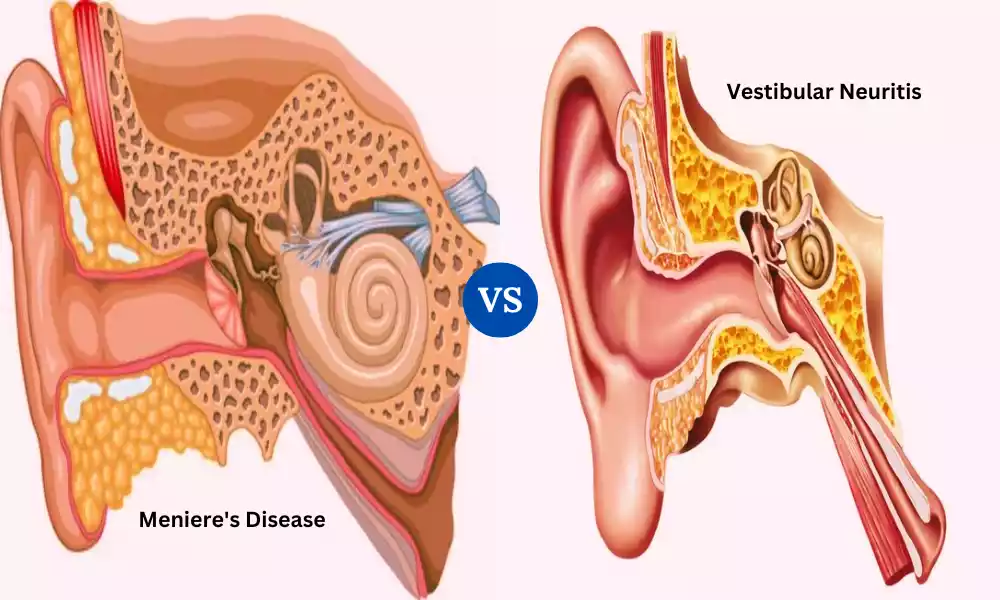
Meniere’s Disease and Vestibular Neuritis emerge as significant challenges impacting individuals’ balance and well-being. These conditions, characterized by vertigo and dizziness, can have a profound effect on daily life. Delves into the differences between these two disorders, exploring their causes, symptoms, diagnosis, and management strategies. Whether you’re seeking insights into your own condition or looking to expand your knowledge, Aims provides a comprehensive understanding of Meniere’s Disease and Vestibular Neuritis.
What is Meniere’s Disease?
Meniere’s Disease is a complex and chronic inner ear disorder that profoundly impacts balance and hearing. It is characterized by recurrent episodes of vertigo, an intense sensation of spinning accompanied by nausea and imbalance. These episodes can be disabling and last anywhere from minutes to hours. Tinnitus, a persistent ringing or buzzing sound in the ears, is another hallmark symptom.
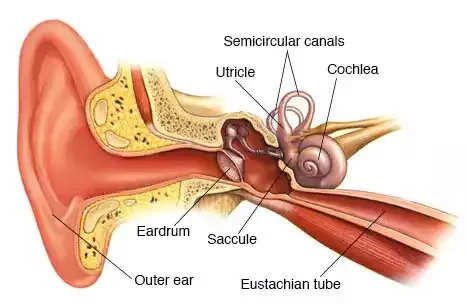
Fluctuating hearing loss, often starting in one ear but potentially affecting both, is a common feature as well. This hearing loss can worsen over time and may be accompanied by a feeling of fullness in the affected ear. The exact cause of Meniere’s Disease remains unclear, but it’s thought to involve an abnormal buildup of fluid in the inner ear’s delicate balance and hearing structures.
While there is no cure, various treatments, including medications, dietary changes, and therapeutic interventions, aim to manage symptoms and improve quality of life for those affected by this condition.
Symptoms of Meniere’s Disease
Meniere’s Disease is characterized by a combination of symptoms that can vary in intensity and duration. The primary symptoms include:
- Vertigo: Sudden and severe episodes of vertigo, a sensation of spinning or whirling. Vertigo attacks can be incapacitating and lead to nausea, vomiting, and a loss of balance. These episodes can last from minutes to hours and often come without warning.
