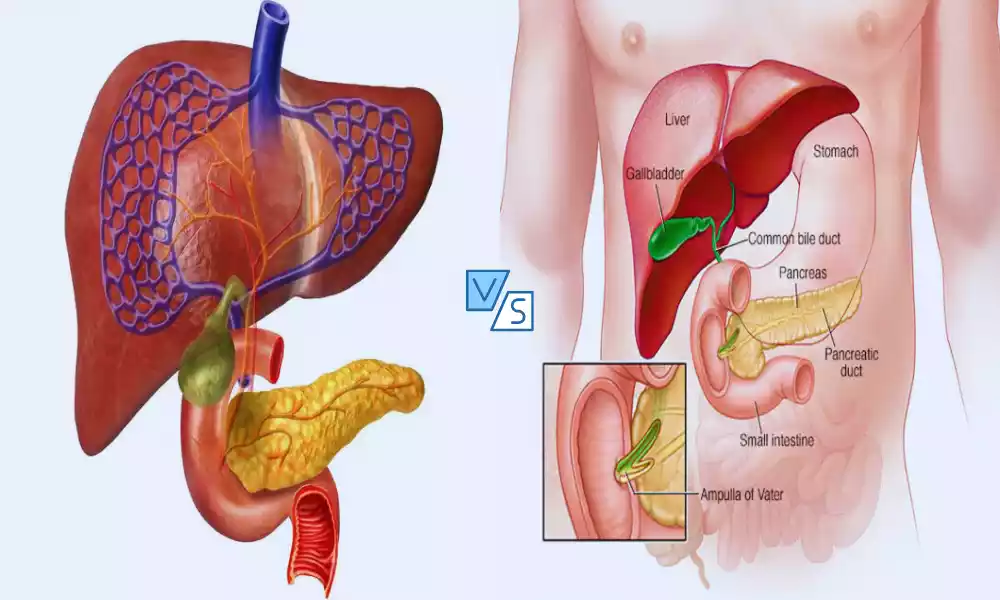
Sphincter of Oddi and Ampulla of Vater are integral components of the digestive system, located near the duodenum, the initial segment of the small intestine. The Sphincter of Oddi is a muscular valve that regulates the flow of bile and pancreatic juices into the duodenum, ensuring optimal digestion.
The Ampulla of Vater is the dilated junction where the common bile duct and pancreatic duct converge, serving as a conduit for these digestive fluids to mix before entering the small intestine. Understanding these structures is crucial for digestive health, as dysfunctions can lead to significant medical issues.
Sphincter of Oddi
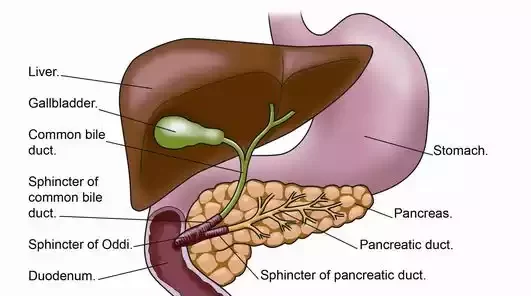
The Sphincter of Oddi is a ring-shaped muscular valve located at the point where the common bile duct and pancreatic duct converge and empty into the duodenum, the first segment of the small intestine. Its primary function is to regulate the flow of bile and pancreatic juices into the duodenum, thereby aiding in the digestive process. The sphincter prevents the backflow of intestinal contents and controls the timing and amount of digestive fluids released, facilitating the digestion of fats and proteins.
The Three Main Parts
The Sphincter of Oddi comprises three main parts, each with its own specific function:
- Sphincter Choledochus: This part surrounds the common bile duct and is responsible for regulating the flow of bile from the liver and gallbladder into the duodenum. When contracted, it prevents bile from flowing into the small intestine, directing it to be stored in the gallbladder instead. When relaxed, it allows bile to flow into the duodenum for digestion.
- Sphincter Pancreaticus: This part surrounds the pancreatic duct and controls the release of pancreatic juices, which contain digestive enzymes like lipase, amylase, and protease. These enzymes are essential for the digestion of fats, carbohydrates, and proteins, respectively. The Sphincter Pancreaticus ensures that these enzymes are released into the duodenum in a controlled manner, promoting efficient digestion.
