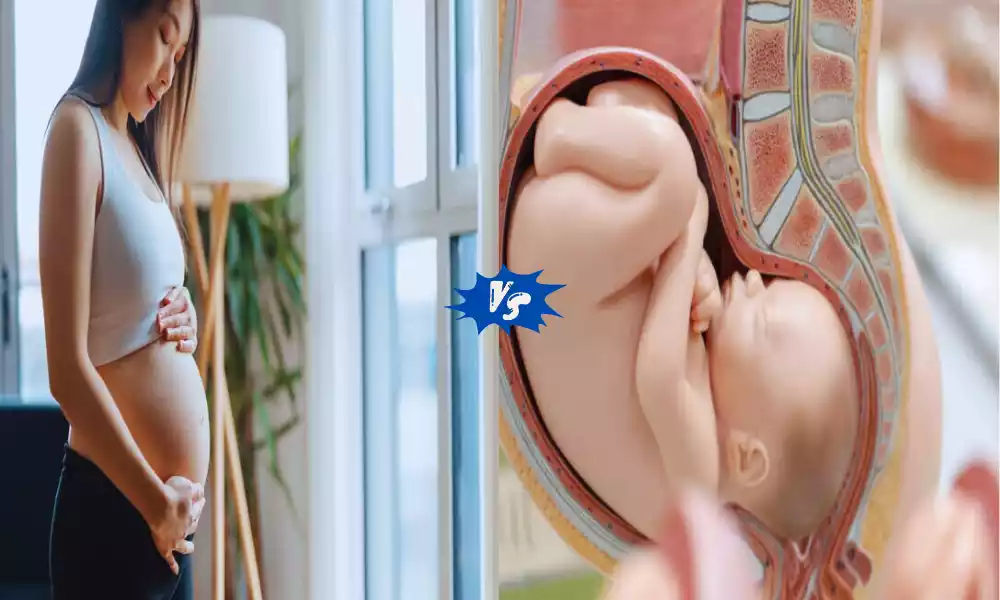
Polyhydramnios and Oligohydramnios are two distinct conditions that affect pregnant women and the development of their unborn babies. Polyhydramnios involves an excessive accumulation of amniotic fluid in the womb, while oligohydramnios is characterized by a deficiency of amniotic fluid. Both conditions can have significant implications for the course of pregnancy and require careful monitoring and medical attention to ensure the health and well-being of both mother and baby.
What is Polyhydramnios?
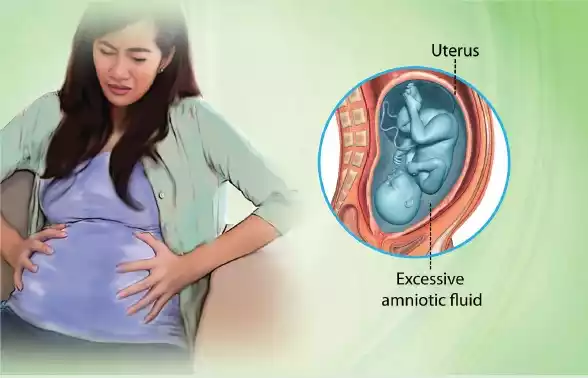
Polyhydramnios is a medical condition that occurs during pregnancy and is char Comparison Table of Polyhydramnios and Oligohydramniosacterized by an excessive accumulation of amniotic fluid within the amniotic sac. Amniotic fluid is the clear, watery fluid that surrounds and protects the developing fetus in the womb. This condition results in an abnormally high volume of amniotic fluid, which can lead to various maternal and fetal complications if not properly managed.
Polyhydramnios is typically diagnosed through ultrasound examinations and measurements of the amniotic fluid index (AFI). It is important for healthcare providers to monitor and address polyhydramnios to ensure the health and well-being of both the pregnant individual and the developing fetus.
Causes of Polyhydramnios
Polyhydramnios, characterized by an excessive accumulation of amniotic fluid during pregnancy, can result from various underlying causes. These causes can be grouped into different categories, including maternal, fetal, and idiopathic (unknown).
