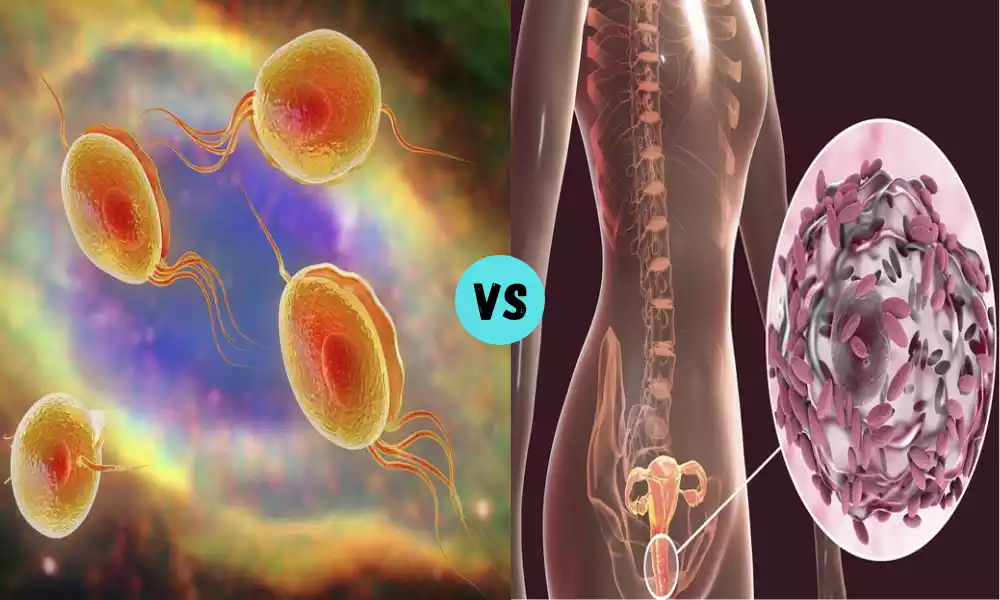
Trichomonas and Gardnerella are two distinct yet common vaginal infections that predominantly affect women. Trichomonas is caused by a parasitic organism called Trichomonas vaginalis and leads to a range of uncomfortable symptoms. On the other hand, Gardnerella infection, also known as bacterial vaginosis (BV), is caused by the bacterium Gardnerella vaginalis and presents its own set of distinct symptoms. Understanding these infections is crucial for women’s health and well-being.
Trichomonas

Trichomonas is a term that refers to a genus of single-celled protozoan parasites. The most well-known species within this genus is Trichomonas vaginalis. These parasites are typically found in the urogenital tract of humans and other animals and are known to cause infections in their respective hosts.
Trichomonas vaginalis, specifically, is responsible for causing trichomoniasis, which is a common sexually transmitted infection (STI) in humans. This protozoan parasite has a pear-shaped morphology and is equipped with flagella, which enables it to move within the urogenital tract. Trichomonas vaginalis primarily infects the urogenital mucous membranes, leading to symptoms such as vaginal itching, burning, pain during urination, and a frothy, greenish-yellow vaginal discharge in women. In men, it can cause urethritis.
Trichomonas infections are typically transmitted through sexual contact, including vaginal, anal, or oral intercourse. Proper diagnosis and treatment are essential to manage trichomoniasis and prevent complications. Treatment often involves the use of antimicrobial medications, such as metronidazole or tinidazole, to eliminate the infection. It is important for both sexual partners to be treated simultaneously to prevent re-infection.
Trichomonas refers to a genus of protozoan parasites, with Trichomonas vaginalis being the most notable species within this genus. Trichomonas vaginalis is responsible for causing trichomoniasis, a sexually transmitted infection in humans.
Symptoms of Trichomonas Infection
Symptoms of Trichomonas Infection typically include:
- Vaginal Itching: Persistent itching in the vaginal area.
- Painful Urination: A burning sensation or pain during urination.
- Foul Odor: A distinctive, unpleasant odor from vaginal discharge.
- Discomfort During Intercourse: Sexual intercourse can become painful.
- Genital Redness and Swelling: The genital area may appear red and swollen.