- Sphincter Ampullae: Also known as the sphincter of the ampulla, this part surrounds the Ampulla of Vater, which is the widened, funnel-like structure where the common bile duct and pancreatic duct meet before emptying into the duodenum. The Sphincter Ampullae coordinates the release of both bile and pancreatic juices into the small intestine through the Ampulla of Vater.
Each of these components works in a coordinated manner to regulate the flow and timing of bile and pancreatic juices entering the duodenum, thereby facilitating optimal digestive function. Dysfunction in any of these parts can result in digestive problems that may require medical intervention.
Function of the Sphincter of Oddi
The primary function of the Sphincter of Oddi is to regulate the flow of bile and pancreatic juices into the duodenum, the first section of the small intestine.
This regulation is essential for several key aspects of digestion and overall gastrointestinal health:
- Timing and Amount: The sphincter controls when and how much bile and pancreatic juices are released into the small intestine. Proper timing is crucial for effective digestion, particularly of fats and proteins.
- Prevention of Backflow: The sphincter acts as a one-way valve, preventing the backflow of intestinal contents into the bile and pancreatic ducts. This is essential to prevent infections and other complications.
- Storage of Bile: When contracted, the Sphincter of Oddi redirects bile back into the gallbladder for storage. This allows the body to have a readily available supply of bile for future meals.
- Enzyme Regulation: By controlling the release of pancreatic juices, which are rich in digestive enzymes like amylase for carbohydrates, lipase for fats, and protease for proteins, the Sphincter of Oddi ensures that these enzymes are available in the right quantities at the right time for optimal digestion.
- Coordination with Other Organs: The Sphincter of Oddi works in conjunction with other digestive organs like the stomach, liver, and pancreas. Hormones such as cholecystokinin and secretin signal the sphincter to relax, allowing the flow of bile and pancreatic juices during the digestive process.
- Protection: By carefully regulating the release of these fluids, the Sphincter of Oddi helps to minimize the risk of damage to the delicate lining of the duodenum from highly concentrated bile or enzymatic juices.
- Alleviation of Spasms: The smooth muscle components of the sphincter can contract or relax to alleviate spasms or obstructions, although dysfunction can lead to problems that might require medical intervention.
The Sphincter of Oddi plays a critical role in the digestive process, regulating the release and flow of essential digestive fluids from the liver, gallbladder, and pancreas into the small intestine. Dysfunction of this important valve can lead to a variety of digestive disorders.
Ampulla of Vater
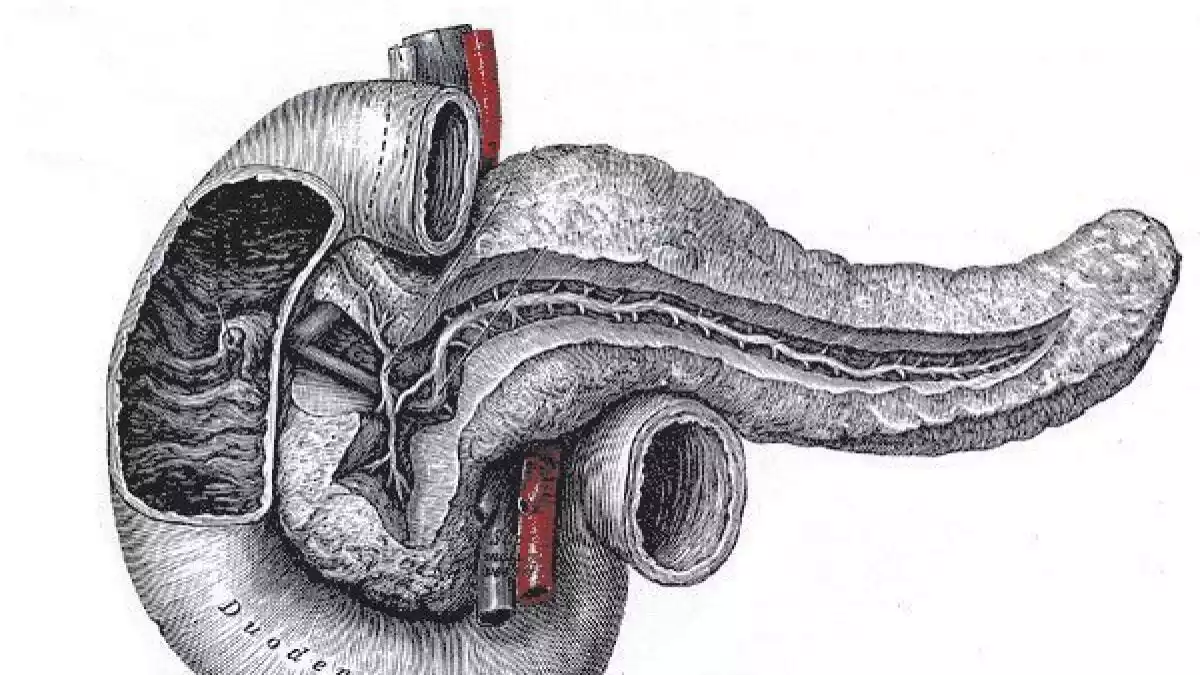
The Ampulla of Vater, also known as the hepatopancreatic ampulla, is a funnel-shaped dilation located in the duodenum, the first segment of the small intestine. It serves as the common meeting point for the common bile duct and the pancreatic duct. The Ampulla of Vater is the site where these two ducts converge and empty their contents—bile from the liver and gallbladder, and pancreatic juices from the pancreas—into the duodenum.