Some common causes and contributing factors of polyhydramnios include:
- Fetal Anomalies: Certain fetal abnormalities can affect the production and absorption of amniotic fluid. Conditions such as gastrointestinal obstructions, congenital malformations (e.g., neural tube defects), or chromosomal abnormalities may lead to polyhydramnios.
- Maternal Diabetes: Pregnant individuals with diabetes, particularly poorly controlled diabetes, may develop polyhydramnios. Elevated blood sugar levels can lead to increased fetal urine production, which contributes to higher amniotic fluid levels.
- Twin or Multiple Pregnancy: Polyhydramnios is more common in pregnancies with twins, triplets, or higher-order multiples. This is often due to the increased urine output of multiple fetuses.
- Fetal Hydrops: Fetal hydrops refers to an abnormal accumulation of fluid within the fetal body, which can increase amniotic fluid levels.
- Fetal Heart or Lung Problems: Some cardiac and pulmonary conditions in the developing fetus can disrupt the normal balance of amniotic fluid. For example, congenital heart defects or conditions that affect fetal lung development may lead to polyhydramnios.
- Infections: Certain maternal infections, such as parvovirus B19, can affect the fetal blood production and lead to polyhydramnios.
- Placental Issues: Conditions that affect the placenta’s ability to regulate amniotic fluid levels, such as placental tumors or vascular abnormalities, can contribute to polyhydramnios.
- Idiopathic: In some cases, the cause of polyhydramnios remains unknown, and it is classified as idiopathic polyhydramnios.
- Medications: Rarely, certain medications taken by the pregnant individual may be associated with increased amniotic fluid levels.
- Polyhydramnios in a Previous Pregnancy: If a person had polyhydramnios in a previous pregnancy, they may be at a slightly higher risk of developing it again in subsequent pregnancies.
It is essential for healthcare providers to identify the underlying cause of polyhydramnios as treatment and management may vary depending on the specific contributing factors. Regular monitoring and appropriate medical care are crucial to ensure the health and well-being of both the pregnant individual and the developing fetus.
Symptoms of Polyhydramnios
Polyhydramnios, characterized by an excessive accumulation of amniotic fluid during pregnancy, may manifest with various symptoms and signs. It’s important to note that some individuals with polyhydramnios may not experience noticeable symptoms, and the condition is often detected through routine prenatal screening.
When symptoms do occur, they may include:
- Abdominal Discomfort: Pregnant individuals with polyhydramnios may experience increased abdominal pressure and discomfort. This can make it challenging to move or find a comfortable position for sleep.
- Rapid Abdominal Growth: The uterus may enlarge at a faster rate than expected for the gestational age of the pregnancy. This rapid abdominal growth can be a visible sign to healthcare providers.
- Shortness of Breath: The excess amniotic fluid can push the diaphragm upward, making it more difficult for the pregnant person to breathe comfortably. This may be especially noticeable when lying down.
- Swelling (Edema): Swelling of the hands and feet, known as edema, may occur due to the increased pressure on blood vessels caused by the enlarged uterus.
- Heartburn and Indigestion: The enlarged uterus can exert pressure on the stomach, leading to an increased likelihood of heartburn and indigestion.
- Frequent Urination: The enlarged uterus can also put pressure on the bladder, causing more frequent urination.
- Fetal Movement: Some individuals with polyhydramnios report feeling increased fetal movements or fluttering sensations. This can be due to the extra space for the fetus to move around within the amniotic sac.
- Backache and Pelvic Pain: The additional weight and pressure in the abdominal area may lead to backache and pelvic discomfort.
It’s important to keep in mind that while these symptoms can be associated with polyhydramnios, they are not specific to this condition and may also occur in normal pregnancies. Diagnosis of polyhydramnios is typically confirmed through ultrasound and amniotic fluid index (AFI) measurements, as well as a thorough evaluation by healthcare providers.
If polyhydramnios is suspected or diagnosed, it is essential for pregnant individuals to receive appropriate prenatal care and monitoring, as the condition can be associated with potential complications for both the mother and the developing fetus.
Impact on Pregnancy
Polyhydramnios, which is characterized by an excessive accumulation of amniotic fluid during pregnancy, can have several impacts on both the pregnant individual and the developing fetus. These impacts may vary in severity depending on the underlying cause, the level of excess fluid, and the gestational age at which polyhydramnios is diagnosed.
