T-Score and Z-Score Osteoporosis are central to this assessment process. These scores provide valuable insights into an individual’s bone density relative to established reference populations. Understanding the differences between T-Score and Z-Score is essential for clinicians and patients alike, as it guides diagnostic categorization and informs treatment decisions.
In this brief exploration, we will delve into the distinctions between T-Score and Z-Score, shedding light on their respective roles in osteoporosis assessment and contributing to more informed healthcare choices.
What is T-Score Osteoporosis?
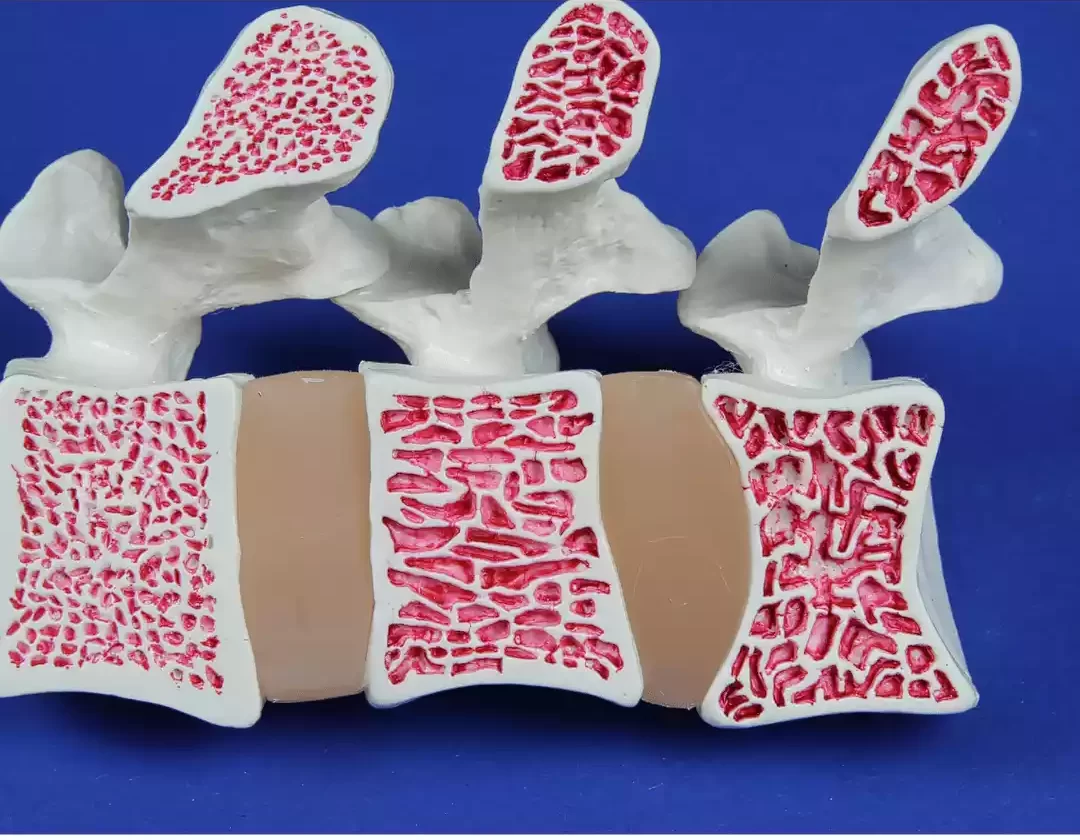
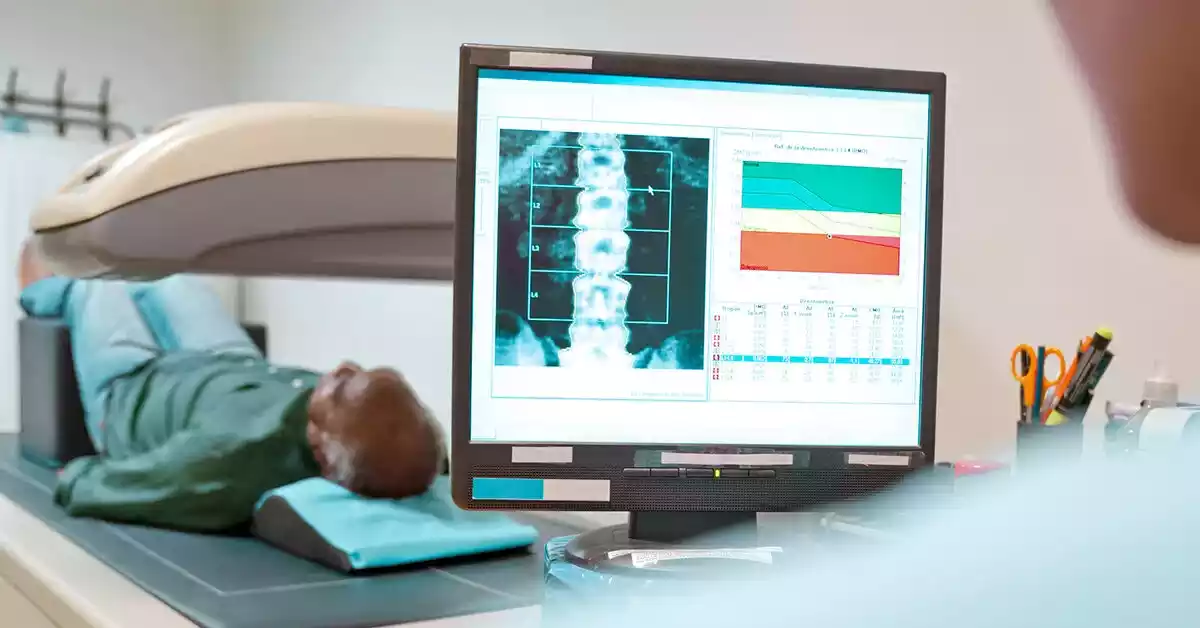
The T-Score in the context of osteoporosis is a standardized measurement to evaluate an individual’s bone density and diagnose the condition. Derived from Dual-energy X-ray Absorptiometry (DXA) scans, the T-Score compares a person’s bone mineral density (BMD) to the mean BMD of a healthy young adult reference population.
