Heberden’s and Bouchard’s Nodes are distinct clinical features associated with osteoarthritis, a common joint disorder. These nodes are bony swellings or outgrowths that typically affect the fingers. Heberden’s nodes occur at the distal interphalangeal joints (DIP joints), which are the joints closest to the fingertips, while Bouchard’s nodes manifest at the proximal interphalangeal joints (PIP joints), located in the middle of the fingers. Understanding the differences and similarities between these two types of nodes is crucial for accurate diagnosis and effective management of osteoarthritis.
Heberden’s Nodes
Heberden’s nodes are bony enlargements or outgrowths that develop at the distal interphalangeal joints (DIP joints) of the fingers. These nodes are a characteristic feature of osteoarthritis, a degenerative joint disease, and they are typically found in the joints closest to the fingertips. Heberden’s nodes can lead to joint deformity, pain, and limited mobility in the affected fingers, and they are considered a clinical sign of osteoarthritis in the hands.

Causes of Heberden’s Nodes
Heberden’s nodes are primarily caused by osteoarthritis, a degenerative joint disease characterized by the breakdown of cartilage and the subsequent formation of bone spurs at the distal interphalangeal joints (DIP joints) of the fingers. Osteoarthritis can occur for various reasons that may not always be clear.
There can be multiple causes for its growth; among them are:
-
- Age: Osteoarthritis is more common in older individuals, as joint wear and tear accumulate over time.
- Genetic Factors: Family history can increase the risk of developing osteoarthritis and Heberden’s nodes.
- Joint Overuse: Repeated stress and strain on the finger joints, often due to occupational or recreational activities, can contribute to osteoarthritis.
- Joint Injuries: Previous finger injuries, fractures, or dislocations may increase the likelihood of osteoarthritis and the formation of nodes.
- Gender: Osteoarthritis, including Heberden’s nodes, is more prevalent in women, especially after menopause.
- Obesity: Excess body weight can place additional stress on joints, increasing the risk of osteoarthritis.
- Joint Alignment: Abnormal joint alignment or joint deformities can contribute to osteoarthritis development.
While these factors play a role in the development of Heberden’s nodes, the specific cause and progression of osteoarthritis can vary from person to person.
Symptoms of Heberden’s Nodes
Heberden’s nodes are a characteristic feature of osteoarthritis in the distal interphalangeal joints (DIP joints) of the fingers. The presence of Heberden’s nodes may be associated with various symptoms, including:
-
- Swelling: The affected DIP joints may appear enlarged or swollen due to the presence of bony growths.
- Pain: Individuals with Heberden’s nodes often experience pain and discomfort in the affected fingers, especially during joint movement or when pressure is applied.
- Stiffness: The fingers may become stiff, making it challenging to bend or straighten them fully.
- Reduced Range of Motion: Due to joint damage and inflammation, there is often a limitation in the range of motion of the fingers, making tasks like gripping objects or performing fine motor skills difficult.
- Joint Deformity: Over time, Heberden’s nodes can lead to joint deformities, with the fingers appearing misshapen or crooked.
- Tenderness: The affected joints may be tender to the touch, causing discomfort even with gentle pressure.
- Weakness: Some individuals may experience weakness in the fingers affected by Heberden’s nodes, impacting their ability to perform everyday tasks.
In terms of severity, symptoms may vary from one individual to the next. Not everyone with Heberden’s nodes will experience all of these symptoms, and the progression of osteoarthritis may be slow or more rapid in different individuals. Seeking medical advice and appropriate management can help alleviate symptoms and improve the quality of life for those affected by Heberden’s nodes.
Bouchard’s Nodes
Bouchard’s nodes are bony growths or enlargements that form at the proximal interphalangeal joints (PIP joints) of the fingers. These nodes are a distinctive feature of osteoarthritis, a degenerative joint disorder, and they usually develop in the middle joints of the fingers. Bouchard’s nodes can cause joint deformity, discomfort, and restricted movement in the affected fingers, and they serve as a clinical indicator of osteoarthritis in the hand joints.

Causes of Bouchard’s Nodes
Bouchard’s nodes are primarily caused by osteoarthritis, a degenerative joint disease that results in the formation of bony growths at the proximal interphalangeal joints (PIP joints) of the fingers.