Here are some of the potential impacts of polyhydramnios on pregnancy:
- Maternal Impact:
- Discomfort: Polyhydramnios can cause significant abdominal discomfort, making it challenging for the pregnant individual to move, sleep, or engage in daily activities comfortably.
- Shortness of Breath: The enlarged uterus due to excess amniotic fluid can push against the diaphragm, leading to shortness of breath, particularly when lying down.
- Increased Risk of Preterm Labor: In some cases, polyhydramnios may increase the risk of preterm labor and delivery.
- Potential Complications: Pregnant individuals with polyhydramnios may be at a slightly higher risk of experiencing complications such as placental abruption or postpartum hemorrhage.
- Fetal Impact:
- Fetal Distress: Excessive amniotic fluid can put pressure on the fetus, potentially leading to fetal distress during labor.
- Malpresentation: The increased fluid can allow the fetus to move into a less favorable presentation for delivery, such as breech or transverse positions.
- Cord Prolapse: There is an increased risk of the umbilical cord slipping into the birth canal before the baby (cord prolapse), which is a medical emergency.
- Respiratory Distress: In severe cases, polyhydramnios can be associated with an increased risk of the baby developing respiratory distress syndrome after birth.
- Monitoring and Management:
- Regular Monitoring: Pregnant individuals with polyhydramnios will typically require more frequent prenatal check-ups and ultrasounds to monitor both maternal and fetal well-being.
- Amnioreduction: In some cases of severe polyhydramnios, a procedure called amnioreduction may be performed to remove excess amniotic fluid. This can help alleviate some of the symptoms and reduce the risk of complications.
- Management of Underlying Causes: If a specific underlying cause of polyhydramnios is identified (e.g., gestational diabetes or fetal anomalies), it will be addressed as part of the overall management plan.
It’s important to emphasize that the management of polyhydramnios should be tailored to the individual’s unique circumstances and the severity of the condition. Close communication with healthcare providers is crucial to ensure appropriate care and monitoring throughout the pregnancy to minimize potential risks and complications. Early detection and management are key to optimizing the outcomes for both the pregnant individual and the baby.
What is Oligohydramnios?
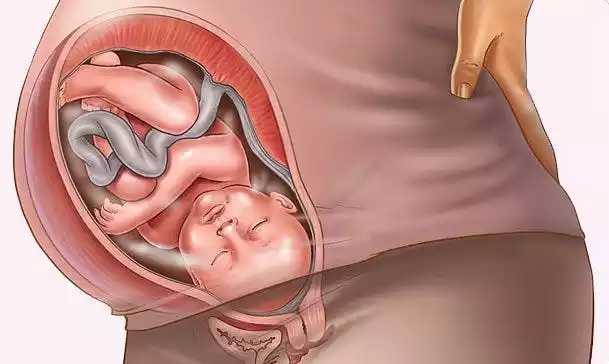
Oligohydramnios is a medical condition that occurs during pregnancy and is characterized by a deficiency or a lower-than-normal amount of amniotic fluid within the amniotic sac. Amniotic fluid is the clear, watery fluid that surrounds and protects the developing fetus in the womb. This condition results in an abnormally low volume of amniotic fluid, which can lead to various maternal and fetal complications if not properly managed.
Oligohydramnios is typically diagnosed through ultrasound examinations and measurements of the amniotic fluid index (AFI). It is important for healthcare providers to monitor and address oligohydramnios to ensure the health and well-being of both the pregnant individual and the developing fetus.
Causes of Oligohydramnios
Oligohydramnios is a condition characterized by a deficiency or lower-than-normal levels of amniotic fluid during pregnancy. Several factors and underlying causes can contribute to the development of oligohydramnios.
These causes may vary in severity and may include:
- Rupture of Membranes (PROM): One of the most common causes of oligohydramnios is the premature rupture of membranes, often referred to as PROM. When the amniotic sac (membranes) breaks before the onset of labor, it can lead to a gradual loss of amniotic fluid, resulting in reduced levels.