This comparison provides critical insights into an individual’s fracture risk and osteoporosis. Calculated using a formula that incorporates the patient’s BMD, the young adult mean BMD, and the standard deviation of BMD within the reference population, the T-Score categorizes bone health into three categories: normal, osteopenia (lower bone density), and osteoporosis (significantly reduced bone density).
By assessing an individual’s bone health relative to a young adult population, the T-Score serves as a cornerstone in diagnosing osteoporosis and guiding appropriate treatment strategies, primarily focusing on postmenopausal women and older men where age-related changes in bone density are significant.
What is Z-Score Osteoporosis?
The Z-Score in the context of osteoporosis represents a measurement employed to assess an individual’s bone density by comparing it to the mean bone density of a reference population with similar age, gender, and sometimes ethnicity. Unlike the T-Score, which compares bone density to a young adult reference population, the Z-Score takes into account an individual’s age-specific context.
Calculated using a formula involving the patient’s bone mineral density, the mean BMD of the age-matched reference group, and the standard deviation of BMD within that group, the Z-Score provides a personalized assessment of bone health. The Z-Score interpretation varies based on the individual’s age and demographic group, offering insights into potential secondary causes of low bone density, suboptimal bone health, or bone density within the expected range for period.
Particularly relevant in specific populations such as children, premenopausal women, and men, the Z-Score aids clinicians in identifying underlying causes of low bone density in younger individuals and tailoring appropriate interventions accordingly. It contributes to a more nuanced understanding of bone health beyond the traditional T-Score, taking into consideration age-related changes and demographic factors to inform osteoporosis diagnosis and management strategies.
Comparison Chart of T-Score and Z-Score Osteoporosis
Here’s a comparison chart highlighting the key differences between T-Score and Z-Score in the context of osteoporosis assessment:
| Aspect | T-Score | Z-Score |
|---|---|---|
| Definition | Compares bone density to young adult reference population | Compares bone density to age-matched reference group |
| Calculation | Patient’s BMD – Young Adult Mean BMD / Young Adult SD of BMD | Patient’s BMD – Mean BMD of Age-Matched Reference Group / SD of BMD of Age-Matched Reference Group |
| Reference Population | Healthy young adults | Individuals of the same age, gender, and sometimes ethnicity |
| Interpretation | -1.0 or above: Normal bone density<br>-1.0 to -2.5: Osteopenia<br>-2.5 or lower: Osteoporosis | Below -2: Concerns about secondary causes<br>-1 to -2: Suboptimal bone health<br>Above -1: Expected range for age and demographics |
| Applicability | Postmenopausal women, older men | All age groups, especially children, premenopausal women, and men |
| Clinical Focus | Primary diagnosis of osteoporosis | Identifying underlying causes in specific populations |
| Clinical Use | Assess fracture risk, guide treatment decisions | Detect secondary causes, and tailor interventions based on age group |
| Contextual Consideration | More relevant in older individuals | More applicable in diverse demographic groups |
| Diagnostic Thresholds | The key for defining osteoporosis diagnosis | May prompt further evaluation rather than a primary diagnosis |
This comparison chart provides a concise overview of the main differences between T-Score and Z-Score in osteoporosis assessment. For a comprehensive understanding, further context, and specific clinical applications, it’s important to refer to additional sources and professional medical guidance.
Limitations and Considerations
While both the T-Score and Z-Score are valuable tools in assessing bone health and diagnosing osteoporosis, it’s important to be aware of their limitations and consider contextual factors for accurate interpretation and decision-making.
