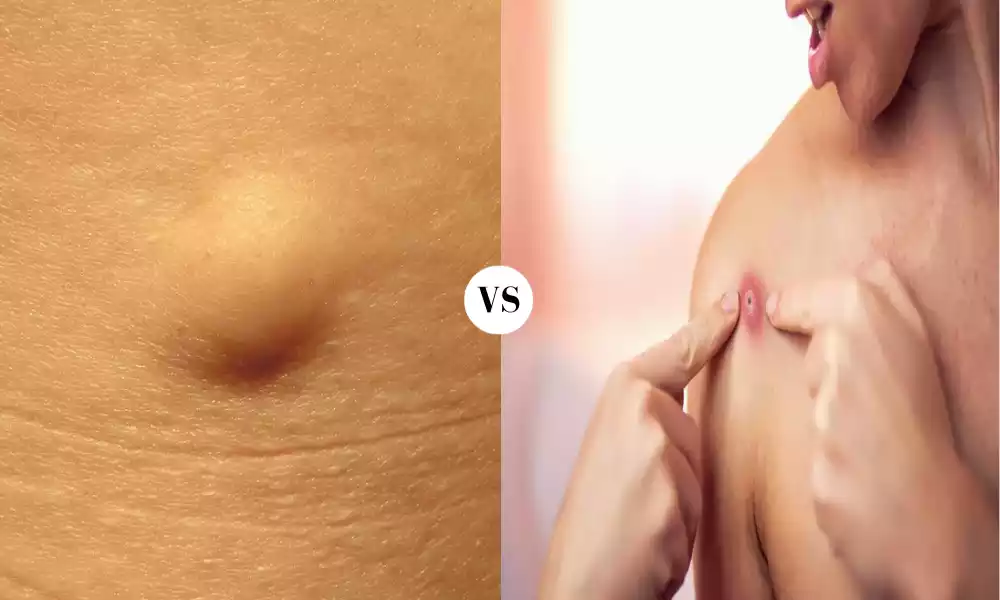
Cyst and Abscess are both palpable lesions that can occur within the body, but they stem from different causes and have distinct characteristics. A cyst is a closed sac-like structure, often filled with liquid, semi-solid, or gaseous material. It can be a result of various processes, including developmental anomalies, infections, or chronic inflammatory conditions, and might be benign or, in rarer cases, malignant.
An abscess is a localized collection of pus resulting from a bacterial infection. As an immune response, tissues produce antibodies as a means of stopping infectious materials from spreading throughout their bodies. Both conditions can manifest anywhere in the body and may require medical intervention depending on their size, location, and underlying cause.
What is a Cyst?
A cyst is a closed sac-like structure that can form in various parts of the body. It is distinguished by a distinct membrane and is often filled with liquid, semi-solid, or gaseous material.

Cysts can arise due to a variety of reasons, including:
- Developmental: Some cysts form during fetal development; these are called congenital cysts.
- Blockages: Blocked ducts or glands can lead to the formation of cysts. For instance, acne can lead to the development of epidermoid cysts due to blocked sebaceous glands.
- Infections: Certain infections can result in the formation of cysts, such as the parasitic infection echinococcosis which leads to hydatid cysts.
- Chronic Inflammation: Conditions involving long-term inflammation can sometimes give rise to cysts.
- Injuries: Trauma to a region might lead to cyst formation in some cases.
- Cellular Abnormalities: Abnormal cells can grow and replicate to form cysts.
- Tumors: Some benign or malignant tumors might have cystic components.
Cysts can be found in various regions of the body, including the skin, breasts, ovaries, kidneys, and liver, among others. While many cysts are benign, some can cause symptoms due to their size and location or may have the potential for malignancy. The approach to managing a cyst often depends on its type, location, size, and any associated symptoms. Some cysts might resolve on their own, while others may require drainage, medication, or surgical removal.
Common Types of Cysts
Cysts can develop in various parts of the body, and while some are common and benign, others might be rare or have the potential for malignancy. Here are some common types of cysts:
- Epidermoid Cyst (Sebaceous Cyst): Found in the skin, these are often caused by blocked hair follicles. They’re typically painless, slow-growing, and filled with keratin.
