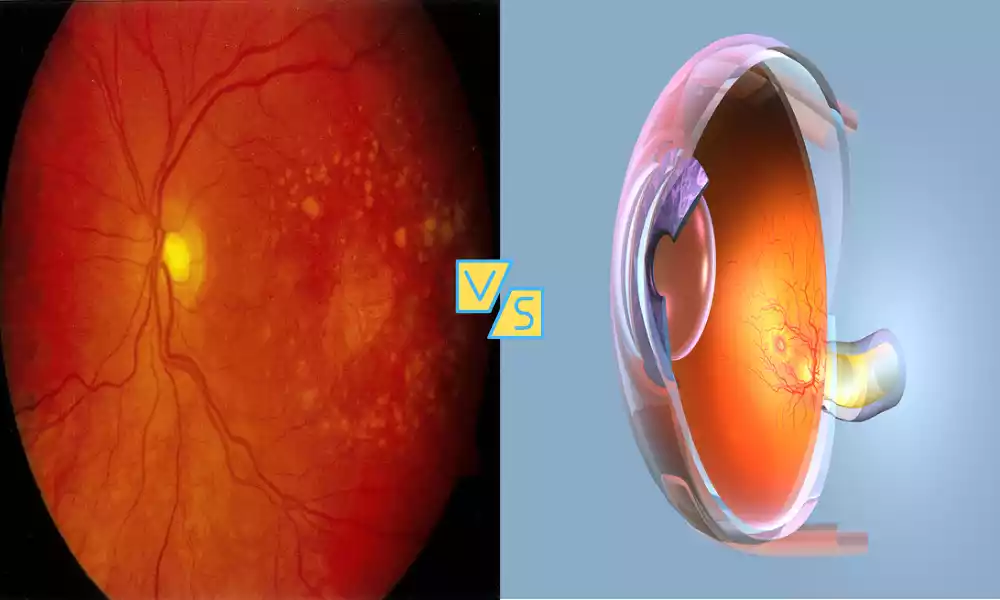
Macular Degeneration and Macular Edema are eye conditions that can impact your vision. Macular Degeneration, also known as AMD, affects older adults and damages the central part of the retina, leading to vision loss. Macular Edema, on the other hand, is characterized by the swelling of the macula due to fluid buildup and can result from various eye-related issues. Both conditions can cause blurred or distorted vision, making early detection and treatment essential.
Macular Degeneration

Macular degeneration, also known as age-related macular degeneration (AMD), is a progressive eye disease characterized by the deterioration of the macula, the central and most sensitive part of the retina in the eye.
This degeneration can result in the loss of central vision, making it difficult to see fine details, read, or recognize faces. Macular degeneration is primarily associated with aging and is a leading cause of vision impairment in older adults. It exists in two primary forms: dry macular degeneration, marked by the gradual breakdown of macular cells, and wet macular degeneration, characterized by the growth of abnormal blood vessels beneath the macula, which can leak and cause rapid vision loss.
Symptoms of Macular Degeneration
Macular degeneration can manifest with various symptoms, and these symptoms can vary in severity. Macular degeneration symptoms commonly seen include:
-
- Blurred or Distorted Vision: One of the earliest signs is often a gradual blurring of central vision. Straight lines may appear wavy or distorted.
- Difficulty Reading: People with macular degeneration may find it challenging to read small print or engage in activities that require sharp, detailed vision.
- Dark or Empty Spots: A blind spot in the center of the visual field may develop, making it difficult to see objects directly in front of you.
- Decreased Color Perception: Colors may appear less vibrant or accurate.
- Difficulty Recognizing Faces: Recognizing faces, particularly at a distance, can become challenging.
- Increased Sensitivity to Light: Some individuals with macular degeneration may experience heightened sensitivity to light (photophobia).
It’s essential to note that macular degeneration typically affects central vision while peripheral vision remains intact. This allows individuals to retain some level of functional vision despite the central vision impairment. The disease can progress, leading to more severe vision loss over time. Regular eye exams are crucial for early detection and intervention, as treatment options are more effective when initiated early in the course of the disease.
Causes of Macular Degeneration
The exact causes of macular degeneration are not fully understood, but several factors, both genetic and environmental, are believed to contribute to the development of this condition.
The primary causes and risk factors for macular degeneration include:
- Aging: Age-related macular degeneration (AMD) is the most common form and is strongly associated with aging. As people get older, their risk for AMD increases.
