CRP and SED Rate are vital markers used in medicine to detect inflammation within the body. CRP is a protein produced by the liver in response to inflammation, while the SED Rate measures how quickly red blood cells settle in a test tube over time. Elevated levels of these markers indicate the presence of inflammation, helping medical professionals diagnose and manage various health conditions.
What is CRP?

C-reactive proteins (CRP) is produced by your liver as an immune response against inflammation. It is classified as an acute-phase protein, meaning its levels increase rapidly in the bloodstream in response to various inflammatory processes occurring in the body. CRP is part of the body’s natural defense mechanism against infections, injuries, and other types of inflammation.
CRP levels can rise within hours of the onset of inflammation, making it a valuable marker for identifying and monitoring acute inflammatory conditions. Doctors often measure CRP levels through a blood test to help diagnose and monitor various medical conditions, including infections, autoimmune diseases, and cardiovascular diseases.
High levels of CRP are often associated with conditions such as bacterial infections, viral infections, tissue injury, and chronic inflammatory disorders. It’s important to note that while elevated CRP levels indicate inflammation, they are not specific to a particular condition. Further tests and clinical evaluation are usually needed to determine the underlying cause of the inflammation.
CRP testing is widely used in clinical practice to assess the severity of inflammation, track the progress of treatment, and monitor disease activity. It can provide valuable insights into a patient’s health status and aid healthcare professionals in making informed decisions about their care.
Role of CRP in the Body
The C-reactive protein (CRP) plays a crucial role in the body’s immune response and inflammation process. Its main functions include:
- Indicator of Inflammation: CRP is a sensitive marker of acute inflammation. When the body detects an injury, infection, or any inflammatory process, the liver responds by producing more CRP. This rapid increase in CRP levels serves as an early warning signal that alerts the immune system to the presence of potential threats.
- Activation of Complement System: CRP is part of the innate immune system, which provides immediate defense against pathogens. It binds to damaged cells, bacteria, and other foreign substances, helping to activate the complement system—a group of proteins that work together to eliminate harmful agents. This promotes phagocytosis (engulfing and digestion of pathogens by immune cells) and the recruitment of immune cells to the site of inflammation.
- Opsonization: CRP enhances the process of opsonization, where it binds to pathogens and labels them for destruction by immune cells. This makes it easier for immune cells to recognize and eliminate the foreign invaders.
- Anti-Inflammatory Effects: While CRP is associated with inflammation, some research suggests that it might also have anti-inflammatory properties. It can modulate immune responses by interacting with different cells and molecules involved in inflammation.
- Tissue Repair and Remodeling: After inflammation, CRP levels typically decrease as the body resolves the inflammatory process. CRP might also play a role in tissue repair and remodeling during the recovery phase.
- Cardiovascular Health: Elevated CRP levels have been linked to cardiovascular diseases. CRP can contribute to the formation of atherosclerotic plaques by promoting inflammation within blood vessels. Monitoring CRP levels can help identify individuals at higher risk of heart disease.
- Monitoring Disease: CRP levels are often monitored in patients with chronic inflammatory conditions, such as rheumatoid arthritis and inflammatory bowel diseases. Changes in CRP levels can provide insights into disease activity and the effectiveness of treatment.
It’s important to note that while CRP is a valuable marker of inflammation and immune response, it’s not specific to any particular condition. Elevated CRP levels can be indicative of various health issues, and further diagnostic tests are usually required to determine the underlying cause of inflammation.
Significance in Inflammation Detection
The significance of C-Reactive Protein (CRP) in inflammation detection lies in its role as a sensitive and rapid marker for identifying and monitoring inflammatory processes within the body.
Here’s why CRP is crucial in this context:
- Early Detection: CRP levels can rise within hours of the onset of inflammation. This rapid response makes it an excellent indicator for detecting acute inflammatory conditions at an early stage. This is particularly important for timely diagnosis and intervention, as well as for tracking the progress of treatment.
- Broad Sensitivity: CRP is a nonspecific marker of inflammation, meaning it responds to a wide range of inflammatory stimuli. This versatility makes it useful for detecting various types of inflammation, including infections, injuries, autoimmune disorders, and other inflammatory diseases.
- Infection Monitoring: Elevated CRP levels often accompany infections caused by bacteria, viruses, and other pathogens. Monitoring CRP levels can help differentiate between viral and bacterial infections and gauge the severity of the infection.
- Disease Activity: For chronic inflammatory diseases like rheumatoid arthritis, inflammatory bowel disease, and lupus, CRP levels can indicate disease activity and flare-ups. Changes in CRP levels can guide treatment adjustments and therapeutic decisions.
