Introduction
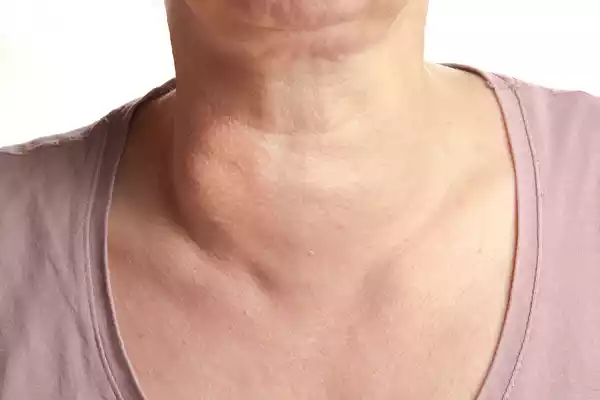
Goiter, a condition characterized by an enlarged thyroid gland, can be classified into two primary categories: toxic goiter and nontoxic goiter. These two conditions exhibit distinct characteristics, causes, symptoms, diagnostic methods, and treatments. Understanding the difference between toxic and nontoxic goiter is essential for healthcare professionals, patients, and anyone interested in thyroid disorders. In this comprehensive article, we will delve into both conditions, addressing their definitions, causes, symptoms, diagnostic procedures, treatments, potential complications, preventive measures, and draw a comparison between the two.
Toxic Goiter
Toxic goiter, also known as hyperthyroidism or overactive thyroid, is a condition in which the thyroid gland produces an excessive amount of thyroid hormones, primarily thyroxine (T4) and triiodothyronine (T3). This hyperactivity can lead to various symptoms and complications, making it a crucial concern in endocrinology and general healthcare.
Causes
- Graves’ Disease: The most common cause of toxic goiter is Graves’ disease, an autoimmune disorder where the immune system mistakenly stimulates the thyroid to produce excess hormones.
- Toxic Multinodular Goiter: This condition occurs when multiple nodules in the thyroid become overactive and produce excessive hormones.
- Toxic Adenoma: A toxic adenoma is a single nodule that autonomously produces excessive thyroid hormones, leading to hyperthyroidism.
- Iodine-Induced Toxic Goiter: Excessive intake of iodine through diet or medication can trigger an overproduction of thyroid hormones.
- Thyroiditis: Inflammation of the thyroid gland can cause the release of stored hormones, resulting in temporary hyperthyroidism.
Syndrome
The symptoms of toxic goiter are primarily a result of the elevated thyroid hormone levels in the bloodstream. These symptoms can be both physiological and psychological, including:
- Weight loss
- Increased appetite
- Nervousness and irritability
- Fatigue
- Tremors
- Heat intolerance
- Increased heart rate (tachycardia)
- Excessive sweating
- Insomnia
- Muscle weakness
- Frequent bowel movements
- Goiter (enlarged thyroid gland)
- Irregular menstrual periods in women
- Thinning of hair
- Protruding eyes (Graves’ Ophthalmopathy)
Nontoxic Goiter
Nontoxic goiter, on the other hand, is a condition characterized by an enlarged thyroid gland without the excessive production of thyroid hormones. In this condition, the thyroid gland enlarges to compensate for various factors that may disrupt its normal function.

Causes
- Iodine Deficiency: A lack of iodine in the diet is a common cause of nontoxic goiter. Iodine is essential for the synthesis of thyroid hormones, and when it’s insufficient, the thyroid gland enlarges in an attempt to produce more hormones.
- Hashimoto’s Thyroiditis: An autoimmune condition where the immune system attacks the thyroid gland, leading to inflammation and gradual thyroid enlargement.
- Subacute Thyroiditis: This condition is characterized by painful inflammation of the thyroid gland, causing transient enlargement.
- Pregnancy: Hormonal changes during pregnancy can cause a temporary enlargement of the thyroid gland, known as gestational goiter.
