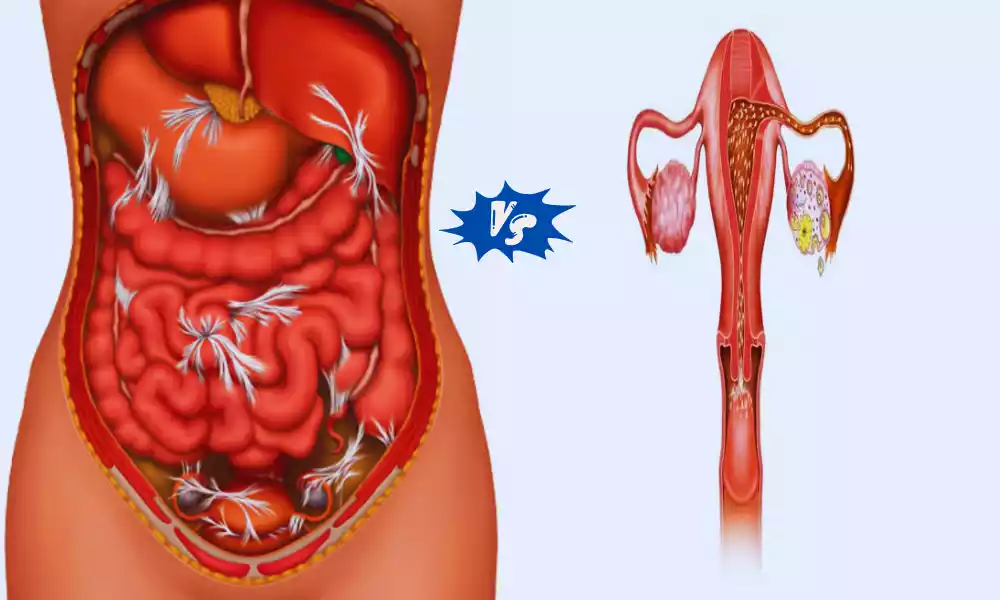
Peritonitis and Salpingitis are inflammatory conditions that impact the abdominal cavity and the fallopian tubes, respectively. While peritonitis involves inflammation of the peritoneum, the lining of the abdominal cavity, salpingitis pertains to inflammation of the fallopian tubes.
What is Peritonitis?

Peritonitis is a serious medical condition characterized by inflammation or infection of the peritoneum, a thin membrane lining the abdominal cavity. This condition usually arises when bacteria or other infectious agents enter the peritoneal space, often due to a rupture or perforation of an abdominal organ. Common causes include gastrointestinal perforations (such as a burst appendix or an ulcer), abdominal surgery, trauma, or certain gastrointestinal diseases.
Symptoms of peritonitis are typically severe and can include intense abdominal pain, tenderness, bloating, nausea, vomiting, fever, chills, and a general feeling of illness. Prompt medical attention is crucial when peritonitis is suspected because it can progress rapidly and lead to life-threatening complications, such as sepsis or organ failure.
Treatment usually involves hospitalization, intravenous antibiotics to combat the infection, and, in severe cases, surgery to repair the underlying issue and remove infected tissue. Early diagnosis and intervention are critical to improve the chances of a successful recovery from peritonitis.
Types of Peritonitis
Peritonitis can be categorized into different types based on its underlying causes and clinical presentations:
- Primary Peritonitis: This type occurs without a clear source of infection in the abdominal cavity. It is relatively rare and is typically associated with underlying medical conditions that weaken the immune system, such as cirrhosis.
- Secondary Peritonitis: Secondary peritonitis is more common and arises from a clear source of infection or inflammation, often due to a rupture, perforation, or infection of abdominal organs. Gastrointestinal perforations and postoperative infections are common causes.
- Tertiary Peritonitis: This is a more complicated form of peritonitis that occurs when the infection persists or recurs after initial treatment for secondary peritonitis. It often requires specialized care and may be associated with multidrug-resistant bacteria.
- Localized Peritonitis: In some cases, peritonitis may be confined to a specific area of the abdominal cavity, forming an abscess. This can occur as a complication of primary or secondary peritonitis.
- Spontaneous Bacterial Peritonitis (SBP): SBP is a specific type of peritonitis that primarily affects individuals with liver disease (cirrhosis) and ascites (fluid buildup in the abdominal cavity). It is caused by bacteria entering the peritoneal cavity without an obvious source of perforation.