- Post-Surgery Monitoring: After surgical procedures or trauma, CRP levels can rise as part of the body’s healing response. Monitoring CRP post-surgery can help detect potential complications or infections.
- Cardiovascular Risk Assessment: CRP has been linked to cardiovascular diseases. Measuring CRP levels is used as an additional tool for assessing the risk of heart disease and evaluating overall cardiovascular health.
- Response to Treatment: Monitoring CRP levels during treatment can provide insights into how well the therapy is working. Decreasing CRP levels often indicate that inflammation is subsiding, whereas persistently high levels might necessitate a change in treatment strategy.
- Research and Clinical Trials: CRP levels are often used as an outcome measure in clinical trials assessing the effectiveness of new drugs and therapies for inflammatory conditions. Changes in CRP levels can help determine the treatment’s impact.
It’s important to emphasize that while CRP is highly valuable for detecting inflammation, it’s a nonspecific marker. Elevated CRP levels can occur in various situations, and additional clinical evaluation is required to determine the underlying cause of the inflammation. Combining CRP measurements with other diagnostic tools and medical assessments provides a comprehensive view of the patient’s health status.
What is SED Rate?
The Erythrocyte Sedimentation Rate (ESR), commonly known as the “sed rate,” is a medical test used to assess the presence of inflammation in the body. It involves measuring the rate at which red blood cells settle to the bottom of a vertical tube over a specific period, usually one hour.
During inflammatory processes, proteins in the blood called fibrinogen and globulins increase, causing red blood cells to clump together and settle more quickly. As a result, a higher ESR value indicates a greater rate of sedimentation, suggesting the possible presence of inflammation or tissue damage.
ESR is a nonspecific marker, meaning it doesn’t pinpoint the exact cause of inflammation but serves as a general indicator. It can be influenced by factors other than inflammation, such as age, gender, anemia, and pregnancy.
While ESR is commonly used in diagnosing and monitoring conditions like rheumatoid arthritis, systemic lupus erythematosus, and temporal arteritis, its limitations should be considered. A normal ESR doesn’t rule out the presence of disease, and additional tests and clinical evaluation are usually needed to determine the underlying cause of inflammation.
How SED Rate is Measured?
The Erythrocyte Sedimentation Rate (ESR) is measured through a simple laboratory test that involves the following steps:
- Blood Collection: A healthcare professional will draw a blood sample from a vein, typically from your arm. The blood is collected in a tube that contains an anticoagulant, a substance that prevents the blood from clotting.
- Preparing the Test: The collected blood is mixed gently with an anticoagulant to prevent clotting and ensure uniform distribution of blood cells.
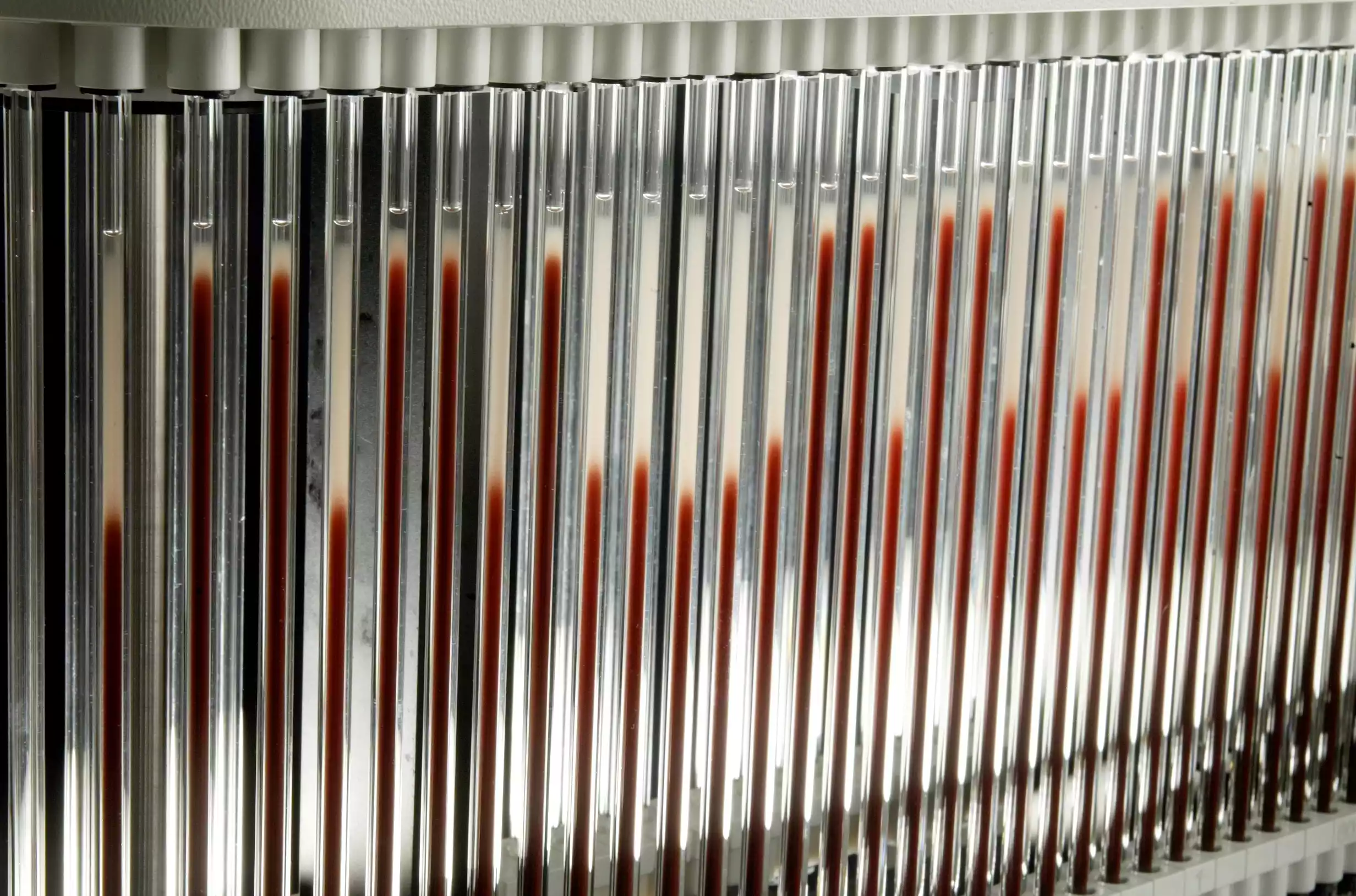
- Setting Up the Test Tube: The well-mixed blood is then placed in a tall, thin tube called a Westergren tube. The tube is usually marked with a scale in millimeters to measure the distance the red blood cells settle over time.
- Vertical Positioning: The Westergren tube is placed vertically in a special rack, allowing the blood to settle undisturbed. The tube is positioned upright for a specific duration, often one hour.