- Genetics: Family history plays a role, as there is evidence of a genetic predisposition to AMD. Any person with a history of the disease is at greater risk.
- Smoking: Smoking is a significant modifiable risk factor for macular degeneration. Smokers have a higher risk of developing both dry and wet AMD.
- Hypertension (High Blood Pressure): Uncontrolled high blood pressure is associated with an increased risk of developing AMD.
- Dietary Factors: A diet lacking in certain nutrients, such as antioxidants (vitamins A, C, and E), zinc, and omega-3 fatty acids, may contribute to the development or progression of AMD.
- Sunlight Exposure: Excessive exposure to ultraviolet (UV) light, especially without adequate eye protection, may be a risk factor.
- Obesity: Being overweight or obese is associated with an increased risk of AMD.
- Cardiovascular Disease: Conditions like atherosclerosis and high cholesterol levels may contribute to the development of AMD.
- Gender: Women are at a slightly higher risk of developing AMD than men.
- Race and Ethnicity: AMD is more common in individuals of Caucasian descent.
- Drusen Deposits: The presence of drusen, small yellow deposits under the retina, is often seen in individuals with AMD.
- Other Health Conditions: Certain medical conditions, such as diabetes, may increase the risk of developing macular degeneration.
While these factors are associated with an increased risk, not everyone with these risk factors will develop macular degeneration, and individuals without these risk factors can still develop the condition. Regular eye examinations and lifestyle modifications, such as not smoking, maintaining a healthy diet, and managing conditions like hypertension and diabetes, can help reduce the risk and slow the progression of macular degeneration.
Macular Edema

Macular edema is a medical condition characterized by the abnormal accumulation of fluid within the macula, which is the central and most sensitive part of the retina in the eye. This fluid buildup can lead to swelling and thickening of the macula, resulting in blurred or distorted central vision.
Macular edema can occur as a complication of various underlying eye conditions or diseases and is often associated with reduced visual acuity and difficulty in tasks that require clear central vision.
Symptoms of Macular Edema
The symptoms of macular edema can vary in severity and may include the following:
-
- Blurred or Distorted Vision: The most common symptom is a noticeable blurring of central vision, which can make it difficult to see fine details or read small print.
- Visual Distortions: Straight lines may appear wavy or bent, a phenomenon known as metamorphopsia.
- Reduced Central Vision: You may experience a central blind spot or dark spot in your field of vision, which can interfere with activities like reading, recognizing faces, or watching television.
- Colors Appear Faded: Some people with macular edema notice a reduction in color intensity, with colors appearing less vibrant than usual.
- Difficulty in Low Light: Vision problems may worsen in low-light conditions, making it challenging to see clearly in dimly lit environments.
- Visual Fluctuations: Symptoms can vary throughout the day, with some individuals reporting better or worse vision at different times.
Macular Edema is often associated with underlying medical conditions, such as diabetic retinopathy or age-related macular degeneration, so the presence of these symptoms should prompt a comprehensive eye examination and evaluation by an eye care professional for proper diagnosis and treatment. Early detection and management are crucial in preserving vision and preventing further deterioration.
Causes of Macular Edema
Macular edema can occur as a result of various underlying conditions or factors that contribute to the accumulation of fluid in the macula, which is the central part of the retina. Common causes of macular edema include:
- Diabetic Retinopathy: One of the most common causes of macular edema is diabetic retinopathy. High blood sugar levels in diabetes can damage the blood vessels in the retina, leading to leakage of fluid and the development of macular edema.
- Retinal Vein Occlusion (RVO): RVO occurs when a blood vessel that drains blood from the retina becomes blocked, causing blood and fluid to accumulate in the retina, including the macula.
- Uveitis: Uveitis is inflammation of the uvea, the middle layer of the eye. Inflammatory processes can lead to macular edema due to increased permeability of blood vessels.
- Age-Related Macular Degeneration (AMD): In some cases of wet AMD, abnormal blood vessel growth can lead to fluid leakage into the macula, resulting in macular edema.
- Cataract Surgery: Macular edema can be a complication of cataract surgery, particularly in individuals with pre-existing risk factors.
- Vascular Diseases: Conditions such as hypertension (high blood pressure) and vascular diseases can affect the blood vessels in the retina, potentially leading to macular edema.
- Inherited Disorders: Some inherited retinal disorders can predispose individuals to macular edema.
- Medications: Certain medications, such as corticosteroids, may increase the risk of developing macular edema, especially when taken for extended periods.