Each type of peritonitis has its own distinct causes, risk factors, and clinical characteristics, which can influence the approach to diagnosis and treatment.
Causes of Peritonitis
Peritonitis can be caused by various factors, primarily involving infection or inflammation of the peritoneum, a thin membrane lining the abdominal cavity. Common causes include:
- Gastrointestinal Perforations: Ruptured appendix, perforated ulcer, or injuries to the gastrointestinal tract can allow bacteria or contaminants to enter the peritoneal cavity.
- Abdominal Surgery: Infections can develop postoperatively, particularly if there is contamination during surgery.
- Trauma: Blunt or penetrating trauma to the abdomen can lead to peritoneal injury and infection.
- Gastrointestinal Conditions: Certain diseases like diverticulitis or Crohn’s disease can increase the risk of peritonitis.
- Intraperitoneal Dialysis: Peritonitis can occur as a complication of peritoneal dialysis when the catheter site becomes infected.
- Primary Bacterial Infection: Rarely, peritonitis can develop without a clear source of infection, often in individuals with weakened immune systems, such as those with cirrhosis.
Prompt diagnosis and treatment are essential to manage peritonitis effectively and prevent potentially life-threatening complications.
Symptoms of Peritonitis
Symptoms of peritonitis can include:
- Severe abdominal pain and tenderness
- Abdominal bloating or distention
- Nausea and vomiting
- Fever and chills
- Rapid breathing
- Reduced or absent bowel movements
- Increased heart rate
- Fatigue and weakness
- Loss of appetite
- Unable to eliminate gas or have intestinal movement
- Dehydration
- Confusion or altered mental state (in severe cases)
- Shock (a life-threatening condition characterized by low blood pressure and organ dysfunction) if left untreated.
What is Salpingitis?
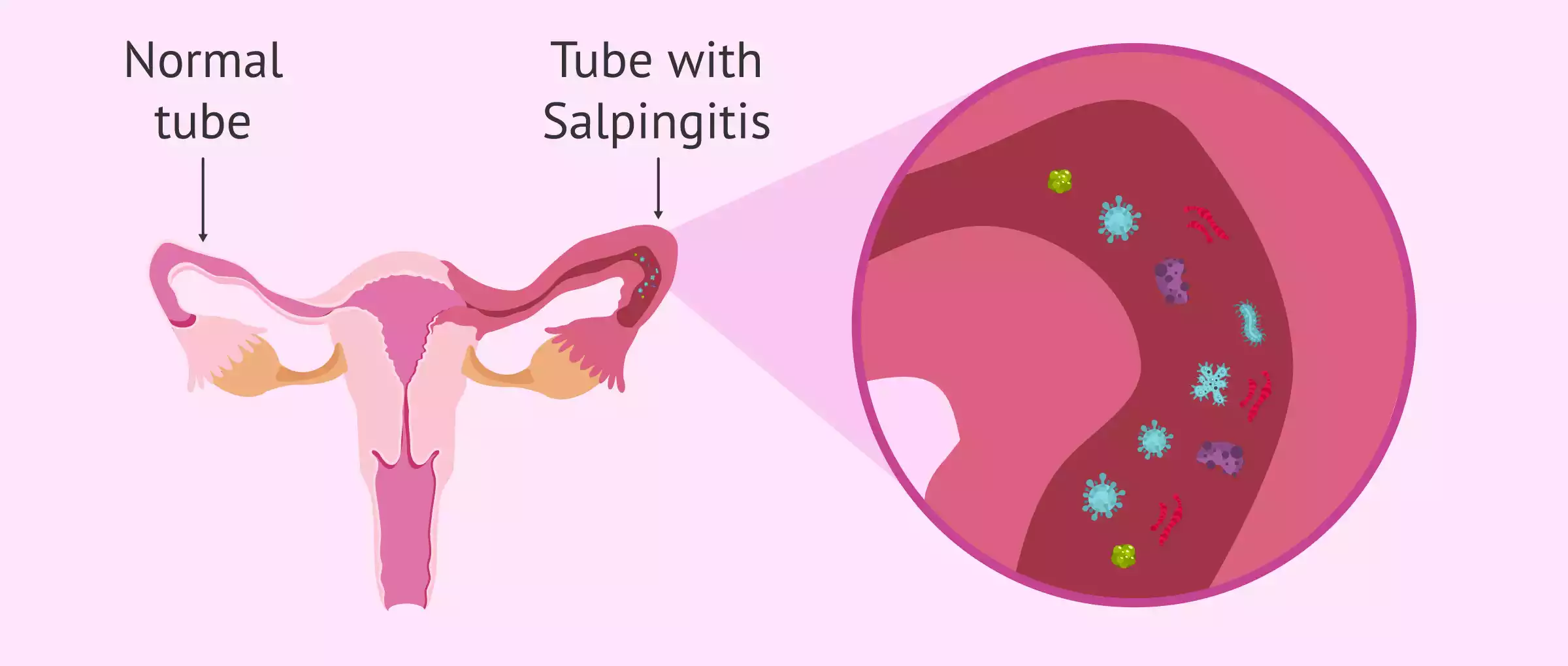
Salpingitis is a medical condition characterized by inflammation or infection of the fallopian tubes, which are essential components of the female reproductive system. These tubes connect the ovaries to the uterus and play a crucial role in transporting eggs from the ovaries to the uterus for fertilization. Salpingitis is typically caused by the ascent of bacteria from the lower genital tract into the fallopian tubes. The most common culprits are sexually transmitted infections (STIs), such as chlamydia and gonorrhea. Non-STI-related infections can also lead to salpingitis.
Symptoms of salpingitis can vary but often include pelvic pain, especially during or after sexual intercourse, abnormal vaginal discharge, fever, and fatigue. If left untreated, the infection can damage the fallopian tubes, leading to serious complications.