Syndrome
Nontoxic goiter doesn’t typically produce symptoms directly related to the thyroid gland’s enlargement. Symptoms, if present, are often associated with the underlying cause and may include:
- Neck swelling (goiter)
- Difficulty swallowing
- Difficulty breathing (if the goiter compresses the trachea)
- Coughing (if the goiter presses against the esophagus or trachea)
Comparison Table of Toxic and Nontoxic Goiter
Let’s present a detailed comparison of toxic and nontoxic goiter:
| Characteristic | Toxic Goiter | Nontoxic Goiter |
| Hormone Levels | Elevated T4 and T3 | Normal T4 and T3 levels |
| Primary Causes | Graves’ disease, toxic nodules, iodine excess, thyroiditis | Iodine deficiency, Hashimoto’s thyroiditis, subacute thyroiditis, pregnancy |
| Goiter Presence | Typically present | Always present |
| Symptoms | Hyperthyroidism symptoms (weight loss, tachycardia, etc.) | Generally, symptoms related to underlying condition (swelling, discomfort) |
| Risk of Complications | High, including heart problems, osteoporosis, eye issues | Low, unless related to the underlying condition (Hashimoto’s, subacute thyroiditis) |
| Diagnostic Tests | Thyroid function tests, radioactive iodine uptake, ultrasound | Thyroid function tests, ultrasound, fine-needle aspiration (if necessary) |
| Treatment Options | Antithyroid medication, radioactive iodine, surgery | Address underlying cause, medication (if necessary), surgery (rarely) |
| Prognosis | Good with treatment, but may require lifelong management | Generally good, unless associated with a severe underlying condition |
| Preventive Measures | No specific prevention for Graves’ disease, monitor iodine intake | Ensure adequate iodine intake, address autoimmune conditions, avoid known triggers |
Similarities between Toxic and Nontoxic Goiter
While toxic and nontoxic goiter differ significantly, they share certain similarities:
- Goiter Presence: Both conditions are characterized by the presence of a goiter, which is an enlarged thyroid gland.
- Diagnostic Methods: Diagnostic methods, such as ultrasound and thyroid function tests, are applicable to both conditions.
- Treatment Options: Surgical intervention may be necessary for both toxic and nontoxic goiters, although the specific approach varies.
- Risk of Complications: In some cases, both types of goiter may lead to complications, particularly if left untreated or associated with severe underlying conditions.
Exams and Tests for Toxic and Nontoxic Goiter
Diagnostic Tests for Toxic Goiter
- Thyroid Function Tests: These include measuring levels of TSH (thyroid-stimulating hormone), T4, and T3 in the blood. In toxic goiter, TSH is usually low, while T4 and T3 are elevated.
- Radioactive Iodine Uptake: This test helps determine how much iodine the thyroid gland takes up. High uptake indicates an overactive gland.
- Thyroid Scan: A thyroid scan, often performed along with the iodine uptake test, helps identify nodules or areas of the thyroid that may be overactive.
- Ultrasound: An ultrasound can provide detailed images of the thyroid gland, helping to identify the size and shape of the gland and any nodules or masses.
Diagnostic Tests for Nontoxic Goiter
- Thyroid Function Tests: As in toxic goiter, thyroid function tests help assess the levels of TSH, T4, and T3. However, in nontoxic goiter, these levels typically remain within the normal range.
- Ultrasound: Ultrasound is an essential tool for evaluating the size and structure of the thyroid gland and identifying the presence of nodules or masses.
- Fine-Needle Aspiration (FNA): If a nontoxic goiter is associated with nodules that raise concern, an FNA biopsy may be performed to rule out cancer.
Treatment for Toxic and Nontoxic Goiter
Treatment for Toxic Goiter
The treatment of toxic goiter aims to normalize thyroid hormone levels, alleviate symptoms, and address the underlying cause. Treatment options include:
- Antithyroid Medications: Drugs like methimazole and propylthiouracil are used to reduce the production of thyroid hormones. These are commonly prescribed for Graves’ disease.
