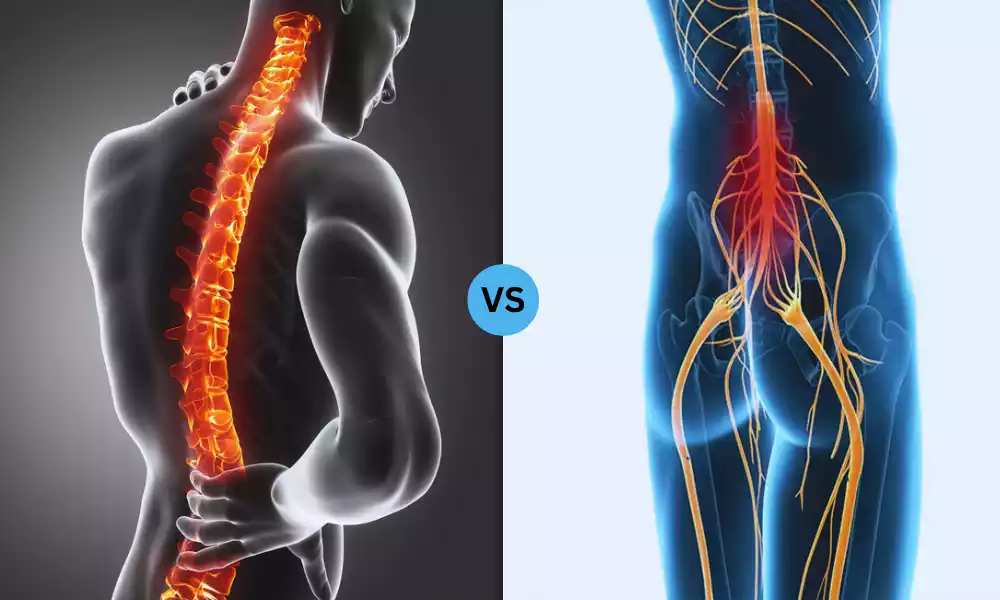
Paraplegia and Tetraplegia are two distinct forms of paralysis caused by spinal cord injuries. While both conditions result in loss of motor function and sensation, they differ in terms of affected body regions and functional limitations. Understanding the differences between paraplegia and tetraplegia is crucial for effective medical management, rehabilitation, and support for individuals living with these conditions.
Definition of Paraplegia

Paraplegia refers to a condition of paralysis that affects the lower half of the body, including the legs and, in some cases, the lower trunk. It results from damage to the spinal cord, which disrupts the normal communication between the brain and the affected body parts. This loss of motor function and sensory perception in the lower limbs is typically caused by trauma or disease affecting the spinal cord.
The severity and extent of paraplegia vary depending on the level of the spinal cord injury. The condition is categorized based on the specific region of the spinal cord that is impacted, which helps determine the extent of paralysis and the affected areas of the body.
Paraplegia can have profound effects on an individual’s mobility, independence, and overall quality of life. Rehabilitation and adaptive strategies play a crucial role in helping individuals with paraplegia regain functional abilities, enhance their self-care skills, and reintegrate into various aspects of daily life.
Type of Paraplegia
Paraplegia is categorized based on the specific level of the spinal cord where the injury occurs. The level of injury determines which parts of the body are affected by paralysis. The two main types of paraplegia are:
- Thoracic Paraplegia: In this type, the injury to the spinal cord occurs in the thoracic region, which is the upper part of the middle back. Thoracic paraplegia results in paralysis of the legs and possibly the lower trunk. The exact extent of paralysis depends on the specific thoracic vertebrae that are affected.
- Lumbar Paraplegia: Lumbar paraplegia is caused by an injury to the spinal cord in the lower back region, known as the lumbar region. This type of paraplegia leads to paralysis of the legs, and the level of paralysis varies based on the specific lumbar vertebrae that are damaged.