- Post-Term Pregnancy: In pregnancies that extend beyond the normal term (42 weeks or more), the amniotic fluid volume may decrease naturally as the fetus matures and swallows more fluid.
- Fetal Kidney Dysfunction: The production and regulation of amniotic fluid depend on fetal urine production. If there is a problem with the fetal kidneys or urinary tract, it can lead to reduced urine output, resulting in oligohydramnios.
- Placental Insufficiency: Conditions that affect the placenta’s function, such as placental abruption or placental infarcts, can disrupt the flow of nutrients and oxygen to the fetus. This can, in turn, affect fetal urine production and result in oligohydramnios.
- Maternal Dehydration: Maternal dehydration can lead to decreased blood flow to the uterus, which can affect the circulation of amniotic fluid to the fetus.
- Hypertension (High Blood Pressure): Certain maternal conditions, such as chronic hypertension or preeclampsia, can impact blood flow to the uterus and reduce amniotic fluid levels.
- Fetal Growth Restriction (IUGR): In cases of intrauterine growth restriction (IUGR), where the fetus is not growing at the expected rate, there may be a decreased production of urine and, consequently, lower amniotic fluid levels.
- Maternal Diabetes: While uncontrolled diabetes can lead to polyhydramnios (excessive amniotic fluid), well-controlled diabetes may lead to oligohydramnios due to decreased fetal urine output.
- Fetal Urinary Tract Abnormalities: Structural abnormalities in the fetal urinary tract, such as kidney malformations or urinary obstructions, can hinder normal urine production and contribute to oligohydramnios.
- Multiple Pregnancy: In twin or multiple pregnancies, there may be a higher risk of oligohydramnios due to increased competition for amniotic fluid among the fetuses.
- Chronic Hypoxia (Lack of Oxygen): Conditions that lead to chronic hypoxia in the fetus, such as maternal smoking or certain medical conditions, can result in reduced fetal urine production and, subsequently, oligohydramnios.
The severity of oligohydramnios and its impact on pregnancy can vary widely depending on the underlying cause and when it occurs during pregnancy. Timely diagnosis, close monitoring, and appropriate management are crucial to address the specific cause and mitigate potential risks to both the pregnant individual and the developing fetus.
Symptoms of Oligohydramnios
Oligohydramnios is a condition characterized by a deficiency or lower-than-normal levels of amniotic fluid during pregnancy. It may not always present with noticeable symptoms, and the diagnosis is often made through prenatal screening and ultrasound examinations. When symptoms do occur or when oligohydramnios becomes severe, it can be associated with various signs and complications.
Here are some potential symptoms and signs of oligohydramnios:
- Reduced Fetal Movement: Pregnant individuals with oligohydramnios may notice decreased fetal movements. This can be a significant concern and should be reported to a healthcare provider promptly.
- Measuring Small for Gestational Age: When the amniotic fluid levels are low, the uterus may not grow as expected for the gestational age of the pregnancy. This can result in the pregnant person measuring smaller than anticipated.
- Dehydration and Thirst: Oligohydramnios can sometimes be associated with maternal dehydration, leading to increased thirst and dry mouth. Dehydration can further exacerbate the condition.
- Decreased Urinary Frequency: Some individuals with oligohydramnios may experience reduced urinary frequency as a result of decreased amniotic fluid levels.
- Compression of the Umbilical Cord: Severe oligohydramnios can increase the risk of the umbilical cord becoming compressed or compressed between the fetus and the uterine wall. This can compromise the fetus’s oxygen and nutrient supply, leading to fetal distress.
- Potential Complications: Oligohydramnios can be associated with various complications, including an increased risk of preterm birth, meconium-stained amniotic fluid (indicating fetal distress), and intrauterine growth restriction (IUGR) in the fetus.
- Breathing Problems for the Baby: In severe cases, oligohydramnios can contribute to underdeveloped fetal lungs, increasing the risk of respiratory distress syndrome (RDS) in the newborn.
While some of these symptoms may be associated with oligohydramnios, they are not specific to this condition and can also be attributed to other factors in pregnancy. Therefore, a definitive diagnosis of oligohydramnios is typically made through ultrasound assessments, particularly the measurement of the amniotic fluid index (AFI).