Some individuals infected with Trichomonas may not display noticeable symptoms, underscoring the importance of regular screenings, especially for sexually active individuals.
Causes of Trichomonas Infections
Here are the causes of Trichomonas Infections:
- Trichomonas vaginalis Parasite: Trichomonas infections, also known as trichomoniasis, are primarily caused by the presence of the parasitic microorganism Trichomonas vaginalis in the genital tract.
- Sexual Transmission: The most common mode of transmission is through sexual contact. Unprotected sex with an infected partner can lead to the transfer of the parasite, resulting in an infection.
- Asymptomatic Carriers: Some individuals may carry the Trichomonas parasite without exhibiting any noticeable symptoms. These carriers can unknowingly transmit the infection to their sexual partners.
- Shared Objects (Rare): While less common, there is a theoretical possibility of Trichomonas transmission through shared objects like towels or wet clothing. Sexual contact remains the primary and most significant mode of transmission.
Practicing safe sex, using condoms consistently, and seeking medical attention if symptoms arise are crucial steps to prevent the spread of Trichomonas infections and potential complications.
Gardnerella
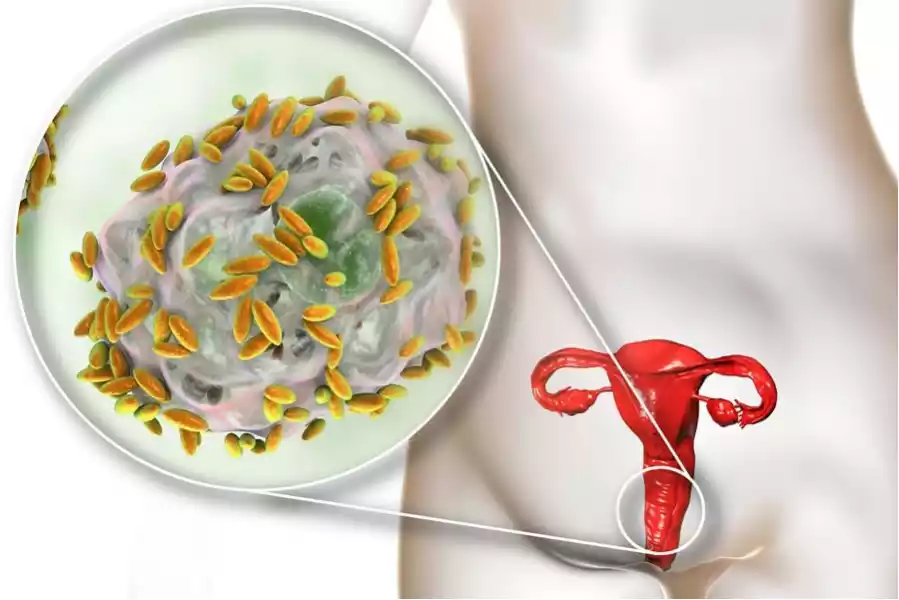
Gardnerella refers to a genus of bacteria and the most well-known species within this genus is Gardnerella vaginalis. Gardnerella vaginalis is a bacterium that is commonly associated with a condition called bacterial vaginosis (BV), which is characterized by an imbalance in the vaginal microbiota. BV is not considered a sexually transmitted infection (STI) but rather a disruption in the normal microbial balance within the vagina.
Gardnerella vaginalis is a small, rod-shaped bacterium that can be found in the vaginal ecosystem. In cases of bacterial vaginosis, there is an overgrowth of Gardnerella vaginalis and other bacterial species that normally inhabit the vagina. This overgrowth can lead to symptoms such as a thin, grayish-white vaginal discharge with a distinct fishy odor. It’s important to note that many cases of BV are asymptomatic.
The exact cause of BV and the role of Gardnerella vaginalis in its development are still subjects of research. It is believed that various factors, such as sexual activity, douching, hormonal changes, and the use of certain hygiene products, can contribute to the disruption of the vaginal microbiota.
Diagnosis of bacterial vaginosis involves clinical evaluation and may also include microscopic examination of vaginal discharge along with the use of the Nugent score, a scoring system that assesses the bacterial morphotypes in vaginal smears.