- Tinnitus: Persistent ringing, buzzing, hissing, or other noises in the ears. Tinnitus can be continuous or intermittent and is often described as bothersome and distracting.
- Fluctuating Hearing Loss: Individuals with Meniere’s Disease may experience fluctuations in their hearing abilities. This typically affects one ear initially, but it can eventually impact both ears. Hearing loss can range from mild to severe and may worsen during or after vertigo attacks.
- Aural Fullness: Many people with Meniere’s Disease report a sensation of fullness, pressure, or congestion in the affected ear. This feeling is often likened to having a plugged ear.
The combination of these symptoms is unique to Meniere’s Disease. The exact cause of the condition is still not fully understood, but it’s believed to be related to issues with fluid regulation in the inner ear. It’s important to seek medical evaluation if you experience these symptoms, as they can be similar to those of other conditions, and proper diagnosis is crucial for effective management.
Impact of Meniere’s Disease
Meniere’s Disease can have a significant impact on various aspects of an individual’s life due to its unpredictable and disruptive nature. The symptoms of Meniere’s Disease, including vertigo, tinnitus, fluctuating hearing loss, and aural fullness, can lead to several challenges:
- Quality of Life: The sudden and intense vertigo attacks can severely limit a person’s ability to engage in daily activities, work, and social interactions. The fear of experiencing vertigo can lead to anxiety and a reduced overall quality of life.
- Physical Functioning: Vertigo can be debilitating, causing dizziness, nausea, and difficulty maintaining balance. This can make it dangerous to perform tasks such as driving, operating machinery, or even walking, leading to limitations in physical activities.
- Emotional Well-being: The chronic and unpredictable nature of Meniere’s Disease can result in emotional distress. Anxiety, depression, and frustration are common responses to the uncertainty of when vertigo attacks might occur.
- Communication Difficulties: Fluctuating hearing loss and tinnitus can make it challenging to communicate effectively, both in personal and professional settings. This can lead to misunderstandings, isolation, and reduced participation in social activities.
- Occupational Impact: The symptoms of Meniere’s Disease can affect work performance and attendance. The unpredictability of vertigo episodes might make it difficult to maintain regular work schedules, potentially leading to career adjustments or changes.
- Social Interactions: Participating in social gatherings or events can be complicated by the fear of sudden vertigo attacks. Tinnitus and hearing difficulties might make conversations challenging and affect relationships.
- Coping Strategies: Individuals with Meniere’s Disease often need to develop coping strategies to manage their symptoms. This might involve avoiding triggers, making lifestyle changes, and seeking medical interventions.
- Treatment and Management: Managing Meniere’s Disease usually requires a combination of medications, dietary adjustments, and sometimes surgical interventions. These treatments can bring their own challenges and side effects.
It’s important for individuals with Meniere’s Disease to work closely with medical professionals to develop a comprehensive management plan. Support from healthcare providers, counseling, support groups, and the development of coping strategies can help individuals navigate the physical and emotional challenges posed by this condition.
Underlying Causes
The exact underlying causes of Meniere’s Disease are not fully understood, but it’s believed to be linked to several factors involving the inner ear’s fluid balance and sensory mechanisms. Some proposed factors include:
- Endolymphatic Hydrops: This is a key theory in Meniere’s Disease. It involves abnormal accumulation of fluid (endolymph) in the inner ear’s labyrinth, which disrupts the ear’s normal balance and hearing functions.
- Vascular Abnormalities: Some researchers suggest that issues with blood flow and vascular regulation in the inner ear might contribute to Meniere’s Disease.
- Autoimmune Factors: Immune responses targeting the inner ear structures could trigger inflammation and fluid imbalance.
- Genetic Predisposition: There might be a genetic component that increases susceptibility to Meniere’s Disease, as it sometimes runs in families.
- Viral Infections: Viral infections affecting the inner ear, like certain types of herpes viruses, have been proposed as potential triggers.
- Anatomical Abnormalities: Structural issues within the inner ear or abnormalities in the way certain parts of the ear develop could play a role.
It’s important to note that Meniere’s Disease is likely to result from a combination of these factors, and each individual’s experience can vary. Research is ongoing to better understand the precise mechanisms driving the condition.
What is Vestibular Neuritis?