- Population Variation: The T-Score and Z-Score calculations rely on reference populations, which may not perfectly represent diverse demographics. Differences in ethnicity, lifestyle, and genetics could impact the relevance of these scores.
- Age Considerations: The T-Score is most applicable to postmenopausal women and older men due to its comparison with a young adult reference population. The Z-Score, while more age-specific, might be less relevant in older individuals.
- Secondary Causes: Both scores might not capture bone density changes caused by secondary factors like medications, medical conditions, or hormonal imbalances. Low Z-Scores might indicate secondary causes rather than primary osteoporosis.
- Pediatric Considerations: The T-Score might not be suitable for children, whose bone density is still developing. The Z-Score is more appropriate in pediatric cases, but reference populations for different age ranges might vary.
- Clinical Context: Scores should always be considered in the context of an individual’s medical history, lifestyle, and risk factors. Clinicians should not rely solely on scores for diagnosis.
- Fracture Risk Prediction: While T-Scores correlate with fracture risk, they do not capture all factors influencing fractures, such as bone quality and trauma history.
- DXA Limitations: Both scores are derived from DXA scans, which might have limitations in specific cases (e.g., obese individuals, those with spinal abnormalities).
- Treatment Decisions: Scores guide but should not solely dictate treatment decisions. Clinical judgment and patient preferences are crucial in determining appropriate interventions.
- Evolution of Knowledge: Osteoporosis assessment is an evolving field. New research might influence score interpretations and management guidelines.
- Long-Term Monitoring: Overreliance on scores for monitoring can lead to unnecessary anxiety or treatments. Regular assessments, along with clinical evaluation, are essential.
While the T-Score and Z-Score provide valuable insights into bone health, they are tools within a broader context of patient assessment. Recognizing their limitations, understanding individual circumstances, and involving healthcare professionals in interpretation are essential for informed osteoporosis management.
Recent Developments and Research
Advancements in technology and evolving research have contributed to refining osteoporosis assessment methods and enhancing our understanding of bone health. Recent developments and research trends in the field include:
- Advanced Imaging Techniques: Beyond traditional DXA, newer imaging methods like quantitative computed tomography (QCT) and high-resolution peripheral quantitative computed tomography (HR-pQCT) offer enhanced insights into bone structure, microarchitecture, and strength, providing a more comprehensive assessment of fracture risk.
- Biomechanical Models: Computational modeling and finite element analysis are being integrated to simulate bone strength and predict fracture risk based on bone geometry, density distribution, and loading conditions, improving fracture prediction accuracy.
- Fracture Risk Assessment Tools: Emerging tools and algorithms, such as FRAX® (Fracture Risk Assessment Tool), incorporate multiple risk factors beyond bone density to provide a more holistic estimation of an individual’s fracture risk.
- Genetic Insights: Genetic studies have revealed specific genetic markers associated with bone health and fracture risk, allowing for more personalized risk prediction and potential drug targets.
- Precision Medicine: The concept of precision medicine is gaining ground, focusing on tailoring osteoporosis treatment plans based on an individual’s unique genetic, lifestyle, and clinical factors.
- Nutrition and Lifestyle Research: Recent studies explore the impact of nutrition, physical activity, and lifestyle on bone health, emphasizing preventive strategies to improve bone density and reduce fracture risk.
- Drug Developments: Continuous research in pharmacotherapy has led to the development of novel medications that target bone metabolism pathways, potentially offering more effective treatments with fewer side effects.
- Pediatric Osteoporosis: Growing attention to pediatric osteoporosis highlights the need for accurate assessment tools and treatment strategies for children and adolescents with bone health disorders.
- Telehealth and Monitoring: Technology-driven solutions, including remote DXA monitoring and telehealth consultations, are becoming more common, improving access to care and monitoring for individuals at risk.
- Machine Learning and AI: Artificial intelligence and machine learning are being employed to analyze complex data sets, aiding in predicting fracture risk, identifying bone abnormalities, and personalizing treatment recommendations.
- Biomarkers: Research into new biomarkers aims to identify early signs of bone turnover and fracture risk, potentially allowing for earlier interventions.
As research continues to progress, these developments promise to refine osteoporosis assessment, enhance personalized treatment approaches, and ultimately reduce the burden of fractures and bone-related health issues. Staying informed about these trends can empower healthcare providers and individuals to make more informed decisions regarding bone health.
The Last word
Understanding the nuances of osteoporosis assessment through T-Score and Z-Score is pivotal for accurate diagnosis and effective management. While the T-Score offers a standardized comparison to a young adult reference population, the Z-Score provides a personalized context based on age-matched peers.
Both scores have limitations and must be interpreted alongside clinical considerations. Recent advancements, such as advanced imaging, genetics, and precision medicine, are shaping a more comprehensive approach to bone health assessment and treatment. By embracing these developments, healthcare providers and individuals can work together to optimize bone health, reduce fracture risk, and improve overall quality of life.