Treatment of bacterial vaginosis usually involves antibiotics, such as metronidazole or clindamycin, to restore the balance of vaginal bacteria. Preventive measures include promoting vaginal health by avoiding douching, using mild hygiene products, and maintaining good sexual hygiene practices.
Gardnerella refers to a genus of bacteria, and Gardnerella vaginalis is a bacterium associated with bacterial vaginosis, a condition characterized by an imbalance in the vaginal microbiota. It’s important to note that BV is not considered an STI but rather a disruption of the normal vaginal microbial balance.
Symptoms of Gardnerella Infection
Here are the symptoms of Gardnerella Infection:
- Thin Grayish-White Discharge: Gardnerella infection, also known as bacterial vaginosis (BV), often leads to a thin, grayish-white vaginal discharge.
- Fishy Odor: The discharge may have a distinct fishy odor, especially after sexual intercourse.
- Vaginal Itching: People living with BV may also experience vaginal itching or irritation.
- Discomfort: Women with bacterial vaginosis may feel general discomfort in the vaginal area.
- Pain During Urination or Sex: BV can sometimes lead to pain or discomfort during urination or sexual intercourse.
It’s essential to note that not all individuals with Gardnerella infection will experience noticeable symptoms, highlighting the importance of seeking medical advice for proper diagnosis and treatment, especially if symptoms are present.
Causes of Gardnerella Infections
Here are the causes of Gardnerella Infections:
- Gardnerella vaginalis Bacterium: Gardnerella infections, also known as bacterial vaginosis (BV), are primarily caused by an overgrowth of the bacterium Gardnerella vaginalis in the vaginal flora.
- Vaginal Microbiome Imbalance: BV occurs when there is a disturbance in the delicate balance of the vaginal microbiome. This imbalance can lead to an overgrowth of harmful bacteria like Gardnerella vaginalis.
- Multiple Sexual Partners: Having multiple sexual partners can increase the risk of developing bacterial vaginosis. It may disrupt the natural equilibrium of vaginal bacteria.
- Douching: The practice of douching, or using vaginal washes and cleansers, can interfere with the vaginal microbiome and increase susceptibility to BV.
- Poor Genital Hygiene: Inadequate genital hygiene practices can contribute to the development of Gardnerella infections by allowing harmful bacteria to thrive.
- Weakened Immune System: Individuals with weakened immune systems may be more susceptible to BV and other vaginal infections.
Maintaining good genital hygiene, practicing safe sex, and avoiding douching are essential steps to help prevent Gardnerella infections and maintain a healthy vaginal microbiome.
Risk Factors for Infection
Several risk factors can increase the likelihood of contracting Trichomonas and Gardnerella infections, which affect the vaginal and genital health of individuals, particularly women. These risk factors include:
- Unprotected Sexual Activity: Engaging in sexual intercourse without the use of condoms or other barrier methods can expose individuals to sexually transmitted infections (STIs) like Trichomonas and Gardnerella.
- Multiple Sexual Partners: Having multiple sexual partners can elevate the risk of encountering infected individuals and, consequently, the risk of infection.
- History of Infections: A previous history of Trichomonas or Gardnerella infections can increase susceptibility to future occurrences.
- Poor Genital Hygiene: Inadequate genital hygiene practices can contribute to the development and persistence of these infections.
- Douching: Douching, or the use of vaginal washes and cleansers, can disrupt the natural balance of vaginal flora, making it easier for harmful microorganisms to thrive.
- Weakened Immune System: A compromised immune system, often due to conditions like HIV/AIDS or immunosuppressive medications, can reduce the body’s ability to fight off infections.
- Certain Medications: The use of antibiotics or medications that affect the balance of vaginal bacteria can increase the risk of Gardnerella infection.
- Hormonal Changes: Hormonal fluctuations, such as those occurring during pregnancy or menopause, can alter the vaginal environment and potentially increase vulnerability to infections.
- Personal Habits: Lifestyle factors, such as smoking and poor diet, can impact health, including immune function and susceptibility to infections.
- Partner’s Infection Status: If a sexual partner is infected with Trichomonas or Gardnerella and remains untreated, it can lead to reinfection.