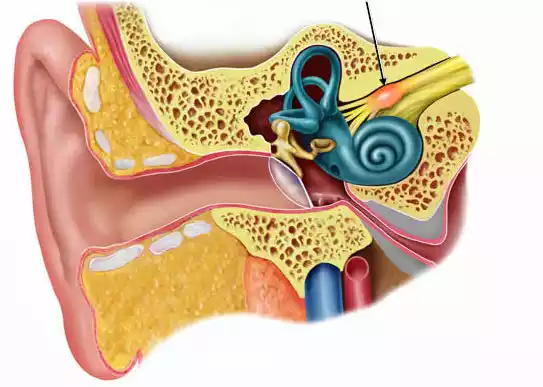
Vestibular Neuritis, also known as acute vestibular neuritis or vestibular neuronitis, is a disorder of the inner ear that causes sudden and severe vertigo, often accompanied by nausea, vomiting, and difficulty maintaining balance. This condition is primarily attributed to inflammation of the vestibular nerve, which connects the inner ear to the brain and is responsible for transmitting signals related to balance and spatial orientation.
The hallmark symptom of vestibular neuritis is the sudden onset of intense vertigo, which can leave individuals feeling as though their surroundings are spinning. This sensation is typically not associated with hearing loss or tinnitus, distinguishing it from other inner ear disorders. The exact cause of vestibular neuritis is often linked to viral infections, particularly those affecting the inner ear. These infections can lead to inflammation and disruption of the delicate balance mechanisms within the vestibular system.
Vestibular neuritis can have a significant impact on a person’s daily life, as the severe vertigo episodes can cause disorientation and hinder routine activities. While the acute symptoms often improve over time as the body’s inflammation subsides, the residual balance issues might persist, necessitating medical intervention and vestibular rehabilitation to aid in recovery.
Identifying Symptoms
Identifying symptoms of Vestibular Neuritis is crucial for proper diagnosis and management. The primary symptoms of this condition include:
- Sudden Vertigo: The hallmark symptom is the sudden onset of intense vertigo, a sensation of spinning or whirling. Vertigo can be severe and incapacitating, often accompanied by nausea, vomiting, and difficulty maintaining balance.
- Nystagmus: Individuals with vestibular neuritis might experience nystagmus, which is an involuntary rhythmic movement of the eyes. Nystagmus can occur when the brain attempts to compensate for the disrupted signals from the affected inner ear.
- Unilateral Vestibular Loss: Unlike some other balance disorders, vestibular neuritis typically affects only one ear. This leads to a sensation of imbalance and unsteadiness on one side.
- Absence of Hearing Loss: One distinguishing feature of vestibular neuritis is that it primarily affects the balance and vestibular functions of the inner ear, without causing significant hearing loss or tinnitus. This sets it apart from conditions like Meniere’s Disease.
- Postural Instability: Even after the acute vertigo subsides, individuals may experience ongoing difficulties with balance, especially during movements like walking or changing positions.
- Visual Disturbances: Visual symptoms such as blurred vision or difficulty focusing may accompany vertigo episodes, contributing to the overall sense of disorientation.
It’s important to seek medical attention if you experience these symptoms, as they can also be indicative of other conditions. A healthcare professional will perform a thorough evaluation, which may include a medical history review, physical examination, and possibly specialized tests such as the Dix-Hallpike maneuver or electronystagmography (ENG) to assess eye movements and vestibular function.
Accurate diagnosis enables appropriate treatment strategies, which may involve medications for symptom relief, vestibular rehabilitation therapy, and addressing the underlying inflammation.
Unveiling the Causes
Here are the potential causes of Vestibular Neuritis presented:
- Inflammation of Vestibular Nerve: The primary cause of Vestibular Neuritis is inflammation of the vestibular nerve, disrupting its signals to the brain that are crucial for balance and spatial orientation.
- Viral Infections: Viral infections, particularly by viruses like herpes simplex or varicella-zoster, are believed to trigger Vestibular Neuritis. These infections can lead to inflammation in the inner ear, affecting the nerve’s function.
- Immune Response: Viral infections can prompt the immune system to respond, causing inflammation not only in the inner ear but also in the vestibular nerve, contributing to the vertigo and dizziness.
