:
- Blood tests may be conducted to check for underlying causes such as vitamin deficiencies (e.g., vitamin B12 deficiency), metabolic disorders, or autoimmune conditions.
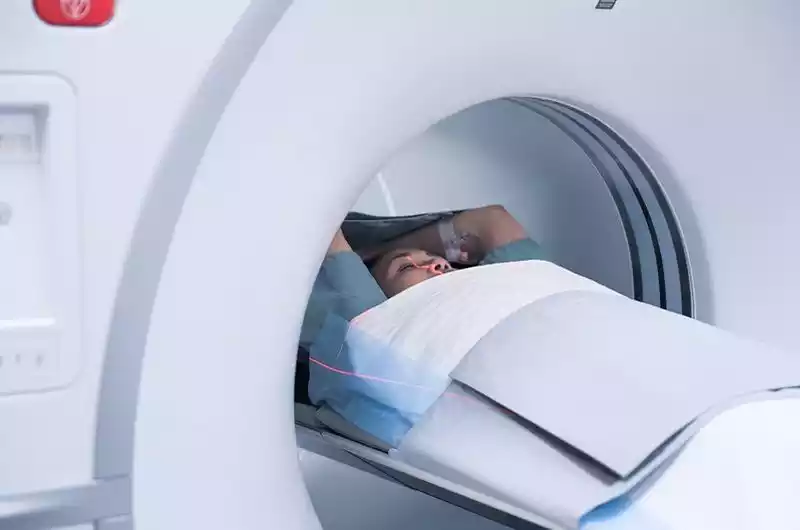
- Imaging Studies:
- In some cases, imaging studies like magnetic resonance imaging (MRI) or computed tomography (CT) scans may be used to rule out structural abnormalities in the spinal cord or brain.
- Cerebrospinal Fluid Analysis:
- Lumbar puncture (spinal tap) and cerebrospinal fluid analysis may be performed if an underlying infection or inflammatory condition is suspected.
Diagnosis of Cerebellar Ataxia:
- Medical History and Physical Examination:
- Similar to sensory ataxia, the healthcare provider will start with a thorough medical history and physical examination to evaluate coordination, balance, muscle tone, and reflexes.
- Neurological Examination:
- A detailed neurological examination will focus on assessing cerebellar function, including tests for limb coordination, gait, and eye movements. Cerebellar ataxia often presents with a wide-based, unsteady gait and difficulties with fine motor control.
- Imaging Studies:
- Brain imaging with MRI or CT scans is a crucial diagnostic tool for cerebellar ataxia. These imaging studies can reveal structural abnormalities or atrophy in the cerebellum, helping to confirm the diagnosis and identify potential causes.
- Genetic Testing:
- Genetic testing may be recommended, especially if there is a suspicion of an inherited form of ataxia, such as spinocerebellar ataxias (SCAs). Genetic tests can identify specific genetic mutations associated with these conditions.
- Blood Tests and Other Tests:
- Similar to sensory ataxia, blood tests may be conducted to assess for underlying metabolic, autoimmune, or infectious causes. Additional tests, such as lumbar puncture, may be performed if necessary.
- Electroencephalogram (EEG):
- In some cases, EEG may be used to evaluate electrical brain activity, especially if seizures are suspected as part of the ataxic presentation.
The diagnosis of both sensory and cerebellar ataxia can be complex, and it often requires collaboration between neurologists and other specialists. Accurate diagnosis is crucial for determining the underlying cause and planning appropriate treatment and management strategies.
Treatment Approaches for Sensory and Cerebellar Ataxia
Treatment approaches for sensory and cerebellar ataxia aim to manage symptoms, improve quality of life, and address any underlying causes. However, it’s important to note that there is no cure for most forms of ataxia, and treatment is often supportive and focused on symptom management. Treatment plans should be tailored to the individual’s specific needs and the underlying cause of ataxia.
Here are the general approaches to treatment:
Treatment for Sensory Ataxia:
- Underlying Cause Management:
- If sensory ataxia is secondary to a specific underlying cause (e.g., vitamin deficiency, neuropathy, or another medical condition), addressing that cause is a primary focus. This may include:
- Vitamin supplementation for deficiencies.
- Management of conditions like diabetes or autoimmune disorders.
- Modification of medications or lifestyle factors contributing to neuropathy.
- If sensory ataxia is secondary to a specific underlying cause (e.g., vitamin deficiency, neuropathy, or another medical condition), addressing that cause is a primary focus. This may include:
- Physical Therapy:
- Physical therapy is often recommended to improve coordination, balance, and mobility.
- Therapists can provide exercises and strategies to help individuals adapt to their impaired sensory input and reduce the risk of falls.
- Assistive Devices:
- Assistive devices like canes, walkers, or orthopedic braces can provide support and stability, helping individuals maintain their independence and safety.
- Occupational Therapy:
- Occupational therapists can help individuals with sensory ataxia adapt to daily tasks and activities by providing techniques and tools to make them more manageable.
Treatment for Cerebellar Ataxia:
- Underlying Cause Management:
- If cerebellar ataxia is caused by an identifiable underlying condition (e.g., stroke, tumor, genetic disorder), addressing the cause is crucial. Treatment may involve surgery, medication, or other specific interventions.
- Physical and Occupational Therapy:
- Physical and occupational therapy can play a significant role in improving balance, coordination, and functional abilities.
- Exercises and strategies can be tailored to the individual’s specific needs and goals.
- Medications:
- Depending on the underlying cause and symptoms, certain medications may be prescribed to manage specific symptoms associated with cerebellar ataxia. For example:
- Medications to reduce tremors or involuntary movements.
- Medications to manage pain or muscle stiffness.
- Medications to address specific genetic or metabolic factors in certain forms of ataxia.
- Depending on the underlying cause and symptoms, certain medications may be prescribed to manage specific symptoms associated with cerebellar ataxia. For example:
- Speech Therapy:
- Speech therapists can work with individuals experiencing speech difficulties, such as slurred speech or voice control problems.
- Adaptive Devices:
- Assistive devices such as orthopedic braces, mobility aids, or communication aids may be recommended to enhance independence and safety.
- Genetic Counseling:
- In cases of genetic ataxias (e.g., spinocerebellar ataxias), genetic counseling can provide information about the condition, inheritance patterns, and family planning.
- Lifestyle Modifications:
- Lifestyle adjustments, including maintaining a healthy diet, staying physically active to the extent possible, and ensuring a safe home environment to prevent falls, can all contribute to better overall well-being.
The treatment plan for ataxia should be individualized and developed in consultation with a neurologist or healthcare team with expertise in managing neurological conditions. Regular follow-up and ongoing care are important to monitor the progression of symptoms and adjust the treatment plan as needed.
Conclusion
Sensory Ataxia and Cerebellar Ataxia are distinct neurological disorders characterized by impaired coordination, balance, and movement. Sensory ataxia primarily results from dysfunction in the sensory pathways of the nervous system, often due to peripheral neuropathy or vitamin deficiencies, and is managed by addressing underlying causes, physical therapy, and assistive devices.
Cerebellar ataxia, on the other hand, stems from damage or dysfunction in the cerebellum, and its management involves treating underlying conditions, physical and occupational therapy, medications, and adaptive devices. While there is no cure for most forms of ataxia, personalized treatment plans can help individuals with these conditions improve their quality of life and functional abilities.