The causes and risk factors for Bouchard’s nodes are similar to those of Heberden’s nodes and may include:
-
- Aging: Osteoarthritis becomes more common as individuals age, with joint wear and tear accumulating over time.
- Genetic Factors: A family history of osteoarthritis can increase the risk of developing the condition and, subsequently, Bouchard’s nodes.
- Joint Overuse: Repetitive strain on the finger joints, often due to certain occupational or recreational activities, can contribute to the development of osteoarthritis and the formation of nodes.
- Joint Injuries: Previous finger injuries, fractures, or dislocations may predispose individuals to osteoarthritis and the appearance of Bouchard’s nodes.
- Gender: Osteoarthritis, including Bouchard’s nodes, tends to be more common in women, particularly after menopause.
- Obesity: Excess body weight can increase the mechanical stress on joints, raising the risk of osteoarthritis and the growth of nodes.
- Joint Alignment: Abnormal joint alignment or pre-existing joint deformities can contribute to the development of osteoarthritis and the appearance of Bouchard’s nodes.
- Other Medical Conditions: Certain medical conditions, such as rheumatoid arthritis or metabolic disorders, can increase the likelihood of osteoarthritis and the formation of nodes in the fingers.
While these factors can contribute to the development of Bouchard’s nodes, the precise cause and progression of osteoarthritis can vary from person to person.
Symptoms of Bouchard’s Nodes
Bouchard’s nodes are a characteristic feature of osteoarthritis in the proximal interphalangeal joints (PIP joints) of the fingers. The presence of Bouchard’s nodes may be associated with various symptoms, including:
-
- Swelling: The PIP joints in the affected fingers may appear enlarged or swollen due to the presence of bony growths.
- Pain: Individuals with Bouchard’s nodes often experience pain and discomfort in the affected fingers, particularly during joint movement or when pressure is applied.
- Stiffness: The fingers may become stiff, making it difficult to bend or straighten them fully.
- Reduced Range of Motion: Due to joint damage and inflammation, there is often a limitation in the range of motion of the fingers, affecting tasks that require finger flexibility.
- Joint Deformity: Over time, Bouchard’s nodes can lead to joint deformities, causing the fingers to appear misshapen or crooked.
- Tenderness: The affected PIP joints may be tender to the touch, causing discomfort even with gentle pressure.
- Weakness: Some individuals may experience weakness in the fingers affected by Bouchard’s nodes, which can impact their ability to perform everyday tasks.
- Skin Changes: In some cases, skin changes, such as redness or warmth, may be noticeable over the affected joints.
The severity of symptoms can vary among individuals, and not everyone with Bouchard’s nodes will experience all of these symptoms. Additionally, the progression of osteoarthritis leading to Bouchard’s nodes may be gradual or more rapid, depending on individual factors. Seeking medical evaluation and appropriate management can help alleviate symptoms and improve the quality of life for those affected by Bouchard’s nodes.
Comparison Table of Heberden’s and Bouchard’s Nodes
Here’s a comparison table highlighting the key differences between Heberden’s and Bouchard’s nodes:
| Aspect | Heberden’s Nodes | Bouchard’s Nodes |
|---|---|---|
| Location | Distal interphalangeal (DIP) joints | Proximal interphalangeal (PIP) joints |
| Appearance | Bony outgrowths at fingertip joints | Bony outgrowths in middle finger joints |
| Finger Joints Affected | Joints closest to the fingertips | Joints in the middle of the fingers |
| Common Finger Involvement | Thumb, index, and middle fingers | Middle and ring fingers |
| Primary Cause | Osteoarthritis | Osteoarthritis |
| Risk Factors | Age, genetics, joint overuse, injuries | Age, genetics, joint overuse, injuries |
| Associated Conditions | Osteoarthritis, joint pain, stiffness | Osteoarthritis, joint pain, stiffness |
| Typical Symptoms | – Swelling
– Pain – Stiffness – Reduced range of motion – Joint deformity |
– Swelling
– Pain – Stiffness – Reduced range of motion – Joint deformity |
| Diagnosis | Clinical examination, X-rays | Clinical examination, X-rays |
| Treatment Options | – Pain relievers
– Physical therapy – Occupational therapy – Joint injections – Surgery (in severe cases) – Lifestyle modifications – Complementary therapies |
– Pain relievers
– Physical therapy – Occupational therapy – Joint injections – Surgery (in severe cases) – Lifestyle modifications – Complementary therapies |
| Commonality in Symptoms | Both can cause similar symptoms such as pain, swelling, stiffness, and joint deformity. | Both can cause similar symptoms such as pain, swelling, stiffness, and joint deformity. |
| Joint Involvement | Mainly DIP joints | Mainly PIP joints |
Heberden’s and Bouchard’s nodes are both associated with osteoarthritis, and the treatment and management approaches for both conditions are often similar. The primary difference lies in the specific finger joints affected, with Heberden’s nodes impacting the joints closest to the fingertips and Bouchard’s nodes affecting the middle finger joints.