Pregnant individuals who suspect they may have oligohydramnios or are experiencing changes in fetal movements or other concerning symptoms should seek immediate medical attention. Early detection and appropriate management are crucial to ensuring the health and well-being of both the pregnant person and the developing fetus.
Impact on Pregnancy
Oligohydramnios, a condition characterized by lower-than-normal levels of amniotic fluid during pregnancy, can have several significant impacts on both the pregnant individual and the developing fetus. The effects of oligohydramnios may vary depending on the severity of the condition, the underlying causes, and when it occurs during pregnancy.
Here are some of the potential impacts of oligohydramnios on pregnancy:
Maternal Impact:
- Maternal Discomfort: Oligohydramnios can cause discomfort and abdominal pain for the pregnant individual due to the decreased cushioning effect of the amniotic fluid.
- Decreased Uterine Growth: The uterus may not grow as expected for the gestational age of the pregnancy, leading to concerns about fetal growth and development.
- Increased Risk of Complications: Pregnant individuals with oligohydramnios may be at a higher risk of experiencing complications such as preterm labor, preeclampsia, and placental abruption.
Fetal Impact:
- Fetal Distress: Oligohydramnios can lead to fetal distress during labor and delivery, as the reduced amniotic fluid may compress the umbilical cord and limit the fetus’s oxygen and nutrient supply.
- Intrauterine Growth Restriction (IUGR): In cases of severe or prolonged oligohydramnios, the fetus may experience reduced growth, known as intrauterine growth restriction (IUGR). This can result in lower birth weight and potential health issues for the newborn.
- Lung Development: Adequate amniotic fluid levels are essential for proper lung development in the fetus. Severe oligohydramnios can lead to underdeveloped fetal lungs, increasing the risk of respiratory distress syndrome (RDS) after birth.
- Musculoskeletal Deformities: In rare cases, oligohydramnios can result in musculoskeletal deformities due to the limited space for fetal movement and growth.
Monitoring and Management:
- Frequent Monitoring: Pregnant individuals with oligohydramnios require close monitoring by healthcare providers. This includes more frequent prenatal check-ups and ultrasounds to assess fetal well-being.
- Amnioinfusion: In some cases, a medical procedure called amnioinfusion may be performed during labor to add sterile fluid into the uterus, thereby increasing the amniotic fluid levels and reducing the risk of cord compression.
- Early Delivery: Depending on the severity of oligohydramnios and other associated factors, healthcare providers may recommend early induction of labor or cesarean section to ensure the safety of both the mother and the fetus.
It’s important to emphasize that the management of oligohydramnios should be individualized based on the specific circumstances of each pregnancy. Early detection, close monitoring, and timely intervention are critical to address the underlying causes and mitigate potential risks. Pregnant individuals diagnosed with oligohydramnios should work closely with their healthcare providers to ensure the best possible outcomes for both themselves and their newborns.
Comparison Table of Polyhydramnios and Oligohydramnios
Here’s a comparison table outlining the key differences between polyhydramnios and oligohydramnios in pregnancy:
| Characteristic | Polyhydramnios | Oligohydramnios |
|---|---|---|
| Amniotic Fluid Levels | Excessive amniotic fluid. | Insufficient amniotic fluid. |
| Diagnosis | Made through ultrasound and AFI measurement. | Made through ultrasound and AFI measurement. |
| Potential Symptoms | – Abdominal discomfort
– Rapid abdominal growth – Shortness of breath – Swelling (edema) – Heartburn and indigestion – Frequent urination – Increased fetal movements |
– Reduced fetal movements
– Measuring small for gestational age – Maternal discomfort – Potential complications |
| Impact on Pregnancy | – Maternal discomfort
– Potential complications – Fetal malpresentation – Cord compression – Potential preterm birth |
– Reduced fetal growth (IUGR)
– Increased risk of preterm labor – Potential fetal distress – Respiratory distress syndrome (RDS) – Musculoskeletal deformities (rare) |
| Monitoring | – Frequent prenatal check-ups
– Serial ultrasounds – Non-Stress Tests (NST) – Maternal evaluation |
– Frequent prenatal check-ups
– Serial ultrasounds – Non-Stress Tests (NST) – Maternal evaluation |
| Treatment and Management | – Address underlying causes
– Regular monitoring – Amnioreduction (if severe) – Manage maternal conditions – Maternal comfort measures |
– Address underlying causes
– Regular monitoring – Amnioinfusion (if severe) – Address maternal dehydration – Consider timing of delivery – Address maternal conditions |
Diagnosis and Monitoring of Polyhydramnios and Oligohydramnios
Diagnosis and monitoring of both polyhydramnios (excessive amniotic fluid) and oligohydramnios (deficient amniotic fluid) are essential components of prenatal care to ensure the health and well-being of both the pregnant individual and the developing fetus.