- Disrupted Signal Transmission: Inflammation interferes with the normal transmission of sensory information from the inner ear to the brain, leading to the sudden and intense vertigo associated with Vestibular Neuritis.
- Vascular Factors: Some research suggests that issues with blood flow to the inner ear might play a role, impacting the nerve’s function and leading to symptoms.
- Autoimmune Factors: Autoimmune reactions that mistakenly target the inner ear structures could also contribute to inflammation and nerve dysfunction.
- Individual Susceptibility: Not everyone who experiences a viral infection develops Vestibular Neuritis. An individual’s immune response, overall health, and genetic factors likely determine susceptibility.
Understanding these potential causes is essential for diagnosing and managing Vestibular Neuritis effectively.
Comparing Table of Meniere’s Disease and Vestibular Neuritis
Here’s a comparative table outlining the differences between Meniere’s Disease and Vestibular Neuritis:
| Aspect | Meniere’s Disease | Vestibular Neuritis |
|---|---|---|
| Primary Symptoms | – Vertigo
– Tinnitus – Fluctuating hearing loss – Aural fullness/pressure |
– Sudden vertigo
– Nausea and vomiting – Unilateral vestibular loss – No hearing loss or tinnitus |
| Underlying Cause | – Fluid buildup in inner ear (endolymphatic hydrops)
– Genetic predisposition (possible) |
– Viral infection affecting vestibular nerve and inner ear structures
– Immune response and inflammation |
| Hearing Involvement | – Fluctuating hearing loss common
– Tinnitus present |
– Typically no significant hearing loss
– No tinnitus |
| Duration of Episodes | – Vertigo episodes can last minutes to hours | – Acute vertigo episodes during onset, lasting days to weeks |
| Triggers | – Stress, dietary factors, fatigue, etc. | – Often follows a viral infection or illness |
| Medical Evaluation | – Diagnosis based on symptoms, hearing tests, balance tests, imaging | – Diagnosis based on symptoms, clinical evaluation, balance tests, eye movement tests |
| Treatment Approach | – Medications for symptom relief
– Dietary changes – Lifestyle adjustments |
– Medications for symptom relief
– Vestibular rehabilitation therapy – Addressing inflammation |
| Long-Term Effects | – Can lead to progressive hearing loss over time | – Vertigo symptoms often improve over time, but residual balance issues can persist |
| Relation to Ear | – Affects one or both ears | – Primarily affects one ear |
This table provides a general comparison between Meniere’s Disease and Vestibular Neuritis, highlighting key differences in their symptoms, causes, and characteristics. Individual experiences can vary, and a medical professional’s evaluation is essential for accurate diagnosis and treatment.
Diagnosis of Meniere’s Disease and Vestibular Neuritis

Diagnosing both Meniere’s Disease and Vestibular Neuritis involves a combination of medical evaluation, symptom assessment, and specialized tests. Navigating the diagnostic journey for these conditions can be essential for effective management. Here’s an overview of the diagnostic process for each:
Meniere’s Disease:
- Medical History: The doctor will start by gathering information about your symptoms, their frequency, and any triggers you’ve noticed.
- Physical Examination: A physical examination, including assessing your ear and neurological function, can provide important clues.
- Audiometric Tests: Hearing tests, such as audiometry, help measure the extent of hearing loss and its characteristics.
- Balance and Vestibular Tests: Tests like electronystagmography (ENG) or videonystagmography (VNG) evaluate eye movements to assess inner ear and balance function.
- Imaging: Imaging tests like magnetic resonance imaging (MRI) can rule out other potential causes of symptoms.
- Diagnosis: Diagnosis is often made based on specific criteria involving recurrent vertigo, hearing loss, tinnitus, and aural fullness.
Vestibular Neuritis:
- Clinical Assessment: The doctor will take a detailed history of your symptoms, their onset, and any recent illnesses.
- Physical Examination: A physical exam may reveal signs of vestibular dysfunction or nystagmus.
- Balance Tests: Specialized tests like the Dix-Hallpike maneuver can provoke characteristic eye movements associated with vestibular neuritis.
- Auditory and Vestibular Testing: These tests can help differentiate between vestibular neuritis and conditions affecting hearing.
- Viral Testing: In some cases, testing for viral infections might be considered if recent illnesses are suspected triggers.