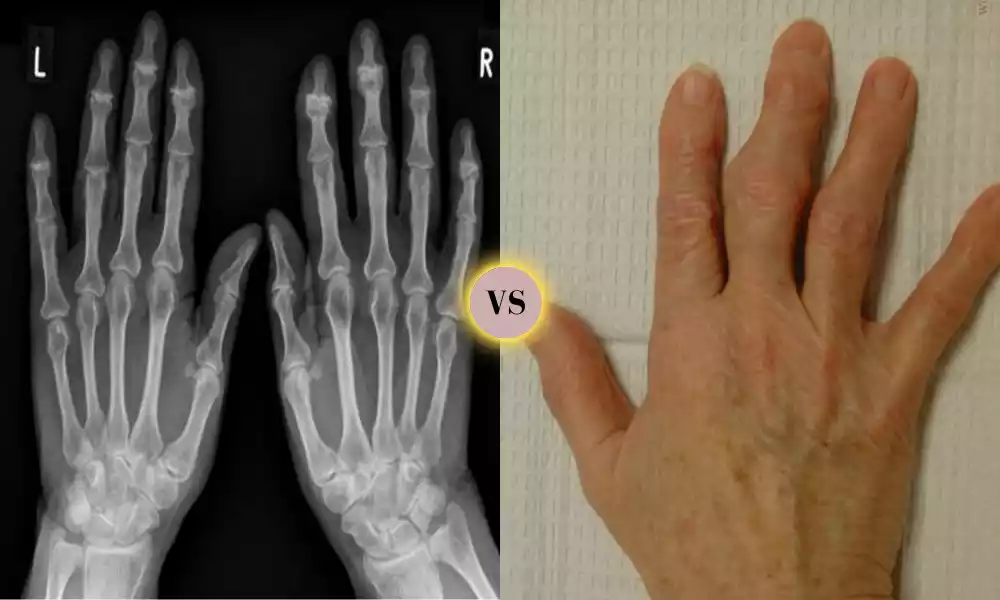
Diagnosis of Heberden’s and Bouchard’s Nodes
Diagnosing Heberden’s and Bouchard’s nodes typically involves a combination of clinical evaluation, medical history, and imaging studies. Here’s a brief outline of our diagnostic procedure:
- Clinical Assessment:
- A healthcare provider will conduct a physical examination, focusing on the affected fingers and joints.
- They will look for characteristic signs, such as bony enlargements at the distal interphalangeal joints (DIP joints) for Heberden’s nodes or at the proximal interphalangeal joints (PIP joints) for Bouchard’s nodes.
- The provider will assess the presence of symptoms like pain, tenderness, stiffness, and joint deformity.
- Medical History:
- The patient’s medical history is essential for diagnosis. The healthcare provider will inquire about symptoms, their duration, and any relevant medical conditions or injuries.
- Imaging Studies:
- X-rays: X-ray imaging is a crucial tool for confirming the presence of Heberden’s or Bouchard’s nodes. X-rays can reveal bony growths, joint damage, and the extent of osteoarthritis.
- Other Imaging: In some cases, more advanced imaging modalities like MRI (Magnetic Resonance Imaging) or ultrasound may be used to evaluate joint structures and rule out other conditions.
- Laboratory Tests:
- Blood tests are typically not used for the diagnosis of Heberden’s or Bouchard’s nodes directly. They may be ordered to rule out other forms of arthritis, such as rheumatoid arthritis, which can have similar symptoms.