Here’s an overview of the diagnostic and monitoring processes for these two conditions:
Diagnosis of Polyhydramnios:
- Clinical Assessment: The diagnosis of polyhydramnios may be suspected based on clinical signs and symptoms, such as maternal discomfort, abdominal distention, or difficulty breathing. The healthcare provider will inquire about these symptoms during routine prenatal check-ups.
- Ultrasound Examination: The primary method for diagnosing and quantifying polyhydramnios is through ultrasound examinations. Ultrasound allows healthcare providers to visualize the amniotic fluid volume and assess its adequacy. Key ultrasound parameters for diagnosing polyhydramnios include:
- Amniotic Fluid Index (AFI): AFI involves measuring the depth of amniotic fluid in different areas of the uterus to calculate the AFI. An AFI above a certain threshold is indicative of polyhydramnios.
- Single Deepest Pocket Measurement: This measurement assesses the deepest pocket of amniotic fluid. A single deep pocket measurement above a specific value may suggest polyhydramnios.
- Amniotic Fluid Volume Chart: Healthcare providers may refer to established amniotic fluid volume charts to determine whether the amniotic fluid levels fall within the expected range for gestational age.
Monitoring of Polyhydramnios:
- Regular Prenatal Check-ups: Pregnant individuals diagnosed with polyhydramnios will require more frequent prenatal check-ups to monitor the condition and assess fetal well-being.
- Ultrasound Monitoring: Serial ultrasound examinations are scheduled to monitor the amniotic fluid levels and assess fetal growth and well-being. These ultrasounds help healthcare providers track changes in amniotic fluid volume over time.
- Non-Stress Tests (NST): NSTs may be recommended to assess fetal heart rate patterns and monitor fetal well-being. These tests evaluate whether the fetus is experiencing distress due to polyhydramnios.
- Maternal Evaluation: Healthcare providers closely monitor the pregnant individual for signs of complications related to polyhydramnios, such as preterm labor or maternal discomfort.
- Management and Intervention: Depending on the severity of polyhydramnios and its underlying causes, healthcare providers will develop a management plan. This may involve addressing any contributing factors, such as gestational diabetes or fetal anomalies, and ensuring appropriate care throughout the remainder of the pregnancy.
Diagnosis of Oligohydramnios:
- Clinical Assessment: The diagnosis of oligohydramnios may be suspected based on clinical signs and symptoms, such as reduced fetal movements, maternal discomfort, or measuring smaller for gestational age. These symptoms should be reported to the healthcare provider.
- Ultrasound Examination: Oligohydramnios is primarily diagnosed through ultrasound assessments. Ultrasound allows healthcare providers to measure amniotic fluid levels using parameters like the Amniotic Fluid Index (AFI) or Single Deepest Pocket measurement.
Monitoring of Oligohydramnios:
- Regular Prenatal Check-ups: Pregnant individuals diagnosed with oligohydramnios will require more frequent prenatal check-ups to monitor the condition and assess fetal well-being.
- Ultrasound Monitoring: Serial ultrasound examinations are used to monitor amniotic fluid levels, assess fetal growth, and evaluate fetal well-being. Changes in amniotic fluid volume are closely tracked.
- Non-Stress Tests (NST): NSTs may be recommended to assess fetal heart rate patterns and monitor fetal well-being. These tests help healthcare providers assess whether the fetus is experiencing distress due to oligohydramnios.
- Management and Intervention: Healthcare providers develop a management plan based on the severity of oligohydramnios and its underlying causes. This may involve addressing factors such as maternal dehydration, fetal urinary tract abnormalities, or maternal conditions contributing to oligohydramnios.