- Eye Injuries or Trauma: Traumatic injuries to the eye can cause inflammation and fluid leakage in the macula, resulting in macular edema.
- Infection: Eye infections, although less common, can lead to macular edema if they affect the retina.
It’s essential to identify and address the underlying cause of macular edema to determine the most appropriate treatment and management strategies. Early diagnosis and intervention are crucial in preserving vision and preventing further damage to the macula.
Comparison Table of Macular Degeneration and Macular Edema
Here’s a comparison table highlighting the key differences between macular degeneration and macular edema:
| Aspect | Macular Degeneration | Macular Edema |
|---|---|---|
| Definition | Progressive eye condition characterized by the deterioration of the macula, leading to central vision loss. | Accumulation of fluid in the macula, causing blurred or distorted central vision. |
| Primary Cause | Often associated with aging. | Can result from various underlying conditions, including diabetes, retinal vein occlusion, uveitis, and others. |
| Types | Dry macular degeneration (more common) and wet macular degeneration (less common). | Occurs as a complication of other eye diseases or conditions. |
| Symptoms | Gradual central vision loss, distorted vision, difficulty reading, dark spots in vision. | Blurred or distorted central vision, difficulty reading, visual distortions, and color perception changes. |
| Diagnosis | Comprehensive eye examination, retinal imaging (OCT, fundus photography), and visual acuity tests. | Eye examination, retinal imaging, and identification of underlying causes through medical history and tests. |
| Treatment Options | Lifestyle modifications, anti-VEGF injections (for wet AMD), dietary supplements (for dry AMD). | Intravitreal injections (anti-VEGF or corticosteroids), laser therapy, addressing underlying causes. |
| Prognosis | Vision loss is progressive and permanent, particularly in advanced stages. | Prognosis varies depending on the underlying condition and effectiveness of treatment. Timely intervention is crucial. |
| Prevalence | Common in individuals over 50, particularly Caucasians. | Occurs in association with underlying conditions and diseases, so prevalence varies with the specific cause. |
| Preventive Measures | Lifestyle modifications (e.g., healthy diet, not smoking) and regular eye exams for early detection. | Managing underlying conditions (e.g., diabetes, hypertension) and seeking prompt treatment for related eye issues. |
Both macular degeneration and macular edema can lead to significant visual impairment, and early diagnosis and appropriate treatment are essential for preserving vision and improving the quality of life for affected individuals.
Diagnosis and Screening

Diagnosis and screening for macular degeneration and macular edema involve various clinical tests and procedures conducted by eye care professionals. Here’s an overview of the diagnostic and screening methods for these conditions:
Diagnosis of Macular Degeneration:
-
- Comprehensive Eye Examination: An eye doctor will conduct a thorough eye exam, including assessing visual acuity, examining the retina, and checking for signs of macular degeneration.
- Dilated Fundus Examination: The pupil is dilated with eye drops, allowing the doctor to examine the macula and the retina in detail. This helps in identifying drusen (small yellow deposits) and other abnormalities.
- Amsler Grid Test: Patients may be asked to look at an Amsler grid, which is a pattern of straight lines, to detect distortions or missing areas in their central vision.
- Fluorescein Angiography (for wet AMD): In cases where wet AMD is suspected, a fluorescent dye is injected into a vein in the arm. The dye highlights blood vessels in the retina and helps identify abnormal vessel growth and leakage.
- Optical Coherence Tomography (OCT): This non-invasive imaging test provides high-resolution cross-sectional images of the retina, allowing the doctor to assess the thickness of the macula and detect fluid buildup in the retina.
Diagnosis of Macular Edema:
-
- Comprehensive Eye Examination: Similar to macular degeneration, a thorough eye exam is conducted to assess visual acuity, examine the retina, and identify signs of macular edema.
- Dilated Fundus Examination: As with macular degeneration, dilating the pupil enables a detailed examination of the macula and retina.
- Optical Coherence Tomography (OCT): OCT is a critical tool for diagnosing macular edema, as it provides clear images of the macula and helps measure the thickness of the macular region, which can be indicative of edema.
- Fluorescein Angiography (in some cases): If the underlying cause of macular edema is unclear or if further assessment is needed, fluorescein angiography may be performed to identify vascular abnormalities.
Screening:
-
- Regular Eye Examinations: Routine eye check-ups with an eye care professional are essential for early detection of both macular degeneration and macular edema, especially in individuals at higher risk (e.g., older adults, diabetics).