- Sedimentation: During the hour, gravity causes the red blood cells to settle to the bottom of the tube. The rate at which they settle is influenced by factors like the size and shape of the red blood cells, as well as the presence of inflammation-related proteins in the blood.
- Measuring the Result: After the designated time, the distance the red blood cells have fallen is measured in millimeters. This distance, known as the sedimentation rate, is recorded as the test result.
- Interpreting the Result: A higher sedimentation rate indicates that the red blood cells settled more quickly, which can be a sign of increased inflammation in the body. The sedimentation rate is a nonspecific marker and does not provide detailed information about the cause or location of inflammation.
It’s important to note that while the ESR test is a straightforward procedure, it is not specific to any particular condition. Elevated ESR levels can be indicative of various health issues, including infections, autoimmune diseases, and inflammatory conditions. As such, the ESR result is often considered alongside other clinical and laboratory findings to aid in the diagnosis and monitoring of health conditions.
Comparison Table of CRP and SED Rate
Here’s a comparison table highlighting the differences between C-Reactive Protein (CRP) and Erythrocyte Sedimentation Rate (ESR):
| Aspect | C-Reactive Protein (CRP) | Erythrocyte Sedimentation Rate (ESR) |
|---|---|---|
| Measurement | Measured directly in blood serum. | Measured indirectly through blood sedimentation rate in a vertical tube. |
| Sensitivity to Inflammation | Highly sensitive to acute inflammation and rapid changes. | Sensitive to inflammation but changes occur more slowly compared to CRP. |
| Specificity | Less specific; elevated levels indicate general inflammation but not the specific cause. | Nonspecific; elevated levels suggest inflammation without pinpointing the exact cause. |
| Rate of Change | Increases rapidly within hours of inflammation onset. | Changes occur more gradually, often over days. |
| Clinical Applications | Widely used to assess disease activity, monitor treatment response, and predict cardiovascular risk. | Used as a screening tool for inflammation, monitoring chronic inflammatory conditions, and assessing disease progression. |
| Influence of Factors | Less influenced by factors like age, gender, and anemia. | Can be affected by various factors beyond inflammation, including anemia, age, and gender. |
| Specific Conditions | Commonly used in assessing infections, autoimmune diseases, and cardiovascular risk. | Often used in diagnosing and monitoring inflammatory diseases like rheumatoid arthritis and temporal arteritis. |
| Test Procedure | Requires a blood sample and laboratory analysis. | Involves simple blood collection and measuring the sedimentation rate in a specialized tube. |
| Rapid Changes | Reflects rapid changes in inflammation status. | Reflects changes in inflammation, but changes occur more gradually. |
| Diagnostic Significance | Often used as an indicator of infection or acute inflammation. | Used to assess the presence of inflammation without identifying the specific cause. |
It’s important to note that while both CRP and ESR are valuable tools for assessing inflammation in the body, they are nonspecific markers. Elevated levels of these markers indicate the presence of inflammation but do not provide a definitive diagnosis of the underlying condition. Further diagnostic tests and clinical evaluation are usually required to determine the specific cause of the inflammation.