Surrounded by the Sphincter of Oddi, the ampulla acts as a conduit that allows for the mixing of bile and pancreatic juices before they enter the small intestine, thereby facilitating the digestive process.
The Union of Ducts
The union of ducts at the Ampulla of Vater is a critical junction in the digestive system. Here, the common bile duct, which carries bile from the liver and gallbladder, and the pancreatic duct, which carries pancreatic juices from the pancreas, converge into a single opening into the duodenum. This union allows for the coordinated release and mixing of these essential digestive fluids, which play a significant role in breaking down fats, carbohydrates, and proteins in the food we consume.
The Sphincter of Oddi, a muscular valve, surrounds the Ampulla of Vater and controls the flow of these fluids into the duodenum. When the sphincter relaxes, bile and pancreatic juices are released into the small intestine. When it contracts, the flow is halted, and bile is redirected to the gallbladder for storage.
This union of ducts is an essential anatomical feature for optimizing digestive efficiency. The coordinated release of bile and pancreatic juices ensures that digestive enzymes and bile salts are present in the right quantities at the right time for effective digestion. Dysfunction or obstruction at this junction can lead to digestive disorders, pain, and other complications, such as gallstones or pancreatitis, and may require medical intervention.
Importance of the Ampulla of Vater
The Ampulla of Vater plays a crucial role in the digestive system for several reasons:
- Central Hub for Digestive Fluids
The ampulla serves as a central junction where the common bile duct and the pancreatic duct meet. It’s like a crossroads for digestive juices, facilitating the smooth passage of these essential fluids into the duodenum.
- Coordination for Effective Digestion
The union of these two ducts at the Ampulla of Vater allows for the mixing of bile and pancreatic juices, which is essential for effective digestion. Bile emulsifies fats, making them easier to digest, while pancreatic juices contain enzymes that help break down carbohydrates, proteins, and fats.
- Regulation and Timing
The Ampulla of Vater, surrounded by the Sphincter of Oddi, helps regulate the timing and flow of bile and pancreatic juices into the small intestine. This ensures that these fluids are released in optimal quantities at the appropriate times to facilitate digestion.
- Prevention of Backflow
The Sphincter of Oddi, which surrounds the Ampulla of Vater, acts as a one-way valve. This prevents the backflow of intestinal contents, thereby reducing the risk of infections and other complications like pancreatitis or cholangitis.
- Clinical Relevance
A dysfunctional or obstructed Ampulla of Vater can lead to significant health issues. Problems can include blockages that may result in jaundice, infections, or acute conditions like pancreatitis. Thus, understanding the function and anatomy of the Ampulla of Vater is crucial for diagnosing and treating digestive disorders.
- Facilitation of Diagnostic Procedures
The Ampulla of Vater is often a focal point in gastrointestinal diagnostic procedures like endoscopic retrograde cholangiopancreatography (ERCP), used to diagnose and treat conditions affecting the bile and pancreatic ducts.
The Ampulla of Vater is a critical anatomical structure in the digestive system. Its role in coordinating the flow of bile and pancreatic juices into the duodenum makes it indispensable for effective digestion and overall gastrointestinal health.