One of the most concerning complications is infertility, as scar tissue or blockages within the fallopian tubes can hinder the normal movement of eggs and sperm. Additionally, untreated salpingitis increases the risk of ectopic pregnancy, a condition in which a fertilized egg implants outside the uterus, usually within a fallopian tube, which can be life-threatening.
Prompt diagnosis and appropriate treatment, typically involving antibiotics, are crucial to manage salpingitis effectively and prevent potential long-term reproductive health issues. If you suspect you may have salpingitis or are experiencing any symptoms, it’s essential to seek medical attention promptly to prevent complications and protect your reproductive health.
Causes of Salpingitis
Salpingitis is primarily caused by bacterial infections, often stemming from the following:
- Sexually Transmitted Infections (STIs): Common STIs like chlamydia and gonorrhea can ascend into the fallopian tubes and cause salpingitis.
- Non-STI Bacterial Infections: Bacteria from other sources can also lead to salpingitis, although less commonly.
- Pelvic Inflammatory Disease (PID): Salpingitis can be a complication of PID, which involves inflammation and infection of the female reproductive organs, including the fallopian tubes.
The infection typically starts in the lower genital tract and then spreads to the fallopian tubes, causing inflammation and potential damage if left untreated.
Symptoms of Salpingitis
Symptoms of salpingitis can include:
- Pelvic discomfort or pain typically manifests itself on one side.
- Abnormal vaginal discharge, which may be foul-smelling
- Painful or uncomfortable sexual intercourse
- Fever and chills
- Fatigue
- Lower abdominal pain
- Irregular menstrual bleeding
- Painful urination
- Nausea and vomiting (in severe cases)
- Infertility or difficulty conceiving (as a long-term complication)
It’s essential to seek medical attention if you experience these symptoms, especially if you suspect you may be at risk for salpingitis due to recent unprotected sexual activity or a history of STIs. Early diagnosis and treatment are crucial to prevent complications and preserve reproductive health.
Complications of Untreated Salpingitis
Untreated salpingitis can lead to several serious complications, including:
- Infertility: Scar tissue and damage to the fallopian tubes can hinder the normal passage of eggs and sperm, making it difficult for fertilization to occur.
- Ectopic Pregnancy: The risk of ectopic pregnancy increases with salpingitis. Failure of fertilization occurs when an embryo fertilized through in vitro fertilization becomes implanted outside the uterus, often inside the fallopian tube.
- Chronic Pelvic Pain: Ongoing inflammation and scarring can lead to persistent pelvic pain and discomfort.
- Pelvic Abscess: In severe cases, untreated salpingitis can result in the formation of a pus-filled pocket within the pelvic cavity called an abscess.
