Dysphagia and Odynophagia: Swallowing is a fundamental and often taken-for-granted function of the human body. For individuals suffering from dysphagia and odynophagia, the simple act of swallowing can become a challenging and painful ordeal. We’ll delve into these two conditions, exploring their causes, symptoms, diagnosis, and treatment options.
What is Dysphagia?
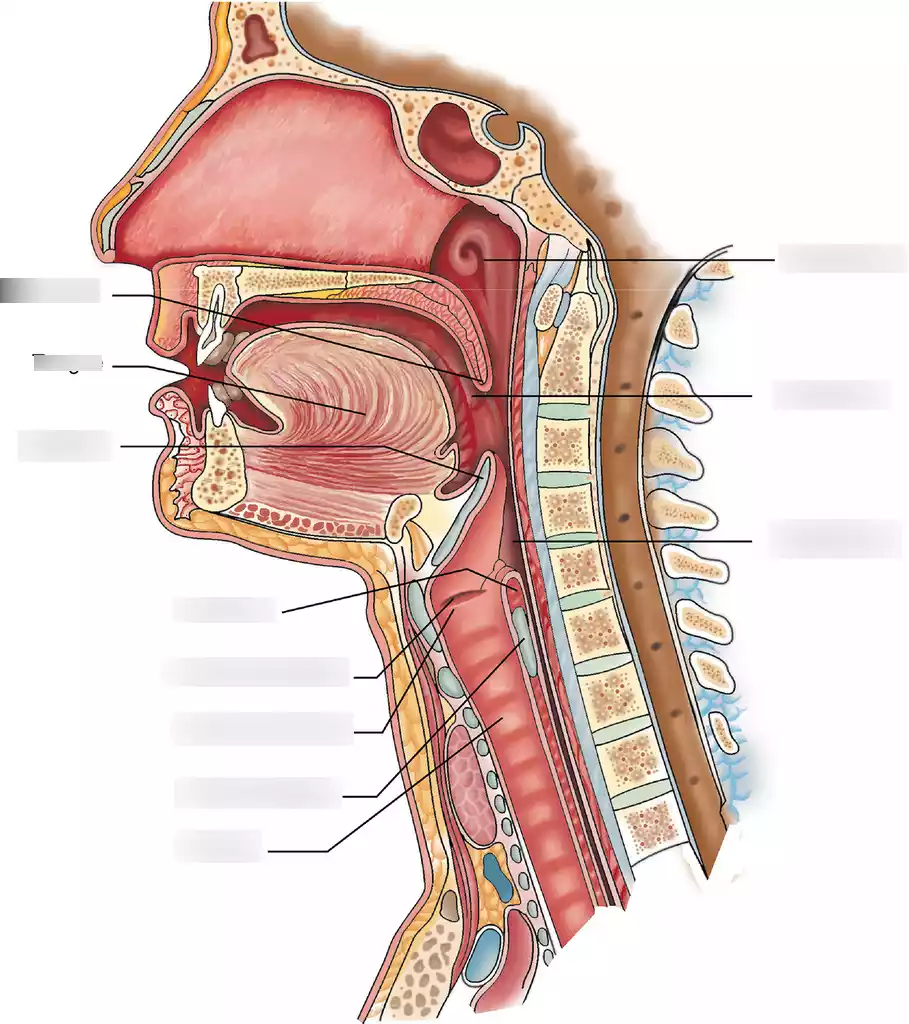
Dysphagia is a medical condition that pertains to difficulties in swallowing, affecting the ability to move food and liquids from the mouth to the stomach. This condition can significantly disrupt an individual’s ability to eat and drink comfortably. There are two primary types of dysphagia: oropharyngeal dysphagia and esophageal dysphagia.
Oropharyngeal dysphagia refers to problems encountered in the oral and pharyngeal phases of swallowing. These issues are often related to difficulties in chewing, manipulating food in the mouth, or coordinating the muscles and movements required to transport food from the mouth to the throat.
Esophageal dysphagia is associated with challenges in the esophagus, the muscular tube that carries food from the throat to the stomach. These difficulties can arise due to structural abnormalities, muscle disorders, or other issues that hinder the smooth passage of food through the esophagus.
Dysphagia can have various causes, including neurological conditions like stroke or Parkinson’s disease, structural abnormalities in the throat or esophagus, muscle weakness, or radiation therapy side effects. Symptoms of dysphagia can include choking, coughing, regurgitation, and a sensation of food getting stuck in the throat.
Diagnosis typically involves a comprehensive assessment, which may include medical history, physical examinations, imaging studies, and endoscopic procedures. Treatment options depend on the underlying cause and may encompass dietary modifications, swallowing exercises, medications, or surgical interventions. Early diagnosis and appropriate management are vital to improving an individual’s ability to eat and drink safely and comfortably while preventing complications.
Types of Dysphagia
Dysphagia, or difficulty swallowing, can be categorized into two main types:
- Oropharyngeal Dysphagia: This type involves difficulties in the oral and pharyngeal phases of swallowing. It often relates to problems with chewing, moving food around in the mouth, or coordinating the muscles needed to transport food to the throat.