- Pilar Cyst: Originating from hair follicles, these cysts predominantly occur on the scalp. They’re filled with keratin and are generally benign.
- Ovarian Cyst: Women can develop fluid-filled sacs called ovarian cysts on or within their ovaries. Some common types include follicular cysts and corpus luteum cysts.
- Baker’s Cyst: Located behind the knee, this cyst forms due to the buildup of synovial fluid, often resulting from arthritis or a knee injury.
- Chalazion: Found on the eyelid, this cyst develops due to a blocked meibomian gland. It’s different from a stye, which is an infected eyelash follicle.
- Ganglion Cyst: Commonly forming on the wrist or hand, these cysts are filled with a jelly-like substance. Their cause isn’t always known, but they might arise from trauma or joint or tendon irritation.
- Cystic Acne: This severe form of acne arises from deep skin infections and can lead to large, red, and painful breakouts.
- Breast Cyst: Fluid-filled sacs that develop in breast tissue, they can feel like a lump and are often identified during routine mammograms.
- Renal Cyst: Found in the kidneys, these are typically filled with fluid. While solitary cysts are usually benign and cause no problems, polycystic kidney disease is a genetic disorder that results in numerous kidney cysts and can lead to kidney failure.
- Dentigerous Cyst: Associated with the crowns of unerupted teeth, this cyst forms in the jaw.
- Pilonidal Cyst: Located near the tailbone, these cysts can become infected and painful. They’re believed to result from a combination of friction and ingrown hairs.
- Bartholin’s Cyst: Forms when the duct of the Bartholin’s gland, located at the opening of the vagina, becomes blocked.
- Pancreatic Cyst: Located in the pancreas, these cysts can be benign or malignant. Some are filled with fluid, while others may contain solid materials.
It’s essential to consult a healthcare professional if you suspect you have a cyst. The appropriate treatment, monitoring, or removal approach will depend on the cyst’s type, size, and location.
Symptoms and Diagnosis
Cysts can present with a wide variety of symptoms depending on their size, location, and the tissues they affect. Here are the general symptoms and diagnostic approaches for cysts:
Symptoms:
- Lump or Bump: The most common symptom of a cyst is the formation of a palpable lump or bump under the skin or within an organ.
- Pain: Some cysts can be painful, especially if they rupture, become infected, or press against nerves.
- Skin Redness or Warmth: If a cyst becomes infected, the overlying skin may become red, warm, and tender to the touch.
- Discharge: Cysts, especially those on the skin, may rupture and release a thick, yellow, foul-smelling discharge.
- Fever: In the case of infected cysts, a person might also experience fever and general malaise.
- Impaired Function: Cysts in certain locations might impair the function of an organ. For instance, ovarian cysts might cause menstrual irregularities.
- Cosmetic Concern: Even if asymptomatic, a cyst might cause cosmetic concerns, especially if it’s large or located in a visible area.
Diagnosis:
- Physical Examination: A healthcare professional might start by physically examining the cyst, assessing its size, shape, and consistency.
- Medical History: Understanding the onset, duration, and any associated symptoms can help in diagnosing the type of cyst.
- Ultrasound: This imaging test can visualize the cyst and determine its size, location, and content (whether it’s fluid-filled, solid, or mixed).
- CT or MRI Scan: For cysts located deeper in the body or when a more detailed view is required, computed tomography (CT) or magnetic resonance imaging (MRI) might be used.
- Blood Tests: In certain situations, blood tests might be performed to check for markers or underlying conditions associated with cysts. For instance, checking hormone levels in the case of suspected ovarian cysts.
- Fine Needle Aspiration (FNA): Using a thin needle, a sample of the cyst’s content might be drawn out. This can help in confirming its nature and ruling out other conditions, like tumors.
- Biopsy: In cases where there’s a suspicion of malignancy, a tissue sample might be taken from the cyst for microscopic examination.
- Laparoscopy: For cysts within the abdomen, like ovarian cysts, a laparoscope can be used to directly visualize and possibly remove the cyst.