Clinical Applications and Interpretation
Clinical Applications and Interpretation of CRP (C-Reactive Protein) and ESR (Erythrocyte Sedimentation Rate):
C-Reactive Protein (CRP):
- Clinical Applications:
- Infection Detection: Elevated CRP levels can indicate the presence of infections, especially bacterial infections.
- Inflammatory Disorders: Used to monitor and assess disease activity in conditions like rheumatoid arthritis, lupus, and inflammatory bowel diseases.
- Cardiovascular Risk: CRP is considered a marker for cardiovascular risk. Elevated levels might suggest an increased risk of heart disease.
- Postoperative Monitoring: Used to detect complications or infections after surgical procedures.
- Response to Treatment: Monitoring CRP levels helps assess the effectiveness of treatments and therapies for various inflammatory conditions.
- Interpretation: Higher CRP levels typically indicate active inflammation. Rapid increases suggest acute conditions like infections, while persistent elevations can signal chronic inflammation. Lower levels indicate a reduced inflammatory response.
Erythrocyte Sedimentation Rate (ESR):
- Clinical Applications:
- Inflammation Screening: Used as a general indicator of inflammation, often as part of initial health assessments.
- Chronic Inflammatory Diseases: Useful for diagnosing and monitoring chronic conditions like rheumatoid arthritis, temporal arteritis, and polymyalgia rheumatica.
- Trends and Progression: Changes in ESR levels over time can indicate disease progression or improvement.
- Temporal Arteritis Diagnosis: Elevated ESR is a key diagnostic criterion for temporal arteritis, a condition that affects blood vessels in the head.
- Interpretation: Increased ESR suggests the presence of inflammation or tissue damage. Higher rates of sedimentation may correlate with more active inflammation, but the ESR value alone does not provide specific diagnostic information.
Interpreting Together:
- Combining CRP and ESR measurements can provide a more comprehensive view of inflammation.
- Acute Infections: In acute infections, CRP rises rapidly, while ESR might also increase but more gradually.
- Chronic Inflammatory Diseases: For chronic conditions, both markers can indicate disease activity, with CRP often reflecting more immediate changes.
- Cardiovascular Risk: Elevated CRP levels in conjunction with other risk factors can contribute to assessing cardiovascular risk.
It’s crucial to remember that both CRP and ESR are nonspecific markers, indicating inflammation without pinpointing the exact cause. The clinical context, medical history, and other diagnostic tests are necessary for accurate interpretation and decision-making.
CRP and SED Rate in Disease Management
CRP (C-Reactive Protein) and ESR (Erythrocyte Sedimentation Rate) in Disease Management:
CRP:
- Role: Rapidly responds to inflammation, reflecting disease activity.
- Applications: Monitors infections, autoimmune disorders, and cardiovascular risk. Assesses treatment efficacy and disease progression.
- Clinical Use: Guides treatment decisions, predicts flare-ups, and evaluates response to therapy.
- Strength: Detects acute changes quickly, aiding timely intervention.
- Limitation: Nonspecific; elevated in various conditions.
- Example: Used to manage rheumatoid arthritis, track infections, and assess cardiovascular risk.
ESR:
- Role: Indicates presence of inflammation, but changes occur more slowly.
- Applications: Screens for general inflammation, monitors chronic conditions like arthritis and arteritis.
- Clinical Use: Assists in diagnosis, tracks disease progression, and evaluates response to treatment.
- Strength: Reflects long-term trends, helpful for chronic conditions.
- Limitation: Nonspecific; influenced by various factors beyond inflammation.
- Example: Employed in managing temporal arteritis, rheumatoid arthritis, and inflammatory diseases.
Combined Use:
- Complementary Information: CRP provides rapid changes, ESR reflects long-term trends.
- Comprehensive Assessment: Together, they offer a more complete picture of inflammation and disease activity.