- Esophageal Dysphagia: Esophageal dysphagia is associated with issues in the esophagus, the muscular tube that carries food from the throat to the stomach. It can result from structural abnormalities, muscle disorders, or other factors that impede the smooth passage of food through the esophagus.
These categories help in diagnosing and treating dysphagia effectively, as the causes and management strategies may differ based on the type of dysphagia a person experiences.
Causes of Dysphagia
Causes of dysphagia, or difficulty swallowing, can vary and include:
- Neurological Conditions: Such as stroke, Parkinson’s disease, or ALS, which affect nerve control of swallowing.
- Structural Abnormalities: Such as narrowing of the esophagus (strictures), tumors, or gastroesophageal reflux disease (GERD).
- Muscle Weakness: Conditions like muscular dystrophy or myasthenia gravis can weaken the muscles involved in swallowing.
- Medications: Some drugs may cause dry mouth or throat muscle problems leading to dysphagia.
- Infections: Conditions like thrush or esophagitis can lead to painful swallowing.
- Radiation Therapy: For head and neck cancers can damage the throat.
- Aging: Natural age-related changes in swallowing function can contribute to dysphagia.
Identifying the specific cause is crucial for effective treatment.
Symptoms of Dysphagia
Symptoms of dysphagia (difficulty swallowing) can include:
- Coughing or choking can occur while eating or after drinking beverages.
- Pain or discomfort while swallowing (odynophagia).
- Food becomes lodged in your chest or throat and causes discomfort.
- Regurgitation of undigested food.
- Frequent heartburn or gastroesophageal reflux.
- Unexplained weight loss due to difficulty eating.
- Change in voice or hoarseness after eating.
- Persistent sore throat.
- Drooling or difficulty managing saliva.
- Recurrent pneumonia or respiratory infections due to food or liquid entering the airway.
These symptoms can vary in severity and may indicate different underlying causes of dysphagia, making prompt evaluation by a healthcare professional important for diagnosis and treatment.
Diagnosis and Assessment of Dysphagia
Diagnosis and assessment of dysphagia (difficulty swallowing) involve:
- Medical History: Discussing medical conditions, symptoms and medications used for their treatment is vitally important.
- Physical Examination: Evaluating the mouth, throat, and neck for abnormalities.
- Imaging: Using tests like a barium swallow or endoscopy to visualize the swallowing process.
- Manometry: Measuring pressure and muscle function in the esophagus.
- Speech and Language Assessment: Evaluating speech and swallowing function.
- Blood Tests: To identify underlying conditions.
- Biopsy: If abnormalities or tumors are suspected.
The specific tests used depend on the suspected cause of dysphagia, aiding in accurate diagnosis and tailored treatment plans.
Treatment for Dysphagia
Treatment for dysphagia (difficulty swallowing) varies based on its type and underlying cause:
- Oropharyngeal Dysphagia: Often includes dietary modifications (changing food consistency), swallowing therapy with a speech therapist, and sometimes medications.
- Esophageal Dysphagia: Treatment may involve dilation to widen the esophagus, medications to address underlying issues like acid reflux, lifestyle changes, or, in severe cases, surgery.
Treatment aims to improve swallowing function, reduce discomfort, and manage the underlying condition. Consultation with a physician is integral to creating a tailored treatment program.
What is Odynophagia?

Odynophagia is the medical term for any experience of pain or discomfort caused by swallowing. Unlike dysphagia, which refers to difficulty swallowing, odynophagia specifically highlights the painful aspect of the swallowing process. This discomfort or pain can occur at any point during swallowing, from the mouth down to the esophagus. Odynophagia is often indicative of an underlying issue or condition that requires medical attention.
There are various potential causes of odynophagia, ranging from relatively minor issues like mild infections (e.g., strep throat or thrush) to more serious conditions such as gastroesophageal reflux disease (GERD), esophagitis, or even esophageal ulcers.
Additionally, structural abnormalities or injuries within the throat or esophagus can lead to odynophagia. Determining the exact cause is crucial for appropriate treatment, as the underlying condition needs to be addressed to relieve the pain during swallowing.
Diagnosis of odynophagia typically involves a comprehensive evaluation by a healthcare provider, including a medical history review, physical examination, and potentially imaging tests or endoscopic procedures.
Treatment options vary based on the specific cause and can include medications to treat infections or reduce inflammation, dietary modifications to minimize irritation, and in some cases, interventions to address structural issues. Prompt diagnosis and management are essential to alleviate discomfort and prevent complications associated with odynophagia.
Types of Odynophagia
Types of Odynophagia include:
- Infectious Odynophagia: Painful swallowing due to infections like strep throat or oral thrush.
- Inflammatory Odynophagia: Painful swallowing caused by inflammation, often related to conditions like GERD.
- Structural Odynophagia: Results from structural issues like strictures, ulcers, or tumors in the throat or esophagus.