The specific diagnostic approach will depend on the suspected type of cyst and its location. Early diagnosis and appropriate management are crucial, especially if there’s any suspicion of malignancy or if the cyst causes significant discomfort or complications.
What is an Abscess?
Abscesses are localized accumulations of pus that may appear anywhere on the body. Pus is a thick, yellowish or greenish fluid that consists of dead white blood cells, bacteria, tissue debris, and other substances. Abscesses are typically the body’s response to infection, inflammation, or the presence of foreign materials.

Key characteristics of an abscess include:
- Pain and Swelling: Abscesses often cause pain, tenderness, and noticeable swelling in the affected area. The skin over the abscess may appear red and warm to the touch.
- Pus Formation: As the immune system tries to fight off infection, it can create a pocket of pus. This pus can be thick and may eventually come to the surface, sometimes through a visible “head” or opening in the skin. If the abscess does not naturally drain, medical intervention may be needed to facilitate drainage.
- Infection: Most abscesses are caused by bacterial infections. The body’s immune response is to isolate the infection and create the abscess to prevent the spread of bacteria to other parts of the body.
- Fever and Malaise: Systemic symptoms like fever, chills, and a general feeling of being unwell (malaise) can accompany an abscess, especially if the infection is severe or has spread.
Abscesses can occur in various parts of the body, including:
- Skin: Skin abscesses are the most common type and can occur anywhere on the body. They are often the result of infected hair follicles or minor cuts and scrapes.
- Dental: Dental abscesses can develop from infected teeth or gums and are often associated with severe toothache and facial swelling.
- Internal Organs: Abscesses can also form in internal organs, such as the liver, lungs, or brain, due to infections or other underlying medical conditions.
Treatment for an abscess typically involves draining the pus, which can be done through a procedure performed by a healthcare provider. Antibiotics may also be prescribed to treat the underlying infection. In some cases, surgical intervention may be necessary to completely remove the abscess or address the underlying cause. Prompt treatment is important to prevent the infection from spreading and causing more serious health issues.
Common Types of Abscesses
Abscesses can develop in various parts of the body, and they are often named based on their location or the underlying cause. Here are some common types of abscesses:
- Skin Abscess: Skin abscesses are the most common type. They can occur anywhere on the body and are often the result of infected hair follicles, minor cuts, insect bites, or blocked sweat glands. These abscesses are typically painful, swollen, and may have a visible “head” where pus collects.
- Dental Abscess: Dental abscesses occur in the mouth and are usually related to infected teeth or gums. They can be further categorized into:
- Periapical Abscess: This type of dental abscess forms at the tip of the tooth’s root due to an infection in the tooth’s pulp (innermost part).
- Periodontal Abscess: This type of abscess develops in the gums, often as a result of gum disease or a foreign object (e.g., popcorn kernel) lodged between the teeth and gums.
- Peritonsillar Abscess: This abscess develops in the tissues surrounding the tonsils in the throat. It can cause severe sore throat, difficulty swallowing, and fever.
- Bartholin’s Abscess: Bartholin’s glands are located near the vaginal opening and secrete fluid to lubricate the vagina. If one of these ducts becomes blocked and infected, it can lead to a Bartholin’s abscess. This type of abscess can cause pain and swelling in the genital area.
- Breast Abscess: Breast abscesses are typically seen in breastfeeding women and can develop when bacteria enter the breast tissue through a cracked or sore nipple. They are often painful and can cause redness and warmth in the affected breast.
- Liver Abscess: Liver abscesses are pockets of pus in the liver and are usually the result of bacterial infection or the spread of infection from another part of the body. They can cause abdominal pain, fever, and other symptoms.
- Lung Abscess: Lung abscesses are rare but serious. They are often caused by aspiration of foreign material or by bacterial infections such as pneumonia. Symptoms can include cough, chest pain, fever, and difficulty breathing.
- Brain Abscess: Brain abscesses are a very serious type of abscess that occurs within brain tissue. They are typically caused by bacteria or fungi and can lead to neurological symptoms like headache, seizures, and altered consciousness.
- Spinal Abscess: Spinal abscesses occur in the spinal cord or the tissues around it. They can cause severe back pain, weakness, and neurological symptoms.