- Spread of Infection: The infection can potentially spread to other reproductive organs, leading to more extensive pelvic inflammatory disease (PID).
Prompt medical intervention and treatment are crucial to prevent these complications and protect reproductive health.
Diagnosis and Medical Assessment of Peritonitis and Salpingitis
Diagnosing Peritonitis:
- Medical History: Assessing symptoms, surgeries, and underlying conditions.
- Physical Exam: Checking for abdominal tenderness and signs of infection.
- Lab Tests: Including CBC, blood cultures, and chemistry panel to evaluate infection and organ function.
- Imaging: Using X-rays and CT scans to visualize the abdomen.
- Paracentesis: Collecting peritoneal fluid for analysis.
- Exploratory Laparotomy: Surgical exploration in severe cases.
Diagnosing Salpingitis:
- Medical History: Discussing symptoms, sexual activity, STIs, and pelvic pain.
- Physical Exam: Evaluating the pelvic area for tenderness and abnormalities.
- Lab Tests: Including STI testing and pregnancy tests.
- Imaging: Using pelvic ultrasound to visualize the fallopian tubes.
- Laparoscopy: In severe or uncertain cases, a minimally invasive procedure may be done to directly examine the pelvic organs.
Both conditions require prompt diagnosis and appropriate treatment, often involving antibiotics, to prevent complications and ensure a successful recovery.
Effective Treatment Approaches for Peritonitis and Salpingitis
Effective treatment approaches for Peritonitis:
- Antibiotics: Prompt administration of broad-spectrum antibiotics to target the underlying infection.
- Fluid and Electrolyte Replacement: Intravenous fluids to maintain hydration and electrolyte balance.
- Surgery: In severe cases, surgical intervention to repair perforations, remove infected tissue, or address the underlying cause.
- Supportive Care: Pain management and monitoring for complications like sepsis.
Effective treatment approaches for Salpingitis:
- Antibiotics: Administering antibiotics to clear the infection, often including treatment for possible STIs.
- Pain Management: Pain relief measures, such as over-the-counter pain relievers or prescription medication.
- Management of Underlying Causes: Treating any underlying conditions contributing to the infection.
- Follow-up Care: Regular monitoring to ensure the infection has resolved and to address potential complications.
Timely and appropriate treatment is essential for both conditions to prevent complications and promote recovery.
Difference table of Peritonitis and Salpingitis
Here’s a difference table outlining the key distinctions between Peritonitis and Salpingitis:
| Characteristic | Peritonitis | Salpingitis |
|---|---|---|
| Affected Area | Peritoneum, the abdominal cavity lining | Fallopian tubes, part of the reproductive system |
| Common Causes | Gastrointestinal perforations, abdominal surgery, trauma | Bacterial infections, often due to sexually transmitted infections (STIs) |
| Symptoms | Severe abdominal pain, tenderness, nausea, fever, vomiting | Pelvic pain, abnormal vaginal discharge, painful intercourse, fever |
| Diagnosis | Physical examination, imaging (X-rays, CT scans), laboratory tests, paracentesis | Physical examination, STI testing, pelvic ultrasound, laparoscopy (in severe cases) |
| Complications | Sepsis, organ damage, perforation, abscess formation | Infertility, ectopic pregnancy, chronic pelvic pain |
| Treatment | Antibiotics, fluid and electrolyte replacement, surgery if necessary | Antibiotics, pain management, addressing underlying causes |
| Prevention | Good hygiene, prompt infection treatment, wound care | Safe sex practices, early STI treatment, regular gynecological check-ups |
| Affected Gender | Both males and females can develop peritonitis | Primarily affects females |
| Risk Factors | Surgery, abdominal trauma, gastrointestinal conditions | Unprotected sex, multiple sexual partners, STIs |
| Importance of Timely Treatment | Urgent; untreated peritonitis can be life-threatening | Urgent; untreated salpingitis can lead to infertility and ectopic pregnancy |
Understanding these differences is crucial for proper diagnosis, treatment, and prevention of these two distinct medical conditions.
Final Thought
Salpingitis and peritonitis are serious medical ailments requiring immediate medical treatment. By understanding their causes, symptoms, and treatment options, individuals can take proactive steps to protect their reproductive and abdominal health. Prioritizing good hygiene, safe sex practices, and seeking medical care when needed are key to preventing these conditions and ensuring overall well-being.