It’s essential for individuals to be aware of these risk factors and take preventive measures to reduce their chances of contracting these infections. This includes practicing safe sex, maintaining good genital hygiene, and seeking timely medical attention if symptoms or risk factors are present. Regular screenings and open communication with healthcare providers can also play a crucial role in early detection and management.
Diagnosis of Trichomonas and Gardnerella Infections
Diagnosing Trichomonas and Gardnerella infections involves specific methods conducted by healthcare professionals to confirm these conditions. Here’s how these infections are typically diagnosed:
Diagnosis of Trichomonas Infection (Trichomoniasis):
- Physical Examination: A healthcare provider may start with a physical examination to check for any visible signs of infection, such as redness or swelling of the genital area.
- Microscopic Examination: To confirm trichomoniasis, a sample (swab) is taken from the vaginal area or urethra in men. Examining a sample under microscope. Healthcare providers look for the presence of Trichomonas vaginalis parasites. This microscopic examination is known as a “wet mount” or “saline preparation.”
- Cultures: A laboratory culture test may be performed. A sample is collected and placed in a culture medium, allowing the Trichomonas parasites to grow over time. This makes it easier to identify them.
Diagnosis of Gardnerella Infection (Bacterial Vaginosis – BV):
- Physical Examination: A healthcare provider may conduct a physical examination to assess the genital area for any visible signs of infection or inflammation.
- Vaginal pH Testing: Testing the vaginal pH level is common in diagnosing BV. BV often leads to an elevated vaginal pH, which can be detected using pH test strips.
- Whiff Test: In the “whiff test,” a healthcare provider adds a solution of potassium hydroxide (KOH) to a sample of vaginal discharge. A distinct fishy odor may be produced if BV is present.
- Microscopic Examination: Similar to trichomoniasis, a sample is collected from the vaginal area and examined under a microscope. In the case of BV, healthcare providers look for an overgrowth of Gardnerella vaginalis bacteria and the presence of clue cells, which are vaginal cells coated with bacteria.
Accurate diagnosis by a healthcare professional is essential for both Trichomonas and Gardnerella infections because they share symptoms with other conditions. Self-diagnosis and self-treatment are not recommended. Timely and precise diagnosis is crucial for appropriate treatment and effective management of these infections.
Treatment Options for Trichomonas and Gardnerella infections

Here are the treatment options for Trichomonas and Gardnerella infections:
Treatment Options for Trichomonas Infection (Trichomoniasis):
- Antibiotics: Trichomoniasis is typically treated with antibiotics, such as metronidazole (Flagyl) or tinidazole (Tindamax), which are taken orally. They can be prescribed as a single dose or a multi-day course.
- Partner Treatment: To prevent reinfection, it is imperative that sexual partners receive treatment simultaneously. Abstaining from sexual activity until both partners have completed treatment is advisable.
- Follow-Up Testing: After treatment, follow-up testing may be recommended to confirm that the infection has been successfully cleared.
Treatment Options for Gardnerella Infection (Bacterial Vaginosis – BV):
- Antibiotics: Bacterial vaginosis is treated with antibiotics, such as metronidazole (Flagyl) or clindamycin (Cleocin). These antibiotics can be administered orally as pills or as topical creams or gels inserted into the vagina.
- Avoid Douching and Scented Products: To prevent recurrence, it’s essential to refrain from douching and using scented personal care products that can disrupt the vaginal flora.
- Regular Follow-Up: Attend follow-up appointments to ensure the infection has been successfully treated, especially if symptoms persist or recur.
- Recurrent Infections: Recurrent BV, healthcare providers may recommend extended courses of antibiotics or alternative treatments.
Complete the full course of antibiotics as prescribed, even if symptoms improve before finishing the medication. This helps ensure all infectious agents are eradicated. During treatment, abstaining from sexual intercourse is advised to prevent the spread of infection and irritation. Maintaining good genital hygiene practices and following healthcare provider guidance can support successful treatment and prevent reinfection.
Preventing Infections
Here are preventive measures for Trichomonas and Gardnerella infections:
Preventing Trichomonas and Gardnerella Infections:
- Safe Sex: Consistently use condoms or other barrier methods during sexual activity to reduce the risk of contracting or spreading these infections.