- Diagnosis: A diagnosis is often made based on the sudden onset of severe vertigo, with absence of significant hearing loss or tinnitus, and the exclusion of other potential causes.
Navigating the diagnostic journey involves effective communication with medical professionals, providing a detailed medical history, and describing your symptoms accurately. Collaboration with an ear, nose, and throat (ENT) specialist or a neurologist who specializes in balance disorders is crucial. The diagnostic process helps ensure proper understanding of the underlying condition, allowing for targeted treatment and management strategies.
Treatment Approaches Regaining Balance
Meniere’s Disease and Vestibular Neuritis can impact balance and quality of life, but they have different treatment approaches. Here’s an overview of how each condition is managed to help individuals regain their balance:
Meniere’s Disease:
- Dietary Changes: Reducing salt intake can help manage fluid buildup in the inner ear, potentially reducing the frequency and severity of vertigo attacks.
- Medications: Prescription medications like diuretics, anti-nausea drugs, and vestibular suppressants can alleviate symptoms during vertigo episodes.
- Lifestyle Modifications: Stress management techniques, getting enough rest, and avoiding triggers like caffeine and alcohol can help reduce symptom severity.
- Vestibular Rehabilitation Therapy: This involves specific exercises and maneuvers to improve balance and reduce the impact of vertigo. It’s often supervised by a physical therapist.
- Surgery: Surgical options might be considered if symptoms are severe and not responding to other treatments. These include procedures like endolymphatic sac decompression or vestibular nerve section.
Vestibular Neuritis:
- Medications: Medications like anti-nausea drugs and sometimes short-term steroids can help manage symptoms during the acute phase.
- Vestibular Rehabilitation Therapy: This is a key treatment, involving exercises to help the brain compensate for the disrupted signals from the affected vestibular nerve.
- Supportive Care: Rest during the acute phase is important. Gradually increasing activity levels as symptoms improve can aid in recovery.
- Treatment of Underlying Infection: If a viral infection triggered the condition, addressing the infection might play a role in management.
- Monitoring: Continuous evaluation of symptoms and progress is important to tailor treatment approaches.
Both conditions require a multidisciplinary approach involving medical professionals such as ear specialists, physical therapists, and sometimes psychologists for addressing the emotional impact. Partnership between medical practitioners is critical in designing an individualized treatment strategy. While there’s no cure for either condition, effective management can greatly improve symptoms and overall quality of life.
Lifestyle Modifications
Lifestyle modifications play a significant role in managing both Meniere’s Disease and Vestibular Neuritis. These adjustments can help reduce the frequency and severity of symptoms, improve balance, and enhance overall well-being.
Here are some lifestyle modifications that individuals with these conditions might consider:
For Meniere’s Disease:
- Dietary Changes: Reduce salt intake to help minimize fluid retention in the inner ear, which can trigger vertigo. Avoiding caffeine and alcohol might also be beneficial.
- Stress Management: Stress can exacerbate symptoms, so practicing relaxation techniques such as deep breathing, meditation, or yoga can be helpful.
- Hydration: Staying properly hydrated can help maintain fluid balance in the body.
- Regular Sleep: Adequate sleep is crucial for overall health and stress reduction.
- Trigger Identification: Keep track of activities or situations that trigger vertigo or worsen symptoms, and try to avoid them.
- Physical Activity: Engage in regular physical activity, within your comfort limits, to improve overall well-being and maintain a healthy weight.
- Hearing Protection: Protect your ears from loud noises to prevent potential exacerbation of symptoms.
For Vestibular Neuritis:
- Rest and Gradual Activity: During the acute phase, rest is important to allow the body to recover. Increase levels of activity as symptoms improve.
- Vestibular Rehabilitation Exercises: These exercises, prescribed by a physical therapist, help the brain adapt to the vestibular imbalance and improve balance.
- Avoid Rapid Movements: Quick head movements can trigger dizziness, so try to move slowly and deliberately.
- Positional Awareness: Be mindful of your head position, especially when lying down or changing positions.
- Hydration and Nutrition: Maintain a balanced diet and proper hydration to support overall health.
- Medication Adherence: Those prescribed medication must follow their physician’s orders carefully.
- Environmental Modifications: Make your living space safe and comfortable to reduce the risk of falls.