Comparison Table of Sphincter of Oddi and the Ampulla of Vater
Comparison table can provide a straightforward way to understand the differences and similarities between the Sphincter of Oddi and the Ampulla of Vater:
| Feature | Sphincter of Oddi | Ampulla of Vater |
|---|---|---|
| Anatomical Location | Surrounds the end of the common bile duct and pancreatic duct | Junction where the common bile duct and pancreatic duct merge into the duodenum |
| Function | Controls the flow of bile and pancreatic juice into the duodenum | Serves as the actual opening through which bile and pancreatic juice enter the duodenum |
| Comprised Of | Smooth muscle fibers | Mucous membrane and underlying connective tissue |
| Relation to Ducts | Encircles the ducts | Represents the union of the ducts |
| Disorders | Sphincter of Oddi Dysfunction, biliary obstruction, post-cholecystectomy syndrome | Ampullary cancer, choledocholithiasis, ampullitis |
| Role in Digestion | Regulatory | Conduit |
| Diagnostic Tests | Manometry, ERCP, Ultrasound | ERCP, MRCP, Ultrasound |
| Treatment Options | Endoscopic Sphincterotomy, medication, surgical intervention | Stent placement, stone removal, surgical resection |
| Importance in Digestion | Timing and regulation of digestive juices | Coordinated release and mixing of digestive juices |
I hope this table helps in understanding the roles and features of the Sphincter of Oddi and the Ampulla of Vater, both of which are essential in the digestive process.
Disorders Affecting Sphincter of Oddi and Ampulla of Vater
Disorders affecting the Sphincter of Oddi and the Ampulla of Vater can have significant implications for digestive health. Dysfunction or anatomical abnormalities in these areas can result in a range of clinical symptoms and conditions:
Disorders Affecting the Sphincter of Oddi
- Sphincter of Oddi Dysfunction (SOD): This involves abnormal muscle tone or spasm of the sphincter, leading to impaired flow of bile or pancreatic juice. Symptoms may include abdominal pain, nausea, and vomiting. It is often diagnosed using tests like manometry, ultrasound, or MRCP (Magnetic Resonance Cholangiopancreatography).
- Biliary Obstruction: Sometimes, gallstones can become lodged in the common bile duct near the Sphincter of Oddi, causing obstruction and leading to conditions like cholangitis or jaundice.
- Post-cholecystectomy Syndrome: After gallbladder removal, some people experience ongoing abdominal symptoms due to changes in bile flow, possibly related to the Sphincter of Oddi.
- Pancreatitis: Dysfunction of the Sphincter of Oddi can result in the backflow of digestive juices, leading to inflammation of the pancreas.
Disorders Affecting the Ampulla of Vater
- Ampullary Cancer: A rare form of gastrointestinal cancer that originates in the Ampulla of Vater. Symptoms often include jaundice, abdominal pain, and weight loss.
- Choledocholithiasis: Presence of gallstones in the common bile duct can cause obstruction at the level of the Ampulla of Vater.
- Ampullitis: Inflammation of the Ampulla of Vater, often due to infection, which can cause symptoms like abdominal pain and fever.
- Congenital Anomalies: Some people may be born with anatomical abnormalities affecting the Ampulla of Vater, which may require surgical correction.
- Papillary Stenosis: Narrowing of the ampullary orifice can restrict the flow of bile and pancreatic juices, leading to digestive problems and pain.
Diagnosis and Treatment
Diagnosing and treating disorders affecting the Sphincter of Oddi and the Ampulla of Vater usually involve a multi-disciplinary approach. Healthcare providers such as gastroenterologists, surgeons, and radiologists often collaborate to offer the best care. Below are some common diagnostic tools and treatment options:
Diagnostic Methods
- Endoscopic Retrograde Cholangiopancreatography (ERCP): This is the most common diagnostic procedure, allowing visualization and direct access to the bile and pancreatic ducts. It can also be used therapeutically to remove stones or insert stents.
- Manometry: This is a specialized test used to measure the pressure within the Sphincter of Oddi. It is particularly useful in diagnosing Sphincter of Oddi Dysfunction (SOD).
- Ultrasound and Doppler Studies: These non-invasive imaging techniques can identify obstructions or anatomical abnormalities in the biliary and pancreatic ducts.