- Anal or Rectal Abscess: These abscesses occur around the anus or rectum and are often associated with pain, swelling, and sometimes fever. They can develop as a result of infection in anal glands or tears in the anal lining.
It’s important to seek medical attention if you suspect you have an abscess, as they often require drainage and treatment with antibiotics or other appropriate therapies. Left untreated, abscesses can lead to complications and more serious health issues.
Symptoms and Treatment
The symptoms and treatment of an abscess can vary depending on the location and severity of the abscess. There are some common symptoms associated with abscesses and general principles of treatment. Here’s an overview:
Common Symptoms of an Abscess:
- Pain: Abscesses are typically painful, and the level of pain can vary from mild to severe.
- Swelling: The area around the abscess is often swollen and may feel warm to the touch.
- Redness: The skin over the abscess may appear red.
- Pus Drainage: In some cases, an abscess may have a visible “head” or opening where pus drains out. This can relieve some of the pressure and pain.
- Fever: Systemic symptoms like fever, chills, and a general feeling of being unwell (malaise) may accompany an abscess, especially if the infection is severe or has spread.
Treatment of an Abscess:
- Drainage: The primary treatment for most abscesses is drainage. This can be done through several methods, including:
- Incision and Drainage (I&D): A healthcare provider makes a small incision in the abscess, allowing pus to drain out. This is often done after the area is numbed with a local anesthetic.
- Needle Aspiration: For some small abscesses, a needle may be used to withdraw the pus.
- Catheter Drainage: In some cases, especially for deep-seated abscesses, a catheter may be inserted to continuously drain the pus until the abscess resolves.
- Antibiotics: Depending on the type and severity of the infection, your healthcare provider may prescribe antibiotics. Antibiotics are typically used in cases where there is a risk of the infection spreading to other parts of the body or when there are systemic symptoms like fever.
- Pain Management: Over-the-counter pain relievers or prescription pain medications may be recommended to manage pain and discomfort.
- Warm Compresses: Applying warm compresses to the abscess can help promote drainage and alleviate some of the discomfort.
- Avoid Squeezing: It’s important not to try to squeeze or “pop” an abscess at home, as this can lead to complications, including the spread of infection.
- Underlying Cause: Treating the underlying cause of the abscess is essential. For example, if a dental abscess is caused by an infected tooth, dental treatment (e.g., root canal or tooth extraction) may be necessary.
- Follow-Up: It’s crucial to follow up with your healthcare provider to ensure that the abscess is healing properly and to monitor for any signs of recurrence or complications.
In some cases, especially with deeper or internal abscesses, surgical intervention may be required to completely remove the abscess or address the underlying cause. The specific treatment approach will depend on the location and severity of the abscess and your overall health.
If you suspect you have an abscess or are experiencing symptoms, it’s important to seek prompt medical attention. Delaying treatment can lead to the abscess worsening or complications arising.
Comparison Table of Cyst and Abscess
Cysts and abscesses are both types of lumps or swellings that can occur in the body, but they have distinct differences in terms of their causes, characteristics, and treatments. Here’s a comparison table outlining the key differences between cysts and abscesses:
| Characteristic | Cyst | Abscess |
|---|---|---|
| Definition | A cyst is a sac-like pocket filled with fluid, air, or other materials. Cysts are typically non-infectious | An abscess is a localized collection of pus caused by infection or other inflammatory processes. |
| Cause | Cysts can form for various reasons, including blocked ducts, genetic factors, or as a response to irritation or injury. | Abscesses are typically caused by bacterial infection, often due to the body’s immune response to infection, injury, or foreign material. |
| Contents | Cysts can contain fluid, air, semi-solid material, or even tissue. | Abscesses contain pus, which is a thick, yellowish or greenish fluid composed of dead white blood cells, bacteria, and tissue debris. |
| Infection | Cysts are usually not associated with infection. | Abscesses are almost always associated with infection, either bacterial or fungal. |
| Pain and Inflammation | Cysts are generally not painful unless they become very large or cause pressure on surrounding tissues. | Abscesses are typically painful, swollen, and may be accompanied by redness and warmth in the affected redness and warmth in the affected area. |
| Treatment | Treatment of cysts may involve drainage, removal, or observation depending on their type and location. | Treatment of abscesses usually involves drainage, antibiotics (if infection is present), and addressing the underlying cause (e.g., tooth extraction for a dental abscess). |
| Recurrence | Cysts can recur if not entirely removed, but they are less likely to return compared to abscesses. | Abscesses may recur if the underlying infection or cause is not adequately treated. |
Both cysts and abscesses can vary in size and location, and a healthcare provider is often needed to accurately diagnose and determine the appropriate treatment for these conditions. Additionally, while cysts are typically non-infectious, they can become infected, at which point they may display some characteristics similar to abscesses.