- Chemical Odynophagia: Occurs when corrosive substances damage the esophagus, often due to accidental ingestion.
- Medication-Induced Odynophagia: Some medications can cause irritation or injury to the throat or esophagus.
- Allergic Odynophagia: Rare, caused by allergies to certain foods or substances, leading to discomfort during swallowing.
Causes of Odynophagia
Odynophagia, or painful swallowing, can be caused by various factors, including:
- Infections: Such as strep throat, thrush (oral yeast infection), or viral pharyngitis.
- Inflammation: Conditions like esophagitis, often associated with gastroesophageal reflux disease (GERD).
- Structural Abnormalities: Including esophageal strictures or ulcers.
- Chemical Irritation: From ingesting corrosive substances.
- Medications: Some medications can cause irritation or damage to the esophagus.
Identifying the specific cause of odynophagia is essential for targeted treatment and relief from the discomfort during swallowing.
Symptoms of Odynophagia
Symptoms of odynophagia (painful swallowing) include:
- Sharp or burning pain while swallowing.
- Discomfort or irritation in the throat or chest when eating or drinking.
- Avoidance of certain foods due to pain during swallowing.
- Coughing or gagging in response to pain.
- Regurgitation of partially swallowed food or liquid.
- Weight loss due to reduced food intake.
- Voice changes or hoarseness after swallowing.
Experiencing these symptoms, especially if they persist, warrants prompt medical evaluation to identify the underlying cause and initiate appropriate treatment.
Diagnosis and Assessment of Odynophagia
Diagnosis and assessment of odynophagia (painful swallowing) typically involve:
- Medical History: Discussing symptoms, their onset, and any relevant medical conditions or recent illnesses.
- Physical Examination: Examining the throat, mouth, and neck for signs of infection, inflammation, or structural issues.
- Imaging: Using tests like endoscopy or barium swallow to visualize the esophagus and identify abnormalities.
- Swabs or Biopsy: Collecting samples to test for infections or abnormal tissue.
- Allergy or Sensitivity Tests: To rule out allergies as a cause.
- Review of Medications: Assessing whether any medications may be contributing to the symptoms.
The diagnostic process helps pinpoint the specific cause of odynophagia, enabling healthcare providers to recommend targeted treatment options for pain relief and addressing the underlying issue.
Treatment for Odynophagia
Treatment for odynophagia (painful swallowing) depends on the underlying cause:
- Infections: Typically treated with antibiotics or antifungal medications.
- Inflammation: Managed with medications to reduce inflammation, such as proton pump inhibitors (PPIs) for GERD-related odynophagia.
- Structural Issues: May require interventions like dilation for strictures or surgical procedures for ulcers or tumors.
- Chemical Irritation: Focuses on symptom relief and managing complications, often involving a healthcare provider.
- Medication-Induced Odynophagia: Involves discontinuing or replacing the offending medication, under medical supervision.
Effective treatment aims to relieve pain, address the underlying cause, and improve the ability to swallow comfortably. An appointment with a physician can ensure accurate diagnosis and treatment plans are put in place.
Comparative table between Dysphagia and Odynophagia
Here’s a comparative table highlighting the key differences between Dysphagia and Odynophagia:
| Aspect | Dysphagia | Odynophagia |
|---|---|---|
| Definition | Difficulty in swallowing | Painful swallowing |
| Primary Symptom | Choking, coughing, food sticking | Sharp or burning pain during swallowing |
| Types | Oropharyngeal (oral and throat phases) and Esophageal (esophagus-related) | Typically related to various causes of throat or esophageal pain |
| Underlying Causes | Neurological conditions, structural abnormalities, muscle weakness, medical treatments | Infections, inflammation, structural issues, chemical irritation, medications |
| Diagnosis | Medical history, physical examination, imaging (e.g., barium swallow), endoscopic procedures | Medical history, physical examination, imaging, swabs or biopsy, medication review |
| Treatment | Depends on type and cause; may include dietary modifications, swallowing therapy, medications, dilation, surgery | Depends on the underlying cause; can involve antibiotics, anti-inflammatory drugs, dilation, discontinuing offending medications |
| Complications if Untreated | Aspiration pneumonia, malnutrition, dehydration, reduced quality of life | Risk of worsening underlying condition, weight loss, nutritional deficiencies, reduced quality of life |
| Primary Concern | Difficulty in safely consuming food and liquids | Pain and discomfort while swallowing |
Remember that both dysphagia and odynophagia can be symptoms of various underlying conditions, and proper diagnosis and treatment are essential to address the specific cause and alleviate these symptoms.
Conclusion
Dysphagia and Odynophagia present unique hurdles. Dysphagia challenges the physical act of swallowing, while odynophagia introduces pain into the equation. While both conditions can be distressing, they are manageable with proper diagnosis and treatment. Understanding these challenges is the first step toward providing support and relief for those affected by these conditions, allowing them to enjoy a more comfortable and fulfilling life.