- Magnetic Resonance Cholangiopancreatography (MRCP): This imaging study provides detailed images of the bile and pancreatic ducts and can be an alternative to ERCP in some cases.
- Blood Tests: Elevated levels of liver enzymes or pancreatic enzymes can suggest issues with the Ampulla of Vater or Sphincter of Oddi.
- CT Scan: Sometimes used to visualize the area, especially if tumors are suspected.
Treatment Options
- Endoscopic Sphincterotomy: In this procedure, a small incision is made in the Sphincter of Oddi during an ERCP to relieve obstruction or to treat SOD.
- Stent Placement: A stent may be placed to keep a narrow duct open, especially if there is a tumor or severe stricture.
- Stone Removal: Gallstones or pancreatic duct stones causing obstruction can often be removed during ERCP.
- Medication: Antispasmodic drugs, antibiotics, or pain medications may be prescribed to manage symptoms.
- Surgical Intervention: In severe or complex cases, surgical options may include resection of a tumor or anatomical repair. Bypass surgery may also be considered in certain cases.
- Balloon Dilatation: Sometimes used to treat strictures or narrowings, often as part of an ERCP procedure.
- Lifestyle Changes: Diet and lifestyle changes may be recommended, particularly for less severe forms of SOD or other functional disorders.
It’s essential to consult a healthcare provider for an accurate diagnosis and appropriate treatment plan tailored to your specific condition. Early diagnosis and intervention are crucial for effective management and a better prognosis.
Healthy Practices for Digestive Well-being

An effective digestive system is key to overall wellbeing. Several lifestyle choices and habits can contribute to better digestive health, including the proper functioning of the Sphincter of Oddi and Ampulla of Vater:
Diet
- High-Fiber Foods: Consuming a diet rich in fiber helps keep the digestive tract moving and can prevent constipation.
- Hydration: Adequate water intake is vital for digestion and absorption of nutrients.
- Limited Processed Foods: Minimize intake of processed foods that are high in salt, sugar, and fats.
- Balanced Diet: Eat a healthy and well-rounded diet including plenty of fruits, vegetables, protein sources such as lean meats and whole wheat products.
Exercise
- Regular Physical Activity: Exercise stimulates normal peristalsis in the digestive tract.
- Core Exercises: Strengthening the muscles around the abdomen can help improve digestion.
Healthy Habits
- Regular Eating Schedule: Eating at consistent times helps regulate the digestive system.
- Mindful Eating: Eat slowly and chew thoroughly in order to aid digestion.
- Avoid Overeating: Heavy meals may overwhelm your digestive tract.
- Limit Alcohol and Caffeine: These can irritate the digestive system and exacerbate symptoms for those with existing issues.
Stress Management
- Meditation and Mindfulness: Stress can adversely affect the digestive system. Mindfulness techniques can help in stress management.
- Adequate Sleep: Poor sleep can negatively affect the digestive system. Try and aim to get at least 7 hours of uninterrupted slumber each night.
Medication and Supplements
- Probiotics: These can help maintain a healthy balance of gut flora, which is essential for digestion.
- Enzyme Supplements: For those with specific enzyme deficiencies, consult a healthcare provider for appropriate supplements.
Regular Check-ups
- Regular Screenings: Keep up with regular medical checkups and screenings to catch digestive issues early.
- Consult a Doctor for Persistent Issues: If you experience recurring digestive issues, seek medical advice for diagnosis and treatment.
Avoid Smoking and Excessive Alcohol
- Quit Smoking: Smoking can exacerbate digestive issues and increase the risk of gastrointestinal cancers.
- Limit Alcohol: Excessive alcohol intake can cause liver problems and impair digestion.
Remember, each individual is different, and it’s always best to consult healthcare providers for personalized advice. These general guidelines can serve as a starting point for most people in maintaining a healthy digestive system.
Final Thoughts
The Sphincter of Oddi and the Ampulla of Vater are crucial components of the digestive system, regulating the flow of bile and pancreatic juices into the small intestine. Disorders affecting these structures can lead to significant digestive issues, requiring a multi-disciplinary approach for diagnosis and treatment.
For general digestive well-being, a balanced diet, regular exercise, stress management, and timely medical check-ups are essential. Taking a proactive approach to digestive health can help ensure the optimal functioning of these important anatomical features and contribute to overall well-being.