- Differential Diagnosis:
- The healthcare provider will consider other conditions that can cause finger joint pain and swelling, such as rheumatoid arthritis, gout, or psoriatic arthritis. A proper diagnosis will help distinguish between these conditions.
- Consultation with a Specialist:
- In some cases, a referral to a rheumatologist or an orthopedic specialist may be necessary for a more comprehensive evaluation, especially if the diagnosis is unclear or if additional treatment options need to be explored.
It’s important to seek medical attention if you suspect you have Heberden’s or Bouchard’s nodes or are experiencing symptoms in your finger joints. Early diagnosis and appropriate management can help alleviate symptoms, slow the progression of osteoarthritis, and improve your quality of life.
Treatment for Heberden’s and Bouchard’s Nodes
The treatment for Heberden’s and Bouchard’s nodes primarily focuses on managing the symptoms, slowing the progression of osteoarthritis, and improving joint function. While these nodes cannot be completely eliminated, various treatment approaches can help individuals affected by them.
Treatment options include:
- Medications:
- Pain Relievers: Over-the-counter pain relievers such as acetaminophen (Tylenol) or nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen can help reduce pain and inflammation associated with Heberden’s and Bouchard’s nodes.
- Prescription Medications: In more severe cases or when over-the-counter medications are not effective, a healthcare provider may prescribe stronger pain relievers or disease-modifying drugs for osteoarthritis.
- Physical Therapy:
- Physical therapy exercises and techniques can help improve joint mobility, strengthen the muscles around the affected joints, and enhance overall joint function.
- Occupational Therapy:
- Occupational therapists can teach individuals how to perform daily activities more efficiently and with less stress on the affected finger joints. They may also recommend assistive devices or splints.
- Hot and Cold Therapy:
- Applying heat (warm compresses) or cold (ice packs) to the affected joints can provide temporary relief from pain and inflammation.
- Joint Injections:
- Corticosteroid injections directly into the affected joints can provide significant pain relief and reduce inflammation, though the effects are usually temporary and may need to be repeated.
- Surgical Options:
- In severe cases where conservative treatments are ineffective and quality of life is significantly impaired, surgical options such as joint fusion or joint replacement surgery may be considered. These procedures aim to alleviate pain and improve joint function.
- Lifestyle Modifications:
- Weight management: Maintaining a healthy weight can reduce stress on the finger joints and slow the progression of osteoarthritis.
- Joint protection techniques: Learning how to perform tasks with minimal joint stress can help manage symptoms.
- Adaptive devices: Using assistive devices like jar openers, padded utensils, or ergonomic tools can make daily activities easier on the joints.
- Alternative Therapies:
- Some individuals find relief from complementary therapies such as acupuncture, dietary supplements, or herbal remedies. Prior to making any decisions about alternative treatments, it is vitally important that you discuss all available options with a healthcare professional.
- Patient Education:
- Understanding the condition, its progression, and self-management strategies can empower individuals to better cope with Heberden’s and Bouchard’s nodes.
The choice of treatment depends on the severity of symptoms, the impact on daily life, and the individual’s overall health. Healthcare providers will work with patients to develop a personalized treatment plan that addresses their specific needs and goals. Regular follow-up appointments are crucial to monitor progress and adjust the treatment plan as necessary.
Similarities – Heberden’s and Bouchard’s Nodes
Heberden’s and Bouchard’s nodes share several similarities due to their common association with osteoarthritis. Here are some key similarities between the two:
- Osteoarthritis Association: Both Heberden’s and Bouchard’s nodes are characteristic features of osteoarthritis, a degenerative joint disease that affects the fingers.
- Symptoms: They can both cause similar symptoms, including pain, swelling, stiffness, tenderness, reduced range of motion, and joint deformity in the affected fingers.
- Risk Factors: The risk factors for developing Heberden’s and Bouchard’s nodes are similar and often include factors such as age, genetics, joint overuse, and previous joint injuries.
- Diagnosis: The diagnostic process for both conditions involves clinical examination and imaging studies like X-rays to confirm the presence of bony growths at the affected finger joints.
- Treatment Approaches: The treatment options for Heberden’s and Bouchard’s nodes overlap significantly and may include pain relievers, physical therapy, occupational therapy, joint injections, surgery (in severe cases), lifestyle modifications, and complementary therapies.