- Amsler Grid (for macular degeneration): Some individuals at risk for macular degeneration may use an Amsler grid at home to monitor their central vision regularly.
- Disease-Specific Screening: Individuals with conditions like diabetes should undergo regular eye screenings to detect diabetic retinopathy, a common cause of macular edema.
- Genetic Testing (in some cases): Genetic testing may be considered for individuals with a strong family history of macular degeneration to assess their risk.
Early diagnosis and intervention are crucial for managing these conditions effectively, as timely treatment can help slow the progression of macular degeneration and address the underlying causes of macular edema.
Treatment Options
Treatment options for macular degeneration and macular edema depend on the specific type of condition and its underlying causes. Here’s an overview of the treatment options for both conditions:
Treatment Options for Macular Degeneration:
- Dry Macular Degeneration:
- Lifestyle Modifications: Patients are advised to make healthy lifestyle choices, including a diet rich in antioxidants and omega-3 fatty acids, not smoking, and managing underlying health conditions like hypertension.
- Nutritional Supplements: Some individuals with intermediate to advanced dry AMD may benefit from specific dietary supplements, such as the Age-Related Eye Disease Study (AREDS) formula, which contains vitamins and minerals like vitamin C, vitamin E, zinc, and copper.
- Regular Monitoring: Close monitoring of the condition through regular eye exams is essential to detect any progression to the wet form.
- Wet Macular Degeneration:
- Intravitreal Injections: Anti-VEGF (vascular endothelial growth factor) medications, such as ranibizumab (Lucentis) or aflibercept (Eylea), are injected directly into the eye to inhibit abnormal blood vessel growth and reduce fluid leakage.
- Laser Therapy: In some cases, laser photocoagulation or photodynamic therapy may be used to seal or destroy abnormal blood vessels in wet AMD.
- Implantable Devices: Some implantable devices, like the Port Delivery System, are designed to continuously release anti-VEGF medication within the eye.
Treatment Options for Macular Edema:
- Underlying Condition Management:
- Treating the underlying cause of macular edema is crucial. For example, in diabetic macular edema (DME), optimizing blood sugar control is essential.
- Managing conditions like hypertension or uveitis can also help reduce macular edema.
- Intravitreal Injections:
- Anti-VEGF injections, such as ranibizumab (Lucentis), bevacizumab (Avastin), or aflibercept (Eylea), are commonly used to reduce vascular leakage and fluid accumulation in the macula.
- Corticosteroids:
- Intravitreal corticosteroid injections, such as dexamethasone (Ozurdex) or fluocinolone (Iluvien), can reduce inflammation and swelling in the macula.
- Laser Therapy:
- Focal laser photocoagulation may be used to seal leaking blood vessels in conditions like diabetic retinopathy.
- Surgical Interventions:
- In some cases of chronic or severe macular edema, surgical procedures like vitrectomy may be considered to remove the vitreous gel and allow for better access to the macula.
Treatment plans are individualized based on the patient’s specific condition, its severity, and other factors. The goal of treatment is to stabilize or improve vision, reduce fluid accumulation, and prevent further damage to the macula. Regular follow-up appointments with an eye care specialist are essential to monitor progress and adjust treatment as needed.
Preventing Macular Degeneration and Macular Edema
Preventing macular degeneration and macular edema primarily involves adopting healthy lifestyle practices and managing risk factors associated with these eye conditions. While prevention cannot guarantee complete immunity, it can significantly reduce the risk and slow the progression of these conditions.
Here are some preventive measures:
Preventing Macular Degeneration:
-
- Healthy Diet: Consume a diet rich in antioxidants, vitamins (A, C, E), minerals (zinc, copper), and omega-3 fatty acids. Foods like leafy greens, colorful fruits and vegetables, fish, and nuts are beneficial.
- Maintain a Healthy Weight: Obesity is a risk factor for macular degeneration, so maintaining a healthy weight through regular exercise and a balanced diet can help reduce the risk.
- Quit Smoking: Smoking is a significant modifiable risk factor for macular degeneration. Quitting smoking can substantially lower your risk.
- Eye Protection: Protect your eyes from harmful UV light by wearing sunglasses that block both UVA and UVB rays when outdoors.
- Regular Eye Exams: Schedule regular eye examinations, especially if you have a family history of macular degeneration or are over the age of 50. Early detection can lead to earlier intervention.