The differentiation between thoracic and lumbar paraplegia is important because the higher the level of injury along the spinal cord, the more extensive the paralysis tends to be. Additionally, the effects on bodily functions such as bowel, bladder control, and sexual function can also vary based on the injury level.
Causes of Paraplegia
Paraplegia is primarily caused by damage to the spinal cord, which disrupts the communication between the brain and the lower half of the body. This damage can result from various traumatic and non-traumatic factors. Some common causes of paraplegia include:
- Traumatic Spinal Cord Injury: Accidents such as car crashes, falls, sports-related injuries, and violence can lead to fractures, dislocations, or compression of the spinal cord, resulting in paraplegia.
- Diseases: Certain medical conditions, including spinal tumors, spinal cord infections (such as spinal abscess), multiple sclerosis, transverse myelitis, and spinal cord strokes, can cause damage to the spinal cord and lead to paraplegia.
- Spinal Cord Ischemia: Insufficient blood flow to the spinal cord, often due to conditions like aortic aneurysms or spinal artery thrombosis, can result in tissue damage and paraplegia.
- Spinal Cord Compression: Conditions like herniated discs, spinal stenosis (narrowing of the spinal canal), and spinal fractures can exert pressure on the spinal cord, causing damage and paralysis.
- Congenital Conditions: Some individuals are born with spinal cord abnormalities that can lead to paraplegia, such as spina bifida or tethered spinal cord.
- Autoimmune Disorders: Autoimmune diseases like Guillain-Barré syndrome and transverse myelitis can cause inflammation and damage to the spinal cord, leading to paraplegia.
- Vascular Issues: Issues like spinal cord infarction, where blood supply to the spinal cord is interrupted, can result in tissue death and paralysis.
- Surgical Complications: Surgical procedures involving the spine, if not performed correctly, can lead to damage of the spinal cord and subsequent paraplegia.
- Degenerative Conditions: Conditions like amyotrophic lateral sclerosis (ALS) or certain forms of hereditary spastic paraplegia can cause progressive damage to the spinal cord and result in paraplegia.
- Electric Shock or Radiation Exposure: Severe electric shock or exposure to high levels of radiation can damage the spinal cord and lead to paralysis.
It’s important to note that advancements in medical care and rehabilitation have improved the prognosis and quality of life for individuals with paraplegia. Effective treatment, supportive care, and adaptive techniques can help individuals with paraplegia manage their condition and regain functional independence to varying degrees.
Symptoms of Paraplegia
Paraplegia is characterized by a range of symptoms that result from the loss of motor function and sensory perception in the lower half of the body due to spinal cord injury. These symptoms can vary in intensity depending on the level and severity of the injury. Common symptoms of paraplegia include:
-
- Loss of Motor Function: Inability to move or control the legs and lower trunk due to disrupted signals between the brain and affected areas.
- Loss of Sensation: Reduced or absent feeling in the legs and lower body, making it difficult to perceive touch, pain, and temperature.
- Muscle Weakness: Muscles in the legs may become weak and atrophied due to lack of use and nerve connection.
- Spasticity: Uncontrolled muscle contractions and spasms can occur in the paralyzed areas, causing stiffness and discomfort.
- Changes in Reflexes: Reflexes in the legs, such as the knee-jerk reflex, may be altered or diminished.
- Bowel and Bladder Dysfunction: Paraplegia can lead to loss of control over bowel and bladder function, requiring the use of catheters or other methods for emptying.
- Sexual Dysfunction: Reduced sexual sensation and function can occur due to disrupted nerve pathways.
- Poor Circulation: Limited mobility and sensation can lead to circulatory issues, increasing the risk of blood clots and pressure sores.
- Skin Sensitivity: Decreased sensation can result in reduced awareness of pain and pressure, increasing the risk of skin injuries.
- Impaired Balance and Coordination: Individuals with paraplegia may have difficulty maintaining balance and coordinating movements.
- Changes in Body Temperature Regulation: The body’s ability to regulate temperature can be compromised due to disrupted neural control.