Risk Factors and Prevention
The risk factors and prevention strategies for cysts and abscesses can vary depending on the underlying causes and locations of these conditions. Here are some general considerations for both:
Risk Factors for Cysts:
- Age and Gender: Certain types of cysts, such as ovarian cysts, are more common in women of reproductive age.
- Genetics: Some cysts, such as sebaceous cysts, can have a genetic component, meaning they may run in families.
- Obstruction of Ducts: Cysts can form when ducts in the body become blocked, so any condition or activity that increases the likelihood of duct blockage can be a risk factor.
- Injury or Irritation: Trauma or irritation to the skin or tissues can sometimes trigger the development of cysts.
- Hormonal Changes: Hormonal fluctuations, as seen in polycystic ovary syndrome (PCOS), can contribute to cyst formation.
Prevention of Cysts:
- Good Hygiene: For skin cysts, maintaining good hygiene and avoiding excessive use of oily or greasy products on the skin may help prevent some types of cysts.
- Regular Health Check-ups: Regular check-ups with a healthcare provider can help identify and manage underlying conditions that may increase the risk of cysts.
- Hormone Management: In cases where hormonal imbalances contribute to cyst formation (e.g., PCOS), hormone therapy or lifestyle changes may be recommended by a healthcare provider.
Risk Factors for Abscesses:
- Bacterial or Fungal Infections: The primary risk factor for abscesses is exposure to bacteria or fungi that can cause infections. This can happen through cuts, wounds, injuries, or other means.
- Poor Immune Function: Individuals with weakened immune systems, due to conditions like HIV/AIDS or certain medications, are at greater risk of developing abscesses.
- Chronic Illnesses: People with chronic medical conditions such as diabetes, Crohn’s disease, or rheumatoid arthritis may be more susceptible to abscesses.
Prevention of Abscesses:
- Wound Care: Properly clean and care for wounds, cuts, and injuries to minimize the risk of infection. Keep wounds clean, cover them with a sterile bandage, and seek medical attention for deep or puncture wounds.
- Hygiene: Maintain good personal hygiene to reduce the risk of skin infections. Regular handwashing and keeping skin clean and dry are important.
- Immune Health: Take steps to support a healthy immune system through a balanced diet, regular exercise, adequate sleep, and minimizing stress.
- Chronic Disease Management: If you have a chronic medical condition that affects your immune system, work closely with your healthcare provider to manage it effectively.
- Dental Health: Good oral hygiene, including regular dental check-ups, can help prevent dental abscesses.
- Safe Sex: Practicing safe sex can reduce the risk of sexually transmitted infections that may lead to abscesses.
Some abscesses, especially those caused by bacterial infections, can develop suddenly and may not always be preventable. In such cases, prompt medical attention is crucial to prevent complications and ensure proper treatment. If you have concerns about cysts or abscesses or are at risk due to underlying conditions, consult with a healthcare provider for personalized guidance and recommendations.
Conclusion
Cysts and Abscesses are both common medical conditions that involve the formation of localized lumps or swellings in the body. Cysts are typically fluid-filled sacs that can form for various reasons, including genetic factors or blocked ducts. They are often non-infectious and may not always require treatment. On the other hand, abscesses are collections of pus caused by infections, usually bacterial or fungal, and they are almost always associated with pain, redness, and swelling.
Prompt medical attention is essential for abscesses, as they require drainage and treatment with antibiotics to prevent complications. Understanding the differences between these two conditions and their respective risk factors and prevention strategies can help individuals better manage their health.