- Manage Cardiovascular Health: Control high blood pressure, cholesterol levels, and other cardiovascular risk factors to reduce the risk of developing macular degeneration.
- Limit Alcohol Consumption: Excessive alcohol consumption may increase the risk, so limit alcohol intake.
Preventing Macular Edema:
-
- Manage Underlying Conditions: For conditions like diabetes or hypertension, carefully manage your health through proper medication, diet, and lifestyle choices.
- Control Blood Sugar: If you have diabetes, maintaining stable blood sugar levels can help prevent diabetic retinopathy and associated macular edema.
- Regular Eye Exams: Diabetic patients should undergo regular eye screenings to detect diabetic retinopathy and macular edema early.
- Medication Management: If you are on medications that could increase the risk of macular edema, consult with your healthcare provider about potential alternatives or monitoring.
- Eye Protection: Protect your eyes from injury or trauma, which can increase the risk of macular edema.
- Quit Smoking: Smoking is a risk factor for various eye conditions, including macular edema. Quitting smoking can reduce this risk.
- Nutrition: Consume a balanced diet rich in nutrients that support eye health, including those with antioxidants and omega-3 fatty acids.
- Maintain a Healthy Lifestyle: Engage in regular physical activity, maintain a healthy weight, and manage stress.
Preventive measures should be personalized to your specific health status and risk factors. Consult with an eye care specialist and other healthcare professionals to develop a comprehensive plan for reducing your risk of macular degeneration and macular edema.
The Future of Macular Disease Research
The future of macular disease research holds significant promise, with ongoing advancements in technology, genetics, and our understanding of the underlying mechanisms of these conditions.
Here are some key areas and developments to look forward to in the field of macular disease research:
- Genetic Research: Advances in genetics and genomics are helping researchers identify specific genes and genetic factors associated with macular degeneration and macular edema. This knowledge may lead to personalized treatments and targeted therapies.
- Early Detection: Improved screening techniques, such as artificial intelligence (AI)-assisted imaging and genetic testing, may allow for earlier and more accurate detection of macular diseases, enabling timely intervention and better outcomes.
- Disease Mechanisms: Continued research into the molecular and cellular mechanisms underlying macular diseases will provide insights into disease progression and potential therapeutic targets.
- Stem Cell Therapies: Stem cell research holds promise for regenerative treatments that could repair damaged retinal tissue in conditions like macular degeneration. Clinical trials are exploring the safety and efficacy of these therapies.
- Drug Development: Ongoing pharmaceutical research is focused on developing new medications and treatment approaches, including longer-lasting anti-VEGF drugs and alternative therapeutic pathways to manage macular diseases.
- Gene Therapy: Experimental gene therapies aim to correct or replace faulty genes associated with macular diseases. Early successes in clinical trials suggest the potential for gene therapy as a treatment option.
- Drug Delivery Systems: Researchers are working on innovative drug delivery methods, such as sustained-release implants and nanoparticle-based treatments, to enhance the effectiveness of therapies and reduce the need for frequent injections.
- Patient Outcomes and Quality of Life: Research is not limited to medical treatments; it also includes studies on the psychological and social impacts of macular diseases and ways to improve patients’ quality of life through support and rehabilitation services.
- Telemedicine and Remote Monitoring: Advances in telemedicine and remote monitoring technologies are making it easier for patients to receive ongoing care and for researchers to collect real-time data on disease progression.
- Global Collaboration: International collaboration and data sharing among researchers are accelerating progress in understanding and treating macular diseases.
- Patient Advocacy and Awareness: Increased awareness and patient advocacy efforts are helping drive research funding, support, and resources to further advance the field.
The future of macular disease research is multidisciplinary, involving ophthalmologists, geneticists, bioengineers, data scientists, and many others. As our knowledge deepens and technology evolves, we can anticipate more effective treatments, earlier interventions, and improved outcomes for individuals affected by macular degeneration and macular edema.
Final Opinion
Macular Degeneration and Macular Edema are significant eye conditions that can have a profound impact on vision. Macular degeneration, primarily age-related, results in gradual central vision loss, while macular edema involves fluid accumulation in the macula, causing blurred or distorted central vision.
Early diagnosis and appropriate management, including lifestyle modifications, medications, and surgical interventions, are vital in preserving vision and improving the quality of life for affected individuals. Ongoing research and advancements in genetics, treatment options, and early detection methods offer hope for better outcomes and a brighter future in the battle against these eye diseases.