- Depression and Emotional Impact: The psychological impact of paraplegia can lead to depression, anxiety, and adjustment challenges.
- Challenges with Mobility: Walking and standing become impossible without assistive devices, and mobility may be achieved through wheelchairs or other aids.
- Loss of Independence: Tasks that require lower body movement, such as dressing, grooming, and bathing, can become challenging without adaptation.
It’s important to note that the extent of these symptoms can vary based on the individual’s injury level and severity. Comprehensive medical care, rehabilitation, and adaptive strategies are essential for managing these symptoms and improving the individual’s quality of life.
Definition of Tetraplegia

Tetraplegia, also known as quadriplegia, is a form of paralysis that affects both the upper and lower parts of the body due to a spinal cord injury. Individuals with tetraplegia experience varying degrees of motor and sensory impairment in their arms, hands, trunk, legs, and pelvic organs. This condition arises from damage to the spinal cord, disrupting the normal signals between the brain and the affected body regions.
The level of impairment in tetraplegia is determined by the location of the spinal cord injury. The higher the injury occurs along the spinal cord, the more extensive the paralysis tends to be. Tetraplegia is categorized based on the specific spinal segment affected, with different segments corresponding to different degrees of impairment and functional limitations.
People with tetraplegia face challenges in various aspects of daily life, including mobility, self-care, communication, and independent living. Rehabilitation, adaptive technologies, and assistive devices are vital components of managing tetraplegia and helping individuals regain as much functional independence as possible. These interventions aim to improve muscle strength, coordination, and skills necessary for performing essential activities and tasks.
Causes of Tetraplegia
Tetraplegia, also known as quadriplegia, is caused by damage to the spinal cord in the cervical region (neck area) of the spine. This damage disrupts the communication between the brain and the body, leading to paralysis of varying degrees in both the upper and lower extremities. Several factors can cause tetraplegia:
- Traumatic Spinal Cord Injury: Accidents such as car crashes, falls, sports injuries, and violence can result in fractures, dislocations, or compression of the cervical spinal cord, leading to tetraplegia.
- Diseases and Medical Conditions: Certain conditions like cervical spinal tumors, infections (such as spinal abscesses), multiple sclerosis, transverse myelitis, and other disorders affecting the cervical spine can cause damage and tetraplegia.
- Spinal Cord Ischemia: Insufficient blood flow to the cervical spinal cord, often due to conditions like aortic dissections or other vascular problems, can result in tissue damage and paralysis.
- Spinal Cord Compression: Conditions such as herniated cervical discs, spinal stenosis, and fractures in the cervical spine can put pressure on the spinal cord, leading to damage and tetraplegia.
- Congenital Conditions: Some individuals are born with conditions like congenital cervical spinal anomalies that can cause tetraplegia from an early age.
- Autoimmune Disorders: Autoimmune diseases like Guillain-Barré syndrome and transverse myelitis can lead to inflammation and damage in the cervical spinal cord, resulting in tetraplegia.
- Vascular Issues: Interruption of blood supply to the cervical spinal cord can cause tissue death and paralysis.
- Surgical Complications: Surgical procedures involving the cervical spine can lead to spinal cord damage if not performed correctly.
- Degenerative Conditions: Certain progressive neurological disorders, such as ALS, can affect the cervical spinal cord over time and lead to tetraplegia.
- Electric Shock or Radiation: Severe electric shocks or exposure to high levels of radiation can damage the cervical spinal cord and cause paralysis.
Due to the complexity of the cervical spinal cord and the central role it plays in controlling upper and lower body functions, damage in this region can have a significant impact on an individual’s mobility, independence, and overall quality of life.
Symptoms of Tetraplegia
Tetraplegia, also known as quadriplegia, is characterized by paralysis that affects both the upper and lower parts of the body due to a spinal cord injury in the cervical region. The symptoms of tetraplegia can vary in severity depending on the level and extent of the injury. Common symptoms include:
-
- Loss of Motor Function: Inability to move or control the arms, hands, legs, and trunk due to disrupted signals between the brain and affected areas.