Early detection, close monitoring, and timely intervention are essential to optimize outcomes for both the pregnant individual and the developing fetus. Pregnant individuals should maintain open communication with their healthcare providers and adhere to recommended monitoring and management plans.
Treatment and Management for Polyhydramnios and Oligohydramnios
The treatment and management of polyhydramnios (excessive amniotic fluid) and oligohydramnios (deficient amniotic fluid) are essential to address potential risks and ensure the well-being of both the pregnant individual and the developing fetus. The approach to treatment and management may vary depending on the severity of the condition, its underlying causes, and the gestational age at which it is diagnosed.
Here are guidelines for the treatment and management of polyhydramnios and oligohydramnios:
Treatment and Management of Polyhydramnios:
- Identify and Address Underlying Causes: The first step in managing polyhydramnios is to identify and address any underlying causes. This may involve assessing for fetal anomalies, maternal diabetes, multiple pregnancies, or other factors contributing to excessive amniotic fluid.
- Regular Monitoring: Pregnant individuals with polyhydramnios require close monitoring, including more frequent prenatal check-ups and ultrasounds to assess the amniotic fluid volume and fetal well-being.
- Amnioreduction: In severe cases of polyhydramnios, where there is a significant risk of complications, amnioreduction may be performed. This procedure involves removing excess amniotic fluid through amniocentesis. Amnioreduction can provide relief from maternal discomfort and reduce the risk of complications such as preterm labor or fetal malposition.
- Maternal Comfort: Measures to alleviate maternal discomfort, such as advising the pregnant individual to rest, use maternity support belts, or sleep with an elevated head, can help improve comfort during pregnancy.
- Manage Gestational Diabetes: If polyhydramnios is associated with gestational diabetes, proper management of blood sugar levels is crucial. This may include dietary changes, medication, or insulin therapy under the guidance of a healthcare provider.
- Monitoring for Fetal Anomalies: If fetal anomalies are detected, additional monitoring and consultations with specialists may be required to assess the severity and potential impact on the pregnancy.
Treatment and Management of Oligohydramnios:
- Identify and Address Underlying Causes: The management of oligohydramnios begins with identifying and addressing the underlying causes. This may involve evaluating for conditions such as rupture of membranes, fetal kidney dysfunction, placental insufficiency, or maternal dehydration.
- Frequent Monitoring: Pregnant individuals diagnosed with oligohydramnios require close monitoring, including more frequent prenatal check-ups, ultrasounds, and non-stress tests (NSTs) to assess fetal well-being.
- Amnioinfusion: In cases of severe oligohydramnios or if there is concern about cord compression during labor, amnioinfusion may be considered. This procedure involves adding sterile fluid into the amniotic cavity to increase amniotic fluid levels temporarily.
- Address Maternal Dehydration: If oligohydramnios is associated with maternal dehydration, rehydration and addressing the underlying cause of dehydration are essential.
- Consider Timing of Delivery: Depending on the severity of oligohydramnios and other associated factors, healthcare providers may recommend early induction of labor or cesarean section to ensure the safety of both the mother and the fetus.
- Address Maternal Conditions: In cases where maternal conditions contribute to oligohydramnios (e.g., maternal hypertension or preeclampsia), managing these conditions is essential to improve fetal well-being.
It’s crucial for pregnant individuals diagnosed with polyhydramnios or oligohydramnios to maintain open communication with their healthcare providers and adhere to recommended monitoring and management plans. Early detection and appropriate intervention are key to optimizing outcomes for both the pregnant individual and the developing fetus. The specific treatment plan will be tailored to the individual’s unique circumstances and the severity of the condition.
Summary
Polyhydramnios and Oligohydramnios are two conditions that underscore the complexity of pregnancy. While they represent opposite ends of the spectrum concerning amniotic fluid levels, both demand vigilant medical care and monitoring.
Early detection, timely intervention, and a supportive healthcare team can significantly improve outcomes for expectant mothers and their babies facing these challenges during pregnancy. Remember, prenatal care and open communication with healthcare providers are essential for a safe and healthy pregnancy journey.