- Radioactive Iodine Therapy: Orally administered radioactive iodine can be consumed and absorbed by the thyroid gland. It gradually reduces the thyroid’s activity, eventually leading to hypothyroidism.
- Thyroidectomy: Surgical removal of part or all of the thyroid gland is a treatment option when other methods are ineffective or not suitable. It may be the preferred option in certain cases, such as when a goiter is causing compression symptoms or if there is suspicion of thyroid cancer.
Treatment for Nontoxic Goiter
The treatment of nontoxic goiter focuses on addressing the underlying cause and managing symptoms. Treatment options include:
- Iodine Supplementation: In cases of iodine deficiency, iodine supplements or dietary changes to increase iodine intake can help reduce the size of the goiter.
- Levothyroxine (T4) Medication: In some cases, synthetic thyroid hormone replacement with levothyroxine may be prescribed to help shrink the goiter and normalize thyroid function.
- Treatment of Underlying Conditions: When nontoxic goiter is a result of autoimmune conditions like Hashimoto’s thyroiditis or subacute thyroiditis, treatment involves managing these conditions, which may include anti-inflammatory medications.
- Surgery: Surgical removal of the goiter may be considered in cases of significant enlargement, discomfort, or if there is concern about malignancy.
Possible Complications
Complications of Toxic Goiter
- Heart Problems: Persistent high thyroid hormone levels can lead to heart issues, including tachycardia, high blood pressure, and an increased risk of heart disease.
- Osteoporosis: Excess thyroid hormone can lead to bone loss, increasing the risk of osteoporosis.
- Thyroid Storm: In severe cases, untreated toxic goiter can result in a life-threatening condition known as thyroid storm, characterized by extreme symptoms like fever, confusion, and organ failure.
- Eye Problems (Graves’ Ophthalmopathy): Graves’ disease can cause eye-related complications, including eye bulging, double vision, and eye discomfort.
Complications of Nontoxic Goiter
- Compression Symptoms: A large goiter can compress the trachea or esophagus, leading to breathing or swallowing difficulties.
- Thyroid Nodules: In some cases, nodules within a nontoxic goiter may become cancerous, requiring additional treatment.
- Psychological Impact: The physical appearance of a goiter can have a psychological impact, leading to body image issues and self-esteem concerns.
Prevention of Toxic and Nontoxic Goiter
Prevention of Toxic Goiter
Toxic goiter prevention is challenging, especially in the case of Graves’ disease, which is an autoimmune condition. Some general measures can help manage symptoms and reduce the risk of complications:
- Stress Management: Reducing stress through relaxation techniques can help manage symptoms of Graves’ disease.
- Eye Care: For individuals with Graves’ ophthalmopathy, proper eye care can help alleviate discomfort.
Prevention of Nontoxic Goiter
Preventing nontoxic goiter primarily involves addressing the underlying causes:
- Iodine Supplementation: Ensuring an adequate intake of iodine through diet or supplementation can prevent iodine-deficiency goiter.
- Treating Autoimmune Conditions: If the goiter is associated with an autoimmune condition, such as Hashimoto’s thyroiditis, managing the autoimmune disease can prevent further thyroid enlargement.
- Thyroid Health Awareness: Regular check-ups and thyroid health awareness can help identify and address thyroid issues early.
Conclusion
Toxic and Nontoxic Goiters represent two distinct thyroid disorders, with toxic goiter marked by excessive hormone production and nontoxic goiter characterized by thyroid enlargement without hormone overproduction. Accurate diagnosis, tailored treatment, and management of underlying causes are crucial for both conditions. Toxic goiter poses higher risks of complications, while nontoxic goiter primarily affects thyroid size. Understanding these differences empowers healthcare professionals and patients to make informed decisions, ensuring optimal care and improved quality of life.