- Loss of Sensation: Reduced or absent feeling in the arms, hands, legs, and trunk, making it difficult to perceive touch, pain, and temperature.
- Muscle Weakness: Muscles in the affected areas may become weak and atrophied due to lack of use and nerve connection.
- Spasticity: Uncontrolled muscle contractions and spasms can occur in the paralyzed areas, causing stiffness and discomfort.
- Changes in Reflexes: Reflexes in the arms and legs may be altered or diminished due to the spinal cord injury.
- Bowel and Bladder Dysfunction: Tetraplegia can lead to loss of control over bowel and bladder function, requiring the use of catheters or other methods for emptying.
- Respiratory Challenges: Depending on the level of injury, respiratory muscles may be affected, potentially leading to breathing difficulties and the need for respiratory support.
- Limited Mobility: Walking and fine motor skills become impossible without assistive devices, and mobility may be achieved through wheelchairs or other aids.
- Impaired Balance and Coordination: Individuals with tetraplegia may have difficulty maintaining balance and coordinating movements due to muscle weakness.
- Sexual Dysfunction: Reduced sexual sensation and function can occur due to disrupted nerve pathways.
- Temperature Regulation Issues: The body’s ability to regulate temperature can be compromised due to disrupted neural control.
- Depression and Emotional Impact: The psychological impact of tetraplegia can lead to depression, anxiety, and adjustment challenges.
- Challenges with Self-Care: Daily tasks such as dressing, grooming, and feeding may become challenging without adaptive techniques and devices.
- Communication Difficulties: Depending on the level of injury, speaking and other forms of communication may be affected.
- Loss of Independence: Tetraplegia can result in dependence on caregivers for various activities of daily living.
The specific symptoms experienced by individuals with tetraplegia depend on the precise location and severity of the spinal cord injury. Comprehensive medical care, rehabilitation, and assistive technologies play a crucial role in managing these symptoms and enhancing the individual’s quality of life.
Comparison Table of Paraplegia and Tetraplegia
Here’s a comparison table outlining the key differences between paraplegia and tetraplegia:
| Aspect | Paraplegia | Tetraplegia |
|---|---|---|
| Affected Regions | Lower body, including legs and possibly lower trunk | Both upper and lower body due to cervical injury |
| Functional Limits | Mobility challenges in lower body, some trunk | Extensive functional limitations in upper and lower |
| Level of Injury | Below cervical region (thoracic or lumbar) | Cervical region (uppermost part of the spine) |
| Mobility | Wheelchairs or mobility aids for lower body | Powered wheelchairs or assistive tech for movement |
| Self-Care | Adaptive techniques for tasks | Extensive assistance due to upper body paralysis |
| Respiratory Function | Generally not affected | Potential impact on respiratory muscles |
| Communication | Typically not affected | Communication may be affected if upper body paralyzed |
| Quality of Life | Challenges exist, often more independence | Greater limitations and reliance on caregivers |
| Rehabilitation | Focus on lower body function, mobility | Addresses upper and lower body, specialized adaptations |
| Independence | Often higher independence levels | Reliance on caregivers for many activities |
What are the similarities between Paraplegia and Tetraplegia?
Paraplegia and tetraplegia are both conditions resulting from spinal cord injuries that lead to paralysis. Despite their differences, there are several similarities between the two conditions:
- Spinal Cord Injury: Both conditions are caused by damage to the spinal cord, which disrupts the communication between the brain and the body, leading to loss of motor function and sensation.
- Functional Limitations: Both conditions result in significant functional limitations that impact mobility, self-care, and daily activities.
- Medical Management: Both paraplegia and tetraplegia require comprehensive medical care, including acute treatment of the initial injury, surgical interventions if necessary, and ongoing medical monitoring.
- Rehabilitation: Rehabilitation is a key component of managing both conditions. Physical therapy, occupational therapy, and other forms of rehabilitation help individuals regain as much independence and functional ability as possible.