- Impact on Daily Life: Both conditions can affect an individual’s quality of life by limiting finger function and causing discomfort or pain during everyday activities.
- Progressive Nature: Both Heberden’s and Bouchard’s nodes are part of the progressive nature of osteoarthritis, where joint damage and symptoms tend to worsen over time.
- Management Focus: The management of Heberden’s and Bouchard’s nodes aims to reduce pain, improve joint function, and slow the progression of osteoarthritis. This often involves a combination of conservative treatments and lifestyle adjustments.
While Heberden’s and Bouchard’s nodes may affect different finger joints, they are both manifestations of osteoarthritis and share many common characteristics in terms of symptoms, risk factors, diagnosis, and treatment approaches.
Coping with Heberden’s and Bouchard’s Nodes
Coping with Heberden’s and Bouchard’s nodes, which are associated with osteoarthritis in the fingers, can be challenging, but there are various strategies and lifestyle adjustments that can help improve your quality of life and manage the symptoms.
Here are some coping strategies:
- Medical Consultation: Seek medical advice and guidance from a healthcare provider who specializes in arthritis or orthopedics. They can help confirm the diagnosis, assess the severity of the condition, and develop a personalized treatment plan.
- Medications: Work with your healthcare provider to determine appropriate pain relief medications or anti-inflammatory drugs. Over-the-counter options or prescription medications may be recommended based on your symptoms.
- Physical Therapy: Consider physical therapy to improve joint mobility, strengthen the muscles around the affected finger joints, and learn exercises that can help manage pain and stiffness.
- Occupational Therapy: An occupational therapist can provide strategies and assistive devices to help you perform daily tasks with less stress on your finger joints. They may recommend adaptive tools and techniques.
- Joint Protection: Learn joint protection techniques to reduce the risk of exacerbating symptoms. This may involve modifying the way you perform certain activities, such as lifting or gripping objects.
- Heat and Cold Therapy: Applying heat (warm compresses) or cold (ice packs) to the affected finger joints can help alleviate pain and reduce inflammation. Discuss these potential options with your healthcare professional.
- Medication Management: If prescribed medications, follow your healthcare provider’s instructions carefully, and be aware of potential side effects or interactions with other medications you may be taking.
- Lifestyle Adjustments:
- Maintain a healthy weight to reduce stress on your finger joints.
- Use assistive devices like jar openers, padded utensils, or ergonomic tools to make daily activities easier.
- Consider wearing splints or braces on affected fingers, especially during activities that may strain the joints.
- Pain Management Techniques:
- Explore relaxation techniques, deep breathing exercises, or mindfulness meditation to manage pain and stress associated with the condition.
- Support Groups: Joining a support group for individuals with osteoarthritis or specifically for those with Heberden’s and Bouchard’s nodes can provide emotional support, shared experiences, and practical tips for coping.
- Stay Active: Engage in gentle, low-impact exercises such as swimming, walking, or stationary cycling to help maintain joint mobility and overall fitness. Inform yourself by seeking guidance from healthcare professionals or physical therapists regarding recommended exercises.
- Balanced Diet: Eat a balanced diet rich in anti-inflammatory foods, such as fruits, vegetables, whole grains, and fatty fish like salmon. Adequate nutrition can help support overall joint health.
- Regular Check-Ups: Maintain regular follow-up appointments with your healthcare provider to monitor your condition, adjust your treatment plan as needed, and address any concerns.
Remember that coping with Heberden’s and Bouchard’s nodes is a long-term process, and individual experiences may vary. It’s essential to work closely with healthcare professionals, follow their recommendations, and adapt strategies as needed to manage your symptoms and improve your quality of life.
Conclusion
Heberden’s and Bouchard’s nodes are distinct clinical features associated with osteoarthritis in the fingers. Heberden’s nodes affect the distal interphalangeal joints (DIP joints), whereas Bouchard’s nodes manifest at the proximal interphalangeal joints (PIP joints). Both conditions share similarities in terms of symptoms, risk factors, diagnosis, and treatment approaches.
Coping strategies involve medical consultation, medication management, physical and occupational therapy, joint protection techniques, lifestyle adjustments, and support from healthcare providers and support groups. While these nodes cannot be entirely eliminated, proactive management can help improve joint function and quality of life for individuals living with Heberden’s and Bouchard’s nodes.