- Limit Sexual Partners: Reducing the number of sexual partners can decrease the likelihood of encountering infected individuals.
- Good Genital Hygiene: Practice proper genital hygiene, which includes regular washing with mild soap and water. Do not use harsh or fragrant products on the genital region.
- Avoid Douching: Refrain from douching, as it can disrupt the natural balance of vaginal flora and increase the risk of infection.
- Regular Screenings: For sexually active individuals, regular screenings and check-ups can detect infections early, allowing for prompt treatment.
- Partner Awareness: Communicate openly with sexual partners about your sexual health and encourage them to seek medical attention if they suspect an infection.
- Preventive Care: If you’ve had these infections before, follow your healthcare provider’s recommendations for preventive care and treatment.
- Maintain a Healthy Lifestyle: A healthy lifestyle, including a balanced diet and not smoking, can support immune system health and reduce susceptibility to infections.
- Stay Informed: Keep yourself informed about sexual health, safe practices, and the signs and symptoms of these infections.
By adopting these preventive measures, individuals can reduce their risk of contracting Trichomonas and Gardnerella infections and maintain better vaginal and genital health.
Maintaining Vaginal Health
Maintaining vaginal health involves:
- Wearing breathable underwear.
- Avoiding tight-fitting clothing.
- Using unscented personal care products.
- Practicing safe sex with condoms.
- Seeking regular check-ups and screenings.
The Importance of Hygiene
Here’s the importance of hygiene presented:
- Personal Health: Good personal hygiene is essential for preventing illnesses and infections, keeping individuals healthy.
- Disease Prevention: Hygiene practices, especially handwashing, are crucial in preventing the transmission of diseases, reducing the risk of outbreaks.
- Mental Well-being: Maintaining cleanliness and grooming can boost self-esteem and contribute to positive mental well-being.
- Social and Professional Interactions: Proper personal hygiene is a societal norm that enhances social relationships and professional opportunities.
- Community Health: Public hygiene practices, like clean water and waste management, are vital for community health and preventing waterborne diseases.
- Environmental Sustainability: Responsible hygiene practices extend to environmental stewardship, helping conserve natural resources and reduce pollution.
By recognizing the significance of hygiene in these areas, individuals and communities can prioritize practices that promote health, well-being, and sustainability.
Comparison table of Trichomonas and Gardnerella
Here’s a comparison table highlighting the key differences between Trichomonas and Gardnerella infections:
| Aspect | Trichomonas Infection | Gardnerella Infection |
|---|---|---|
| Causative Agent | Trichomonas vaginalis, a parasitic protozoan | Gardnerella vaginalis, a bacterium |
| Transmission | Primarily through sexual contact | Not considered a classic sexually transmitted infection (STI); can occur in women with or without sexual activity |
| Symptoms | – Vaginal itching
– Burning during urination – Foul-smelling discharge – Discomfort during intercourse – Genital redness and swelling |
– Thin grayish-white vaginal discharge
– Fishy odor, especially after sex – Vaginal itching – Discomfort during sex – Some individuals may remain asymptomatic |
| Diagnostic Methods | – Microscopic examination of vaginal discharge
– Culture tests |
– Vaginal pH testing
– “Whiff test” with KOH solution – Microscopic examination of vaginal discharge |
| Treatment | Antibiotics (metronidazole or tinidazole) | Antibiotics (metronidazole or clindamycin) |
| Partner Treatment | Recommended for prevention of reinfection | Generally not necessary |
| Prevention Strategies | – Safe sex practices
– Limiting sexual partners – Good genital hygiene |
– Good genital hygiene
– Avoiding douching – Regular screenings |
This table provides a concise overview of the main differences between Trichomonas and Gardnerella infections, including their causes, transmission, symptoms, diagnostic methods, treatment, and prevention strategies.
Conclusion
Trichomonas and Gardnerella infections can pose challenges to women’s health and well-being. Recognizing the symptoms, understanding the causes, and adopting preventive measures are vital steps in maintaining vaginal health. With proper hygiene, safe sexual practices, and timely medical care, women can minimize the impact of these infections on their lives.