- Assistive Technologies: Individuals with both paraplegia and tetraplegia benefit from various assistive technologies, such as wheelchairs, mobility aids, communication devices, and adaptive equipment designed to enhance their quality of life.
- Adaptive Techniques: Both conditions necessitate the learning and use of adaptive techniques to perform daily activities, such as transferring, dressing, grooming, and using assistive devices.
- Psychological Impact: Both paraplegia and tetraplegia can have a significant psychological impact, leading to feelings of depression, anxiety, and adjustment challenges.
- Caregiver Support: In both cases, individuals may require varying degrees of caregiver support, particularly for tasks that they are unable to perform independently.
- Community Inclusion: Individuals with both conditions often face challenges in terms of social inclusion and accessibility, prompting the need for awareness and advocacy efforts.
- Ongoing Research: Medical research and advancements in spinal cord injury treatment benefit individuals with both paraplegia and tetraplegia, offering hope for improved quality of life.
It’s important to recognize that each person’s experience with paraplegia or tetraplegia is unique, and the impact of these conditions can vary based on the individual’s injury level, personal resilience, and access to medical care and support.
Medical Management and Treatment Options
Medical Management and Treatment Options for Paraplegia and Tetraplegia:
- Acute Care: Immediate stabilization and assessment after injury.
- Surgery: If needed, surgical procedures to address spinal cord damage.
- Medications: Pain relief, muscle relaxants, spasticity management.
- Rehabilitation: Physical therapy for mobility, occupational therapy for daily tasks.
- Assistive Devices: Wheelchairs, braces, communication aids.
- Respiratory Support: Ventilation assistance for severe tetraplegia.
- Bowel and Bladder Management: Catheterization, bowel programs.
- Pain Management: Medications, therapies, interventions.
- Psychological Support: Counseling, therapy for emotional well-being.
- Pressure Ulcer Prevention: Techniques to prevent skin breakdown.
- Nutrition and Hydration: Proper diet and hydration for overall health.
- Education: Learn adaptive techniques, self-care strategies.
- Research Opportunities: Participation in studies for advancements.
- Multidisciplinary Team: Collaborative care involving various specialists.
Psychological and Social Considerations
The psychological and social aspects of living with paraplegia or tetraplegia are significant, as they can influence emotional well-being, relationships, and overall quality of life. Addressing these considerations is crucial to promoting holistic recovery and adaptation. Here’s an overview:
Psychological Considerations:
-
- Depression and Anxiety: Adjusting to life with paralysis can lead to depression, anxiety, and feelings of loss. Professional mental health support and counseling are important for coping.
- Body Image and Self-Esteem: Changes in physical appearance and abilities may impact self-esteem. Encouraging self-acceptance and offering peer support can help address body image concerns.
- Grief and Loss: Individuals may mourn the loss of their pre-injury abilities and lifestyle. Grieving is a natural process that should be acknowledged and supported.
- Stress Management: Learning effective stress management techniques can help individuals handle the challenges that come with their condition.
- Coping Strategies: Developing healthy coping strategies, such as mindfulness, meditation, and positive self-talk, can enhance emotional resilience.
- Identity Adjustment: Adapting to a new identity as someone with a disability can be challenging. Encouraging a sense of purpose and exploring new interests can help.
Social Considerations:
-
- Relationships: Family dynamics and relationships with friends and partners may change. Open communication, empathy, and education about the condition can help maintain healthy relationships.
- Social Isolation: Mobility limitations and accessibility issues can contribute to feelings of isolation. Encouraging social engagement and providing accessible environments are important.
- Stigma and Discrimination: People with disabilities may face stigma and discrimination. Advocacy efforts and raising awareness can help combat negative attitudes.
- Peer Support: Connecting with others who share similar experiences can provide emotional support and practical advice.
- Employment and Education: Returning to work or pursuing education may require adjustments. Providing accommodations and fostering inclusive environments can aid reintegration.
- Community Involvement: Encouraging participation in community activities and organizations can help individuals with disabilities feel connected and valued.