- Clinical Decision-Making: Used alongside other clinical data for accurate management strategies.
While CRP and ESR are valuable tools in disease management, they are not diagnostic alone. They provide indications of inflammation that must be interpreted within the broader clinical context for effective disease management.
Factors Affecting CRP and SED Rate Levels
Factors Affecting CRP (C-Reactive Protein) and ESR (Erythrocyte Sedimentation Rate) Levels:
CRP:
- Inflammation: The primary factor influencing CRP levels is the presence and extent of inflammation in the body.
- Infection Type: Bacterial infections often lead to higher CRP levels than viral infections.
- Disease Severity: More severe inflammation or disease activity is associated with higher CRP levels.
- Autoimmune Disorders: Conditions like rheumatoid arthritis, lupus, and inflammatory bowel diseases can elevate CRP.
- Tissue Injury: Trauma, surgery, and tissue damage can result in elevated CRP levels.
- Medications: Some medications, like corticosteroids, can influence CRP levels.
- Cardiovascular Risk: CRP is used to assess cardiovascular risk; factors like obesity and smoking can affect levels.
ESR:
- Inflammation: Like CRP, the primary influence on ESR is the presence of inflammation.
- Aging: ESR tends to increase with age due to changes in blood composition.
- Gender: Women often have slightly higher ESR levels compared to men.
- Anemia: Low red blood cell count can lead to elevated ESR levels.
- Pregnancy: ESR increases during pregnancy due to changes in blood composition.
- Certain Diseases: Conditions like multiple myeloma and temporal arteritis can substantially elevate ESR.
- Medications: Certain drugs can impact ESR levels, such as oral contraceptives and nonsteroidal anti-inflammatory drugs.
Common Considerations:
- Non-Specificity: Both markers are nonspecific, meaning various factors can influence their levels.
- Baseline Variation: Individual baseline levels can vary; changes from an individual’s baseline are often more indicative.
- Clinical Context: Interpretation must consider the patient’s medical history, overall health, and other diagnostic information.
When interpreting CRP and ESR levels, it’s essential to consider these factors to accurately assess the degree of inflammation and its underlying cause.
Importance of Regular Monitoring

Importance of Regular Monitoring in Disease Management:
Regular monitoring of health markers, including C-Reactive Protein (CRP) and Erythrocyte Sedimentation Rate (ESR), plays a pivotal role in effective disease management. Here’s why it’s crucial:
- Early Detection: Regular monitoring allows for the early detection of changes in inflammation levels. This is particularly important in identifying disease flare-ups, complications, or treatment inefficacies before they become severe.
- Treatment Adjustment: Monitoring provides insights into how well treatments are working. If CRP or ESR levels indicate persistent or worsening inflammation, healthcare providers can adjust treatment plans promptly to optimize outcomes.
- Disease Progression: Tracking changes over time helps healthcare professionals understand the trajectory of a disease. Monitoring disease progression aids in making informed decisions about adjusting medications, therapies, and lifestyle modifications.
- Customized Care: Regular monitoring enables personalized care plans. Healthcare providers can tailor treatments based on individual responses, optimizing the management of chronic conditions.
- Preventive Measures: For individuals at risk of specific conditions, regular monitoring helps identify early warning signs, facilitating preventive interventions and lifestyle adjustments.
- Objective Data: Monitoring provides objective data to support medical decisions. It eliminates guesswork and ensures that treatment plans are based on quantifiable changes.
- Patient Engagement: Patients who actively participate in their health management are more likely to follow prescribed treatments. Regular monitoring empowers patients to take charge of their health.
- Quality of Life: Effective disease management enhances quality of life. Regular monitoring can help minimize symptoms, reduce disease impact, and improve overall well-being.
- Clinical Trials: In research settings, regular monitoring ensures that participants are responding as expected to experimental treatments, contributing to accurate trial outcomes.
- Preventing Complications: Monitoring aids in catching potential complications early, preventing hospitalizations and more aggressive interventions.
Regular monitoring of CRP, ESR, and other relevant health markers provides valuable data for healthcare providers and patients alike. It empowers informed decision-making, supports proactive interventions, and contributes to improved health outcomes.
Conclusion
Regular monitoring of markers like C-Reactive Protein (CRP) and Erythrocyte Sedimentation Rate (ESR) is integral to effective disease management. This proactive approach enables early detection of changes, facilitates timely treatment adjustments, and provides valuable insights into disease progression. With personalized care plans, objective data, and improved patient engagement, regular monitoring plays a pivotal role in optimizing health outcomes and enhancing overall quality of life.