Remember that these lifestyle modifications are general guidelines. The impact of specific changes can vary from person to person. Consulting with healthcare professionals, including ENT specialists, physical therapists, and nutritionists, is crucial for developing a tailored plan that suits your individual needs and goals. Regular communication with your healthcare team helps ensure effective symptom management and improved quality of life.
Strategies for Dealing with Challenges
Coping with the challenges posed by Meniere’s Disease and Vestibular Neuritis requires a combination of physical, emotional, and practical strategies. Here are some strategies that can help individuals effectively deal with the challenges of these conditions:
For Meniere’s Disease:
- Educate Yourself: Understanding the condition and its triggers empowers you to make informed decisions about lifestyle adjustments and treatment options.
- Symptom Tracking: Keep a journal to record symptom patterns, triggers, and the effectiveness of different strategies. This can help you identify trends and make informed choices.
- Stress Reduction: Practice stress management techniques such as meditation, deep breathing, or mindfulness to help reduce the impact of stress on symptoms.
- Support System: Connect with support groups or online communities where you can share experiences, get advice, and find emotional support.
- Communication: Inform friends, family, and coworkers about your condition, so they can offer understanding and support.
- Safety Measures: Make your environment safer to prevent falls during vertigo episodes. Use handrails, non-slip rugs, and keep pathways clear.
For Vestibular Neuritis:
- Rest and Gradual Activity: During acute phases, prioritize rest and gradually reintroduce physical activity as symptoms improve.
- Vestibular Rehabilitation: Engage in prescribed exercises to help the brain adapt to vestibular imbalances and enhance balance.
- Positional Awareness: Be mindful of head positions and movements that trigger dizziness. Slow and deliberate movements can help prevent sudden vertigo.
- Patience: Understand that recovery can take time. Be kind to yourself and grant your body time to recover.
- Positive Mindset: Focus on the progress you’re making, no matter how small. Celebrate each step towards improvement.
- Seek Professional Guidance: Consult with medical professionals to adjust treatment plans, address concerns, and receive personalized advice.
- Visual and Auditory Cues: In environments with visual cues (like contrasting floor patterns) and auditory cues (like consistent background noise), your balance might improve.
Remember that everyone’s experience is unique, so finding strategies that work for you may involve trial and error. A multidisciplinary approach involving healthcare professionals, physical therapists, and mental health experts can help you navigate the challenges and improve your overall well-being. Regular communication with your medical team is key to adjusting strategies as your condition evolves.
Research and Advancements
Research and advancements in the field of Meniere’s Disease and Vestibular Neuritis are ongoing, aiming to improve understanding, diagnosis, and treatment. Here’s a brief overview:
Meniere’s Disease:
- Genetic Studies: Research is exploring genetic factors that might contribute to Meniere’s Disease, potentially leading to more targeted treatments.
- Biological Mechanisms: Advances in understanding the inner ear’s fluid balance and cellular functions could provide insights into the condition’s underlying causes.
- Treatment Innovation: Ongoing studies are investigating new medications, therapies, and surgical interventions to alleviate symptoms and improve quality of life.
Vestibular Neuritis:
- Viral Triggers: Research is delving into specific viral infections that might trigger vestibular neuritis, aiding in identifying risk factors and preventive measures.
- Vestibular Rehabilitation: Studies are refining and expanding vestibular rehabilitation techniques to optimize recovery and balance improvement.
- Diagnostic Tools: Advancements in diagnostic tools, such as improved imaging techniques, can aid in more accurate and early diagnosis.
- Personalized Treatment: The field is moving towards tailoring treatment plans to individual needs, taking into account factors like genetics and symptom patterns.
- Neuroplasticity: Understanding the brain’s ability to adapt and compensate for vestibular imbalances is shaping innovative rehabilitation strategies.
Remember that research is an ongoing process, and new discoveries are continually being made. Staying informed through reputable medical sources and discussions with healthcare professionals can help individuals benefit from these advancements as they become available.
Final Opinion
Meniere’s Disease and Vestibular Neuritis stand as challenges that require careful management and understanding. While they share some symptoms, their underlying causes and treatment approaches differ significantly. By seeking early diagnosis, adopting lifestyle modifications, and staying informed about advancements, individuals can navigate these disorders with resilience and a higher quality of life.