- Sexuality and Intimacy: Addressing questions about sexuality, relationships, and intimacy is crucial. Open communication and professional guidance can provide answers and support.
- Accessibility: Ensuring physical and social environments are accessible promotes inclusion and participation in various activities.
- Advocacy: Empowering individuals with paraplegia or tetraplegia to advocate for their rights and needs can lead to positive changes in society.
Both psychological and social aspects should be considered as part of a comprehensive care plan for individuals with paraplegia or tetraplegia. Collaborative efforts between medical professionals, mental health specialists, caregivers, and the individual themselves contribute to a well-rounded approach to addressing these considerations.
Ongoing Research and Advancements

Medical research and technological innovations are continually advancing the understanding and treatment of paraplegia and tetraplegia. These advancements aim to improve quality of life, enhance functional independence, and develop potential therapeutic interventions.
Here are some areas of ongoing research and advancements:
1. Neuroregeneration: Researchers are exploring ways to stimulate nerve regrowth and repair damaged spinal cord tissue, potentially restoring lost function.
2. Neuroprosthetics: Developments in brain-computer interfaces and neuroprosthetic devices are allowing individuals to control computers, robotic limbs, and other devices using their thoughts.
3. Exoskeletons: Wearable exoskeleton devices are being developed to enable individuals with paralysis to stand, walk, and regain some mobility.
4. Stem Cell Therapies: Research into stem cell transplantation and regenerative therapies aims to promote spinal cord healing and functional recovery.
5. Electrical Stimulation: Techniques like functional electrical stimulation (FES) are being refined to activate muscles and restore movement.
6. Neuromodulation: Approaches like epidural stimulation involve applying electrical currents to the spinal cord to enhance motor function.
7. Virtual Reality: Virtual reality and augmented reality are being used in rehabilitation to enhance therapy and functional recovery.
8. Robotics: Advancements in robotic technology are leading to more sophisticated robotic assistance for daily tasks and mobility.
9. Pharmacological Interventions: Researchers are investigating drugs that could mitigate secondary complications, promote nerve repair, or improve functional outcomes.
10. Neuroplasticity: Understanding the brain’s ability to rewire itself (neuroplasticity) is guiding interventions to optimize recovery and adaptability.
11. Gene Therapy: Gene-editing techniques hold promise for altering genes to encourage nerve regeneration and functional improvement.
12. Clinical Trials: Ongoing clinical trials assess the safety and efficacy of new treatments, offering participants opportunities to access cutting-edge therapies.
13. Neural Mapping: Advanced imaging techniques are helping researchers map neural connections, aiding in the development of interventions.
14. Advancements in Assistive Technology: Innovations in wheelchairs, communication devices, and mobility aids are enhancing accessibility and independence.
15. Brain-Machine Interfaces: Researchers are working on more advanced ways to connect the brain directly to external devices, enabling greater control.
16. Rehabilitation Techniques: Research into optimized rehabilitation protocols and neurorehabilitation strategies continues to evolve.
17. Patient-Centered Outcomes: Researchers are focusing on understanding individual needs and preferences to tailor treatments and interventions.
Ongoing research and advancements hold significant promise for individuals with paraplegia and tetraplegia. While not all breakthroughs immediately translate into widely available treatments, the continuous progress in various fields offers hope for improved outcomes and quality of life for those affected by spinal cord injuries.
Summary
Paraplegia and Tetraplegia are conditions resulting from spinal cord injuries that lead to paralysis in distinct parts of the body. Paraplegia affects the lower body, while tetraplegia affects both the upper and lower body due to injuries in different regions of the spine.
Both conditions present challenges in mobility, self-care, and emotional well-being. Advances in medical care, rehabilitation techniques, assistive technologies, and ongoing research are continually improving the quality of life for individuals living with these conditions. With a comprehensive and multidisciplinary approach, individuals with paraplegia and tetraplegia can regain independence, engage in their communities, and lead fulfilling lives.